There is no consensus on the most appropriate treatment for chronic active antibody-mediated rejection (cAMR). Recent studies suggest that treatment with tocilizumab (TCZ) may stabilize graft function, decrease the intensity of donor-specific HLA antibodies (DSAs) and reduce inflammation of microcirculation.
Patients and methodsObservational study with renal allograft recipients diagnosed with cAMR (n = 5) who had not submitted a response to traditional treatment based on the combination of plasma replacements, immunoglobulins, and rituximab. Patients were told to be treated with TCZ as compassionate use in six doses per month (8 mg/kg/month). Renal function, proteinuria, and the intensity of DSAs were monitored during follow-up.
ResultsFive patients, average age 60 ± 13 years, three male and two retrasplants (cPRA average 55%) with preformed DSAs. Treatment with TCZ was initiated within 47 ± 52 days of biopsy. In two cases treatment was discontinued after the first dose, by severe bicitopenia with cytomegalovirus viremia and by graft failure, respectively. In the three patients who completed treatment, no stability of renal function (serum creatinine from 1.73 ± 0.70 to 2.04 ± 0.52 mg/dL, e-FGR 4 6 ± 15 to 36 ± 16 mL/min), showed increased proteinuria (3.2 ± 4.0 to 6.9 ± 11.0 g/g) and the intensity of DSAs maintain stable. No changes were observed in the degree of inflammation of microcirculation (g+pt 4.2 ± 0.8 vs. 4.3 ± 1.0) or in the degree of transplant glomerulopathy (cg 1.2 ± 0.4 vs. 1.8 ± 1.0).
ConclusionsTCZ therapy does not appear to be effective in modifying the natural history of chronic active antibody-mediated rejection, does not improve the degree of inflammation of microcirculation and does not reduces the intensity of DSAs.
No existe consenso sobre el tratamiento más adecuado para el rechazo humoral crónico activo (RHCa). Estudios recientes sugieren que el tratamiento con tocilizumab (TCZ) puede estabilizar la función del injerto, disminuir la intensidad de los anticuerpos anti-HLA donante-específicos (ADEs) y reducir la inflamación de la microcirculación.
Pacientes y métodosEstudio observacional con pacientes trasplantados renales diagnosticados de RHCa (n = 5) que no habían presentado respuesta al tratamiento tradicional basado en la combinación de recambios plasmáticos, inmunoglobulinas y rituximab. A los pacientes se les indicó tratamiento con TCZ como uso compasivo en seis dosis mensuales (8 mg/kg/mes). Durante el seguimiento se monitorizó la función renal, proteinuria y la intensidad de los ADEs.
ResultadosCinco pacientes, de edad media 60 ± 13 años, tres de género masculino y dos retrasplantes (cPRA medio 55%) con ADEs preformados. El tratamiento con TCZ se inició a los 47 ± 52 días de la biopsia. En dos casos se suspendió el tratamiento tras la primera dosis, por bicitopenia severa con viremia por citomegalovirus y por fracaso del injerto, respectivamente. En los tres pacientes que completaron el tratamiento no se observó estabilidad de la función renal (creatinina sérica [Cr-s] de 1,73 ± 0,70 a 2,04 ± 0,52 mg/dL, filtrado glomerular estimado [FGRe] de 46 ± 15 a 36 ± 16 mL/min), presentaron aumento de la proteinuria (3,2 ± 4,0 a 6,9 ± 11,0 g/g) y la intensidad de los ADEs se mantuvo estable. No se observaron cambios en el grado de inflamación de la microcirculación (glomerulitis y capilaritis peritubular [g+cpt] 4,2 ± 0,8 vs. 4,3 ± 1,0), ni en el grado de glomerulopatía del trasplante (glomerulopatía crónica [cg] 1,2 ± 0,4 vs. 1,8 ± 1,0).
ConclusionesLa terapia con TCZ no parece ser eficaz en modificar la historia natural del rechazo humoral crónico activo, no mejora el grado de la inflamación de la microcirculación ni reduce la intensidad de ADEs.
Chronic active humoral rejection (c-aABMR) is one of the main causes of renal graft loss.1,2 Traditional treatment based on the combination of plasma exchanges (PE), intravenous immunoglobulins (IvIg) and rituximab (RTX) has not been shown to be effective,3 therefore new therapeutic targets are being evaluated.4
Donor-specific antibodies (DSA), T and B lymphocytes, plasma cells, and NK cells are involved in the pathophysiology of c-aABMR. The existence of preformed DSA, as well as the development of de novo DSAs, have been related to changes in microcirculation, the appearance of transplant glomerulopathy and progressive interstitial fibrosis.5,6 A systematic review of the treatments used in c-aABMR has recently been published and it is recognized that to date there is no effective treatment.7–10
In recent years, it has been shown that the proinflammatory cytokine interleukin-6 (IL-6) participates in the pathogenesis of humoral rejection, intervening in the regulation of inflammation, in the development, differentiation and activation of T cells, B cells and T cells plasmatic.11 IL-6 mediates chronic inflammation and autoimmunity,12 suggesting that it may have an effect on humoral rejection.13
Tocilizumab (TCZ) ( Actemra®, Roche/Genentech, San Francisco, CA, USA) is a humanized monoclonal antibody directed against the IL-6 receptor; used as rescue therapy in patients with c-aABMR. In 2017, Choi et al. published the first study in which TCZ was used as rescue therapy, observing stable renal function, improvement of histological lesions, and reduction of DSAs.14
We report our experience in five patients with c-aABMR, in whom TCZ was used due to lack of response to conventional treatment. Renal function, proteinuria, histology, the evolution of DSAs, and adverse events associated with treatment were monitored.
MethodsPatientsThis is a retrospective observational study including kidney transplant recipients from our center who received at least one dose of TCZ for the treatment of c-aABMR between June 2018 and January 2020. The patients included were refractory to traditional treatment. The established treatment scheme consisted in the administration of TCZ for six months (8 mg/kg/month) by intravenous infusion without premedication as an outpatient.
MethodsDuring follow-up, renal function (eGFR using the CKD-EPI formula), proteinuria (g/g), complete blood count, and liver function tests were evaluated. At the time of inclusion all patients had a kidney biopsy with the diagnosis of c-aABMR. In addition, another biopsy was performed at the end of the follow-up in those patients who completed the treatment. The evaluation of the biopsies was based on the Banff 2019 criteria.15
The presence of DSAs was determined at the time of the biopsy and at the end of the treatment. The detection of DSAs was performed with the LIFECODES Life Screen Deluxe (Gen-Probe, San Diego, CA, USA) and the threshold value to be classified as positive was a mean fluorescence intensity (MFI) >1000. For each patient, the immunodominant DSA was defined as the one with the highest MFI among all donor-specific reactivities.
ResultsDemographic and transplant-related variables are shown in Table 1. The mean age of the patients was 60 ± 13 years. The mean number of HLA mismatches at the AB loci was 3.2 ± 1.3 and at the DR locus was 1.6 ± 0.5.
Baseline characteristics of the patients.
| Case | Age | Sex | CKD | Retransplantation | Donor | cPRA total (%) | cPRA class I (%) | cPRA class II (%) | Desensitization | HLA A/B/DR mismatch |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 41 | M | Cortical necrosis | Yes | DCA III | 98 | 94 | 95 | Yes | 2/2/2 |
| 2 | 56 | M | PKD | No | Living | 0 | 0 | 0 | No | 0/1/1 |
| 3 | 59 | F | SLE | No | BD | 99 | 85 | 96 | No | 2/2/2 |
| 4 | 73 | F | SLE | No | DCA III | 0 | 0 | 0 | No | 2/2/2 |
| 5 | 73 | M | Unknown | Yes | DCA III | 82 | 0 | 82 | Yes | 2/1/1 |
cPRA: calculated PRA; DCA III: donor in controlled asystole type III; CKD chronic kidney disease; SLE: systemic lupus erythematosus; BD: brain death; PKD: polycystic hepatorenal disease.
In four patients, the induction treatment was with thymoglobulin and in the other case with basiliximab. All patients began maintenance treatment with triple therapy based on the combination of tacrolimus, mycophenolate mofetil (MMF) and prednisone.
The diagnosis of c-aABMR was made at 13.8 ± 10.5 months post-transplant, in four of the cases traditional treatment was performed. The patient who presented concomitant BK nephropathy received treatment with IvIg (2 g/kg) monthly (Fig. 1). Due to lack of clinical response, TCZ was indicated, which began 47 ± 52 days after the diagnostic biopsy. Two patients received only a single dose due to cytomegalovirus viremia (2937 copies/mL in whole blood) with bicytopenia (970 leukocytes/mm3 and 57,000 platelets/mm3) in one case and non-response in the other case (Fig. 1).
The three patients who completed the treatment did not present favorable changes in renal function (eGFR changed from 46 ± 15 to 36 ± 16 mL/min), and it was observed an increase in proteinuria from 3.2 ± 4.0 to 6.9 ± 11.0 g/g.
Fig. 2 describes the degree of histological lesion at the time of c-aABMR diagnosis, before and after treatment with TCZ. No changes were observed in the degree of inflammation of the microcirculation (g+ptc = 4.2 ± 0.8 vs. 4.3 ± 1.0, p = 0.936), nor in that of interstitial fibrosis/tubular atrophy (ci+ct 2.0 ± 1.2 vs. 2.8 ± 1.0, p = 0.351). No significant changes were observed in the degree of transplant glomerulopathy (chronic glomerulopathy [cg] 1.2 ± 0.4 vs. 1.8 ± 1.0, p = 0.287).
Case 142-year-old male, chronic kidney disease (CKD) due to neonatal cortical necrosis. He received a fifth kidney transplant in May 2018 from a brain-dead donor, in the national hypersensitivity program. A kidney transplant was performed with a negative CDC crossmatch and flow cytometry (FC) positive for B lymphocytes (SCMF 318) and weakly positive for T lymphocytes (SCMF 48) under induction with thymoglobulin and triple therapy. Due to slow recovery of renal function and detection of DSA class I (A*33:03 with MFI 6146) and class II (DPB1*04:01 MFI 2432) ADE, peritransplant desensitization (DS) with PE was started (seven sessions). Ivig (0.2 g/kg per session) and RTX (375 mg/m2) and a renal biopsy was indicated, which showed active humoral rejection (ABMR) with C4d negative. At discharge, he presented creatinine (Cr-s) of 1.5 mg/dL.
After DS, he presented a decrease in the intensity of DSAs A*33:03 (MFI 3546) and DPB1*04:01 (MFI 2900), and continued with seven PE sessions and IvIg; evidencing a decrease in A*33:03 (MFI 1224) and a negativization of DPB1*04:01.
A protocol biopsy was performed at three months (Cr-s 1.9 mg/dL and urine protein/creatinine ratio [UPCR] 500 mg/g), which showed persistence of RHa C4d negative and positivity for BK polyomavirus and treatment with IvIg was given for six months (2 g/kg/month).
Due to chronic graft dysfunction (sCr 2.3 mg/dL and UPCR 1500 mg/g), a new biopsy was performed in January 2020, which showed CAMR with negative C4d and negative DSAs. TCZ was indicated for six months (420 mg monthly), with persistence of CAMR and negative DSAs. No changes in renal function or proteinuria were observed (sCr 2.64 mg/dL and UPCR 1500 mg/g) without adverse effects. During follow-up no adverse effects were recorded.
Case 2A 56-year-old man, CKD due to hepatorenal polycystic disease, kidney transplant in February 2017 from a haploidentical living donor, with negative CDC and CF crossmatch, induction with basiliximab and triple therapy. At discharge, he presented serum Cr 1.0 mg/dL. In May 2017, MMF was discontinued, and rapamycin was started for non-melanocytic skin carcinoma.
In July 2018, a biopsy was performed due to acute deterioration of renal function (serum Cr 1.5 mg/dL), which showed RHa, C4d negative and DSA de novo (B*35:08 with MFI 1.404). He underwent treatment with PE (seven sessions), IvIg and RTX (1000 mg) and DSA became negative.
In June 2019, a new biopsy was performed due to chronic dysfunction (serum Cr 2.22 mg/dL, UPCR 210 mg/g), which showed CAMR with C4d negative, without DSA s. TCZ was indicated for six months (640 mg/monthly), and after its completion showed persistence of the CAMR without the presence of DSA s. Renal function remained stable (Cr-s 1.57 and UPCR 200 mg/g) and no adverse effects were observed.
Case 3A 59-year-old woman with CKD secondary to lupus nephropathy. She received a first kidney transplant in October 2017, from a brain-dead donor. With negative CDC crossmatch and CF weakly positive for B lymphocytes (SCMF 235). She received induction with thymoglobulin and triple therapy. She presented class II DSAs (DQB1*05:01 with MFI 2900), but due to adequate evolution, it was maintained an expectant attitude. In May 2018, a renal biopsy was performed due to proteinuria (UPCR 3000 mg/g), which showed CAMR with C4d negative, and IgG, IgA and IgM deposits by immunofluorescence, without criteria of lupus activity (ANA titers 1/80, anti-DNA <12 IU/, RF 8.5 IU/mL). Due to an increase in DSAs (DQB1*05:01 with MFI 3800), treatment with PE (seven sessions), IvIg and RTX (1000 mg) was indicated. In February 2019, a new biopsy was performed due to proteinuria, and it was observed persistence of CAMR. TCZ treatment was prescribed for six months (400 mg/monthly). In May 2020, due to chronic dysfunction, a biopsy was performed that showed CAMR with stage V lupus nephritis without evidence of DSAs. During the treatment the patient did not present adverse effects.
Case 4A 73-year-old woman, CKD due to secondary focal and segmental glomerulosclerosis, received a kidney transplant in August 2018 from a donor in controlled asystole. With negative CDC, CF and virtual crossmatch; received induction with thymoglobulin and triple therapy with good evolution (serum Cr of 1.3 mg/dL). After 15 days, acute renal dysfunction (serum Cr 2.2 mg/dL) prompted the execution of biopsy that showed signs of mixed rejection (grade IIa and CAMR rejection), with anti-HLA and non-anti-HLA antibodies (MICA and GSTT) being negative. She received treatment with three pulses of methylpredsnisolone, thymoglobulin, PE (seven sessions), IvIg and RTX (500 mg), presenting at discharge a Cr of 0.9 mg/dL.
In October 2018, a biopsy was performed due to proteinuria (UPCR 8000 mg/g), with normal renal function. The biopsy showed CAMR rejection with negative C4d and negative ADEs. TCZ was indicated (480 mg/month), receiving only one dose for pancytopenia and CMV viremia (3.7 log). Treatment with valganciclovir was indicated and MMF was changed by rapamycin. During follow-up, a new biopsy was performed due to nephrotic proteinuria, which showed persistent CAMR with stable renal function (Cr-s 1.2 mg/g).
Case 5He is a 73-year-old male with CKD of unknown etiology. Recipient of a second kidney transplant in March 2018 from a donor in controlled asystole. With negative crossmatch for CDC and CF; induction with thymoglobulin and triple therapy. Due to the slow recovery of renal function and the presence of anti-DP antibodies, the HLA typing of the donor was expanded, observing ADE DPB1*01:01 (MFI of 22,000). A DS peri transplant with immunoadsorption (IA) (five sessions) and IvIg was indicated, and a renal biopsy was performed that showed signs of CAMR with C4d positive. Due to refractoriness to treatment and persistence of DSAs, up to 10 AI sessions with IvIg and RTX were performed (700 mg). Due to chronic dysfunction and proteinuria (serum Cr 4.4 mg/dL and UPCR 900 mg/g), a renal biopsy was performed that showed CAMR with negative C4d and a slight decrease in ADE DPB1*01:01 (MFI 9456). TCZ was indicated (600 mg/monthly), receiving only one dose due to graft failure.
DiscussionThe present study includes five renal transplant recipients with a diagnosis of CAMR, who did not respond to traditional treatment. The histology of the biopsies before the treatment with TCZ showed a high degree of inflammation of the microcirculation and chronic lesions. At the end of the treatment, no improvement was observed in the clinical variables, renal function and proteinuria, nor in the histological and immunological parameters. We have not observed serious adverse effects associated with the treatment, however, one case developed severe bicytopenia.
In our series, the lack of response to traditional treatment is consistent with the results of a recent multicenter trial aimed at evaluating the efficacy and safety of IvIg combined with RTX. In this study, the treatment and the placebo groups did not show differences in the evolution of glomerular filtration rate, proteinuria, and histological lesions.8 This failure of traditional treatment has led to various clinical trials aimed at evaluating new therapeutic strategies. The BORTEJECT clinical trial, in which the proteasome inhibitor bortezomib was compared to placebo in patients with AMR or CAMR, showed no changes in the evolution of renal function, histological lesions or ADEs. Instead, a high rate of haematological toxicity was described.9 However, positive results have been observed with daratumumab (an anti-CD38 monoclonal antibody that induces central and peripheral depletion of plasma cells and NK cells), with negativization of DSAs.16
In 2015, Vo et al. reported the results of a clinical trial using TCZ and IvIg in patients with calculated panel reactive antibodies (cPRA) ≥50%, who did not respond to their pre-transplant desensitizing treatment regimen with IvIg and RTX. Five of the 10 patients included in the study underwent transplantation, observing a decrease in the intensity of the DSAs. Histological monitoring at six months showed no signs of humoral rejection, suggesting that TCZ may be effective as a desensitizing treatment.17
Following these results, Choi et al. conducted a study in 36 patients diagnosed with CAMR who did not respond to traditional treatment. The results of this study showed stability of renal function at 36 months and a significant decrease in the intensity of DSAs. In nine of the 36 cases in which a protocol biopsy was performed at one year, it was observed a decreased inflammation of the microcirculation. It is noteworthy that no serious adverse effects were observed.14 In another study, which included seven cases, stable renal function was observed together with a decrease in DSAs, although only three patients received the complete treatment scheme due to infectious and neoplastic processes and/or adverse reactions.18
Recently, Massat et al. published a study that included nine patients with CAMR treated with TCZ after failure of traditional treatment, and they were compared with a historical cohort of 37 patients. Both groups presented similar clinical, immunological and histological characteristics. No differences were observed in graft survival, the evolution of renal function, and the intensity of DSAs between the two groups. In seven patients with histological follow-up by paired biopsies, no changes were observed in the inflammation of the microcirculation or in the degree of glomerulopathy.19 Similarly, in the study by Kumar et al. it could not be observed any efficacy of treatment with TCZ in 10 patients diagnosed with CAMR who presented a high degree of inflammation of the microcirculation (g+ptc 4.8 ± 1.4) and chronic damage (ci+ct 2.5 ± 0.8).20
The previously described results contrast with those of a clinical trial that evaluated the usefulness of clazakizumab (a monoclonal antibody against IL-6) in 20 patients with CAMR. In the first phase, the patients were randomized to a placebo arm and a treatment arm for 12 weeks. In the second phase, all patients received clazakizumab for 40 weeks. It was observed a retardation in the progression of renal dysfunction and a decrease in DSAs. At the histological level, there was an improvement in the inflammation of the microcirculation, and a reversion of the phenotype of active AMR to inactive AMR.21
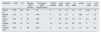
Table 2 shows the evolution of renal function and histological lesions in paired biopsies from the different studies mentioned. In those studies with high microcirculatory inflammation and advanced signs of interstitial fibrosis/tubular atrophy prior to TCZ treatment, there was no response to treatment. It is noteworthy that the study by Choi et al.,14 who reported stable renal function, had a lower degree of histological lesion at the start of treatment.
Evolution of glomerular filtration and histological lesions in studies with paired biopsies before and after TCZ.
| Reference | Drug | No | Baseline eGFR (mL/min) | Decrease in eGFR (mL/min/month) | Paired biopsies | g+cpt basal | g+cpt final | cg basal | cg final | ic+ct basal | ci+ct final |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Choi et al.14 | TCZ | 36 | 36 | ≈0 | 9 | 1.8 | 1.0 | 1.5 | 1.4 | 0.93 | 1.4 |
| Massat et al.19 | TCZ | 9 | 40 | 0.49 | 7 | 3.0 | 2.5 | 1.1 | 0.98 | 1.5 | 3.0 |
| Kumar et al.20 | TCZ | 10 | 42 | 0.33 | 6 | 4.8 | 4.2 | 1.8 | 2.4 | 2.5 | 3.3 |
| Doberer et al.21 | CKZ | 20 | 39 | 0.29 | 18 | 3.8 | 2.8 | 2.5 | 2.5 | 3 | 4 |
| Chamon et al.a | TCZ | 5 | 46 | 0.62 | 4 | 4.2 | 4.3 | 1,2 | 1.8 | 2.0 | 2.8 |
CKZ: clazakizumab; cg: chronic glomerulopathy; ci+ct: interstitial fibrosis/tubular atrophy; g+cpt: glomerulitis and peritubular capillaritis; eGFR: estimated glomerular filtration rate; TCZ: tocilizumab.
In summary, we report an uncontrolled study with a small series of patients diagnosed with CAMR with a high degree of inflammation of the microcirculation and advanced signs of chronicity who have not responded to treatment with TCZ. These data, together with the review of previous studies, suggest that it is necessary to design clinical trials that include patients in the initial stages of the disease.
Key conceptsChronic active humoral rejection is one of the leading causes of renal allograft failure, which has been well characterized from the histological and immunological point of view over the last 15 years.
Currently, there are no approved drugs for the treatment of chronic active humoral rejection, since there are only a limited number of prospective and randomized clinical trials performed. Treatment with the combination of rituximab and intravenous immunoglobulins, as well as treatment with proteasome inhibitors (bortezomib) have not shown effectiveness.
Blockade of the interlekin-6 signal and its receptor have shown promising results in a prospective clinical trial randomized with clazakizumab and in a case series with tocilizumab.
In our series of cases with severe inflammation of the microcirculation, we did not observe that a six month treatment with tocilizumab modified the evolution of renal function, the intensity of donor-specific antibodies, or the histological features.
It is necessary to perform new clinical trials in a larger sample size to assess whether the blockade of the interleukin-6 signal and its receptor can modify the natural history of active chronic humoral rejection, and in which stages of the disease the treatment can be effective.
Conflicts of interestThe authors declare the following conflict of interest: BC has a pre-doctoral fellowship from the Vall d’Hebron Research Institute(VHIR).