The 2021 guidelines on the prevention of vascular disease (VD) in clinical practice published by the European Society of Cardiology (ESC) and supported by 13 other European scientific societies recognize the key role of screening for chronic kidney disease (CKD) in the prevention of VD. Vascular risk in CKD is categorized based on measurements of estimated glomerular filtration rate (eGFR) and urine albumin to creatinine ratio (ACR). Thus, moderate CKD is associated with a high vascular risk and severe CKD with a very high vascular risk requiring therapeutic action, and there is no need to apply other vascular risk scores when vascular risk is already very high due to CKD. Moreover, the ESC indicates that vascular risk assessment and the subsequent decision algorithm should start with measurement of eGFR and ACR. To optimize the implementation of the ESC 2021 guidelines on the prevention of CVD in Spain, we consider that: 1) Urine testing for albuminuria using ACR should be part of the clinical routine at the same level as blood glucose, cholesterolemia, and GFR estimation when these are used to make decisions on CVD risk. 2) Spanish public and private health services should have the necessary means and resources to optimally implement the ESC 2021 guidelines for the prevention of CVD in Spain, including ACR testing.
Las guías 2021 sobre la prevención de la enfermedad vascular (EV) en la práctica clínica publicadas por la European Society of Cardiology (ESC) y apoyadas por otras 13 Sociedades científicas europeas, reconocen el papel clave de la detección de la enfermedad renal crónica (ERC) en la prevención de la EV. El riesgo vascular en la ERC se categoriza a partir de las medidas del filtrado glomerular estimado (FGe) y del cociente albúmina:creatinina en orina (ACRo). Así, la ERC moderada se asocia a un riesgo vascular alto y la ERC grave a un riesgo vascular muy alto, debiendo actuar en consecuencia desde el punto de vista terapéutico y no siendo necesario aplicar otras puntuaciones de riesgo vascular cuando este ya es muy alto debido a la ERC. Es más, la ESC sitúa la medida del FGe y del ACRo en el inicio de la estimación del riesgo vascular y del algoritmo de decisión subsiguiente. A fin de optimizar la implementación de la guía 2021 de la ESC sobre la prevención de la EV en España, consideramos que: 1) El estudio de la orina para determinar la albuminuria mediante el ACRo debería formar parte de la rutina clínica al mismo nivel que las de la glucemia, la colesterolemia y la estimación del FG cuando estas se usan para tomar decisiones sobre el riesgo de EV. 2) Los servicios de salud públicos y privados españoles deberían disponer de los medios y recursos necesarios para implementar de forma óptima las Guías ESC 2021 de prevención de la EV en España, incluyendo la determinación del ACRo.
In 2021, diseases of the circulatory system caused 119,196 deaths in Spain, representing 26.4% of all deaths and placing them as the leading cause of mortality.1 Prevention remains the cornerstone of the fight against vascular disease (CVD). In August 2021, the European Society of Cardiology updated the "Guidelines on cardiovascular disease prevention in clinical practice.”2,3 The document was supported by 13 other European scientific societies, including the European Association for the Study of Diabetes; the European Atherosclerosis Society; the European Renal Association; the European Society of Hypertension; the European Stroke Organization; the European Geriatric Medicine Society; the World Organization of National Colleges, Academies and Academic Associations of General Practitioners/Family Physicians-Europe, among others. The guidelines recognize the key role of early detection of chronic kidney disease (CKD) in the prevention of CVD.
Table 3 of the document highlights the novelties compared to the 2013 guidelines. Among the class 1 novelties, moderate or severe CKD is considered at the same level as established CVD, diabetes mellitus (DM), and familial hypercholesterolemia, as a condition that automatically confers a high or very high CVD risk. When the risk is already very high, there is no need for further stratify risk based on scores such as SCORE2 or SCORE2-OP, regardless of age. Recently, the European Renal Association has highlighted the significance and implications for clinical practice of including CKD among the diseases to be detected to optimize CKD prevention.4,5 Specifically, the ESC recommendations imply the need to measure serum creatinine to estimate glomerular filtration rate (eGFR), but also the albumin:creatinine ratio in a single urine sample (uACR) in any person in whom the risk of CVD is to be assessed. The ESC 2021 guidelines on the prevention of VD in clinical practice also provides guidance on who should be assessed for VD risk (Table 1) In its broader version, it states that systematic or opportunistic vascular risk assessment (which includes measuring uACR) should be considered in the general population in men>40 years and in women>50 years or who are postmenopausal.
Recommendations for vascular disease (VD) risk assessment according to the 2021 ESC guidelines for the prevention of VD (2).
| Recommendations | Class | Level |
|---|---|---|
| An overall systematic evaluation of the risk of VD is recommended in individuals with any major vascular risk factor (i.e., family history of premature VD, familial hypercholesterolemia, VD risk factors such as smoking, hypertension, DM, elevated lipid levels, obesity or comorbidities that increase the risk of VD). | I | C |
| Systematic or opportunistic VD risk assessment may be considered in the general population in men > 40 years and in women > 50 years or postmenopausal women with no known risk factors for atherosclerotic VD. | IIb | C |
| In those individuals who have undergone a VD risk assessment in the context of opportunistic screening, a repeat screening may be considered after 5 years (or sooner if the risk was close to treatment thresholds) | IIb | C |
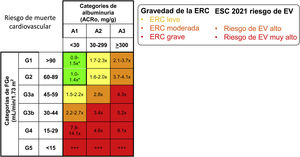
Kidney Disease: Improving Global Outcomes (KDIGO) defines CKD as abnormalities of kidney structure or function, present for more than 3 months, with health implications.6,7 Among the health implications of CKD, KDIGO focuses on the elevated risk of death from any cause, including vascular etiology, progression of CKD to eventually requiring renal function replacement, and acute renal failure. The specific criteria that, on their own, allow the diagnosis of CKD are the presence of eGFR < 60 mL/min/1.73 m2, evidence of renal damage identified by the presence of albuminuria (uACR ≥ 30 mg/g), urinary sediment, electrolyte and other abnormalities due to tubular disorders, alterations detected by histology, structural disorders objectified by imaging methods or a history of renal transplantation. In clinical practice, CKD is diagnosed if uACR is ≥30 mg/g, even if eGFR is ≥60 mL/min/1.73 m2. KDIGO also recognizes three categories of health risk in people already diagnosed with CKD, defined by ranges of eGFR and uACR. Even though there is an international categorization of CKD according to KDIGO into 1, 2, 3a and 3b, 4, and 5, the ESC 2021 guidelines have used the very intuitive terms mild, moderate, and severe CKD to identify the KDIGO risk categories, considering a high VD risk for moderate CKD and very high for severe CKD2–5 (Fig. 2).
Chronic kidney disease in the ESC 2021 guideline on vascular disease preventionThe 2021 ESC guidelines on the prevention of VD indicate that individuals should be categorized into 5 baseline risk situations for VD (Fig. 1), to correctly stratify risk and to address specific measures for follow-up and prevention of VD. A history of atherosclerotic disease, DM, familial hypercholesterolemia, or CKD implies a high or very high risk of VD (Fig. 3A).2 Once these situations have been ruled out, the guidelines consider the person to be healthy, which implies that the risk of VD in the next 10 years should be calculated using scores such as SCORE2 for people younger than 70 years and SCORE2-OP for people aged 70 years or older.
Equivalence between chronic kidney disease (CKD) severity and vascular disease (VD) risk classes defined by the European Society of Cardiology (ESC) in its 2021 guidelines for the prevention of VD. Cell numbers represent the risk of vascular death according to KDIGO. Modified from references Ortiz et al.,4,5 using additional information from KDIGO.7
* Risk is >1.1 when ACRo has values between 10 and 29 mg/g.
Categories of individuals in whom an intervention to prevent the risk of VD should be considered according to the 2021 European Society of Cardiology guidelines on prevention of VD. Taken from Visseren et al.2 B) Algorithm that translates Fig. 2 of the ESC 2021 guidelines into concrete actions in clinical practice.
ASCVD: atherosclerotic vascular disease; CKD: chronic kidney disease; DM: diabetes mellitus; CKD: chronic kidney disease; CVD: atherosclerotic vascular disease; FH: familial hypercholesterolemia; HC: familial hypercholesterolemia; TOD: target organ damage.
Diagnoses of DM, familial hypercholesterolemia, or CKD may already appear in the clinical history or be obvious because they have been treated previously (Fig. 3B). However, CKD may still go unnoticed. In a recent Swedish study, among almost 60,000 people diagnosed with CKD for having an eGFR persistently below 60 mL/min/1.73 m2, only 20% had a diagnosis of CKD recorded in their medical records: a diagnosis of CKD was less frequent than a diagnosis of cancer or DM in these same patients.8,9 If the diagnoses of DM, hypercholesterolemia, or CKD do not appear in the clinical history, they can be ruled out by blood (cholesterol, glycemia, creatinine) and urine (uACR) tests (Fig. 3B). Although the presence of cholesterol, glycemia, and creatinine in routine analyses is almost universal, there is still a long way to go for uACR to be studied in periodic health check-ups in primary care or in employment-based clinics, or in people with other diseases followed up in these settings or by specialists.
A diagnosis of CKD requires specific actions for preventing VD, such as achieving optimal blood pressure figures and considering the prescription of hypolipidemic agents or sodium-glucose cotransporter type 2 (SGLT2) inhibitors, among other possible actions,2 in addition to a study of the etiology and the adjustment or suspension of drugs with potential nephrotoxicity.3,4,10 This is currently a dynamic field which is evolving rapidly based on the results of large clinical trials.11–14
Implementation of the ESC 2021 Guidelines for the prevention of CVD in Spain: screening of chronic kidney disease by quantifying albuminuria using the uACRIn Spain, it is estimated that more than 15% of adults have CKD, and the majority are undiagnosed.15 Spanish society can benefit from the implementation of the ESC 2021 guidelines for the prevention of CVD. Specifically, with respect to CKD:
- 1.
Urine testing for albuminuria by uACR should be part of the clinical routine at the same level as blood glucose, cholesterolemia and eGFR estimation when these are used to make decisions about VD risk.16
- 2.
Spanish public and private health services, including employer-based clinics, should have the necessary means and resources to optimally implement the ESC 2021 guidelines for the prevention of VD in Spain, including uACR.
The research of Alberto Ortiz and Patricia de Sequera is funded by the Instituto de Salud Carlos III (ISCIII) RICORS program to RICORS2040 (RD21/0005/0001) funded byEuropean Union– NextGenerationEU, Mechanism for Recovery and Resilience (MRR), FEDERfunds.
Conflict of interestThe authors have no conflicts of interest to declare.
This manuscript has been publicly reviewed by members of the S.E.N., to whom the authors are grateful for their collaboration.
The Cerebrovascular Diseases Study Group of the Spanish Society of Neurology is formed by María del Mar Freijo Guerrero, Elena López-Cancio Martínez, Francisco Moniche Álvarez and Marta Rubiera del Fueyo.