To the Editor,
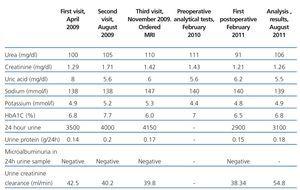
We present the case of a female patient aged 71 years who was referred to our diabetic nephropathy department in April 2009. Her relevant medical history included high blood pressure and type 2 diabetes mellitus (DM2) for more than 20 years, with various diabetes-related complications (diabetic retinopathy); hyperuricaemia, dyslipidaemia, history of occasional treatment with non-steroidal anti-inflammatory agents, 7 pregnancies with 7 deliveries and no gestosis. Clinical measurements only revealed single-episode nocturia and significant loss of visual acuity in the right eye. Physical examination was normal: blood pressure 120/60mm Hg, weight 72.3kg and height 1.57m. The patient was being treated with alprazolam, furosemide, carvedilol, valsartan, calcium dobesilate and pravastatin. The patient provided an echocardiogram reading that showed moderate left ventricular hypertrophy, ejection fraction of 80% and grade I diastolic dysfunction. She also provided results from an analysis performed by her health centre (Table 1).
On her second visit in August 2009, she only provided analysis results from June 2009 (Table 1). In November 2009 on her third visit, the patient provided a more recent analytical test (Table 1) and an abdominal ultrasound, which showed a right kidney measuring 9.7cm and a left kidney measuring 9.4cm. Both presented good cortical/medullary differentiation. The patient stated that she had not brought the entire 24 hour urine output sample but that she did not have polydipsia. Since the patient presented hypernatraemia and polyuria, we requested a cerebral MRI without gadolinium. This test, evaluated in January 2010, showed a rounded expanding mass measuring 4cm compatible with parasagittal parietal meningioma in the right convexity, with no perilesional oedema and preserved meningeal grooves. The patient was referred to the neurosurgery division and underwent medial craniotomy in April 2010 to remove bone infiltrated by tumour cells and have it replaced with a titanium mesh. Diagnosis based on histological results was WHO grade I fibrous meningioma with focal bone infiltration. After being referred to the neurosurgery division, the patient did not make follow-up visits until she came in for an appointment in February 2011 in good general health and with improved visual acuity in the right eye. Her most recent evaluation was in August 2011; the patient remained asymptomatic, with no dysnatraemia and a slightly improved glomerular filtration rate (Table 1).
To resume, the patient had stage 3 chronic kidney disease (CKD), probably secondary to nephroangiosclerosis. On a single occasion during her follow-up period she presented with hypernatraemia, polyuria and euvolaemia, which led to a diagnosis of meningioma, and the tumour was subsequently resected. The differential diagnosis focused on the presence of hypernatraemia with normal total sodium levels. This would also include differential diagnosis for central diabetes insipidus or partial diabetes insipidus with hypodipsia.1 The absence of polydipsia almost ruled out the diagnoses of diabetes insipidus or primary polydipsia.1
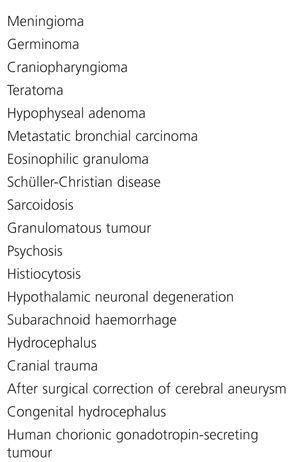
Hypodipsia-hyponatraemia syndrome is characterised by persistent hypernatraemia that cannot be explained by loss of volume, absence of thirst, partial diabetes insipidus, and normal renal response to vasopresin.2 Causes related to this syndrome are listed in Table 2. Its physiopathology seems to be related to an osmoreceptor disorder that makes these patients dilute and concentrate urine at inappropriately high levels of plasma osmolality.3
The most frequent type of dysnatraemia in patients with CRF and type 2 DM is pseudohyponatraemia secondary to hyperglycaemia or hypertriglyceridaemia; in CFR patients, hyponatraemia is usually much more common than hypernatraemia.4-5 For that reason, in a patient with CRF and type 2 DM the presence of hypernatraemia, even on a single occasion, requires assessment and a differential diagnosis. The absence of polydipsia made us suspect the presence of hypodipsia-hypernatraemia syndrome, and we were able to identify and correct its cause.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Table 1. Evolution of patient¿s laboratory data
Table 2. Causes of hypernatraemia syndrome with hypodipsia