Overwhelmed by the constant trickle, which in recent months has now turned into a flood, of migrants who come to accident and emergency fleeing the precarious renal replacement therapy (RRT) offered in developing countries, I consider it my duty to alert people to the situation.
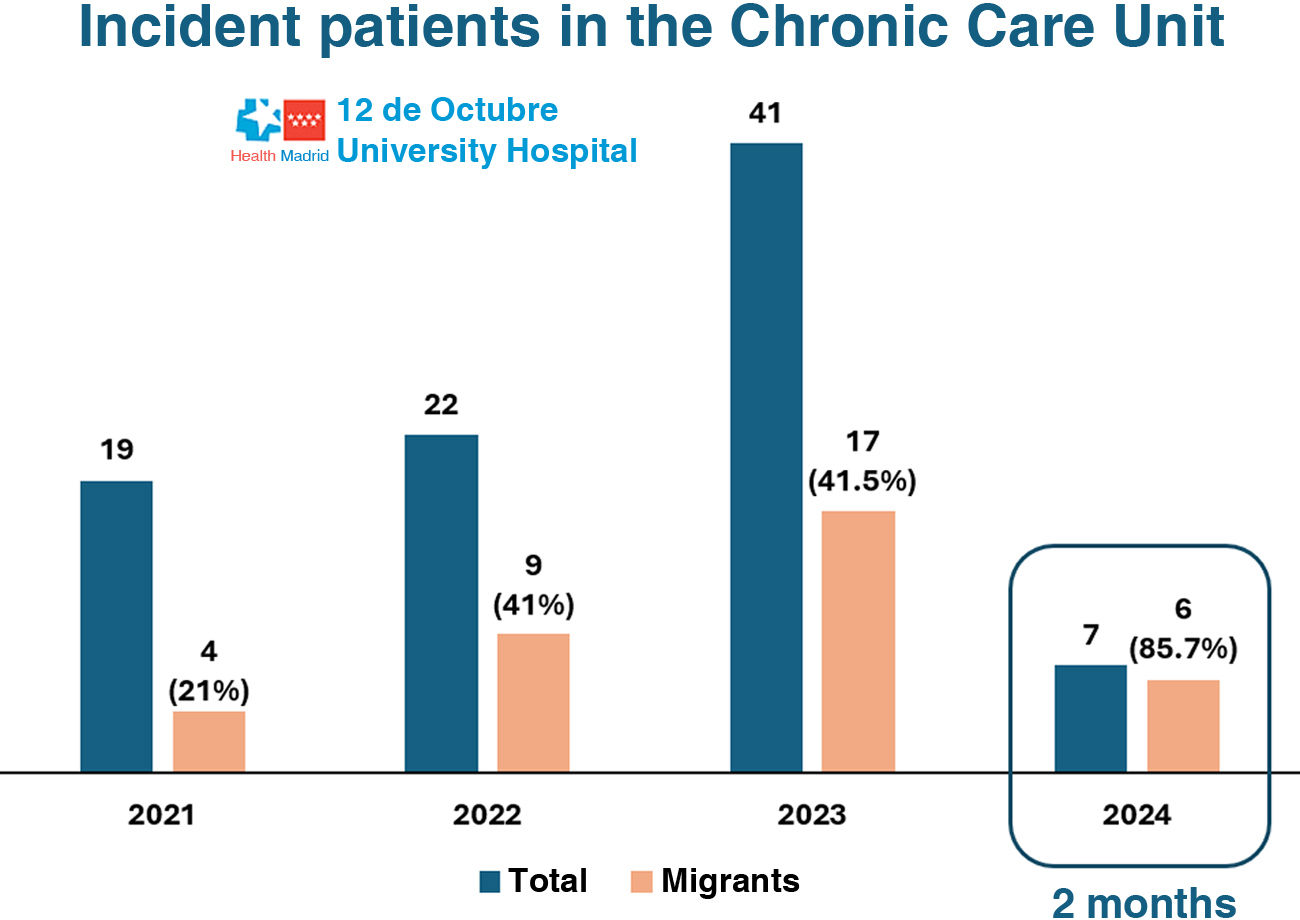
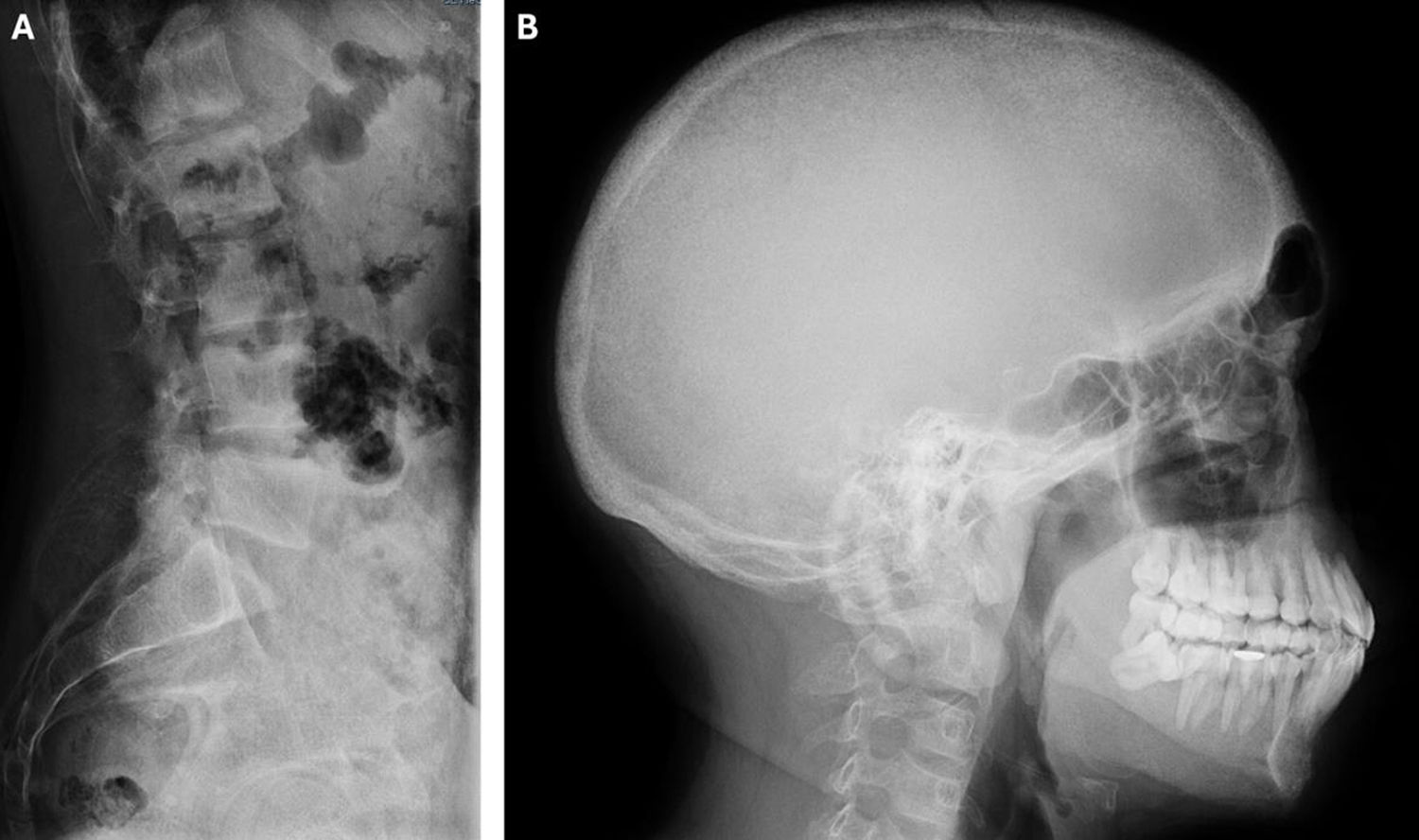
In the last six months, 17 people with terminal chronic kidney disease (CKD) on haemodialysis (HD) have come to the Hospital 12 Octubre Accident and Emergency Department to continue with their regular sessions. In recent years, the number of people arriving has continued to increase (Fig. 1). Each of these individuals reminds us that humanity and globalisation are failing, and that there is a gap in equity in access to RRT between countries. They are also teaching us the classic clinical signs of kidney disease, which Western nephrologists have forgotten, as they are the result of sustained underdialysis (Fig. 2). These people, after falling into debt to pay for treatment in countries where health coverage does not protect them, escape from their reality to continue living. Some of them, if they are lucky, have family or friends who take them in; others come alone and end up homeless. Migrants on RRT lack residence permits and work permits, in addition to suffering the employment problems of terminally ill patients who require hospital care three times a week.
As in other centres, individuals on HD in our health area who exceed the capacity of our hospital unit (n = 64) are channelled to peripheral centres (n = 160). People without a health card cannot be referred to these centres, so they displace more fragile and comorbid people who, for clinical reasons, should undergo in-hospital dialysis. Moreover, it does not seem fair that people who have paid taxes throughout their lives to maintain the public health system are deprived of the option of receiving dialysis in a hospital. Their feeling that patients with no health coverage constitute a threat is also logical. Owing to the lack of full health coverage, migrants are also not candidates for peritoneal dialysis or kidney transplants, both of which are economically more cost-effective for the health system, but which could be used as a lure for medical tourism.
As healthcare professionals, our mission is always to safeguard the health and interests of people, irrespective of their condition. Our job is not to punish illegal immigrants, nor to make things more difficult for them. This situation is awkward for everyone, and we all lose.
We are aware that this is a major global health problem, given the dramatic forecast of increasing prevalence and incidence of CKD, mainly attributable to population ageing in developed countries and access to diagnosis in developing countries. Consequently, it is estimated that in 2030, of the 14.5 million people with end-stage CKD, only 5.4 million will receive renal replacement therapy.1
The solutions to this problem would involve endowing developing countries with infrastructure, materials and knowledge so that they have the resources to offer adequate health care. However, there are other challenges to ensuring equity in areas with low population density, or in remote locations with limited access to water and electricity, and difficult transport links. These limitations imply physical barriers in the product replacement and repair chain,2 as evidenced by the impact that natural disasters or conflict zones have on access to RRT.3,4
Improving the funding of RRT is essential, given that it is estimated that less than 50% of countries5 provide any form of public financing for expensive RRT, condemning sufferers to destitution. Finally, we need care policies for people living with CKD, since we know that the cost of RRT is only the tip of the iceberg of a disease that affects 10% of the world's population.6 An urgent solution needs to be found to prevent the collapse of hospital units and ensure care for all patients.