Dear Editor,
Vascular access is very important in the management of patients beginning Long Term Haemodialysis (LTH) nonetheless, in spite of the advances achieved in many fields, there is a very large number of patients that reach dialysis without proper vascular access.
Recent data demonstrates that, irrespective of the recommendations of guidelines, the use of Arteriovenous Fistulae (AVF) is even decreasing.1,2 Therefore, this is a field where much work needs to be done.
In our hospital, we have carried out a retrospective study of all patients that began their LTH program between 1 January 2002, and 31 December 2003. Among other data we recorded the type of vascular access used at the beginning of their dialysis and at the end of the study, the dose of erythropoietin given during the entire period of the study to each patient (the annual dose was calculated for each one), the number of hospital admissions, in absolute numbers and calculated by total days, and the comorbidity score using the Charlson Co-Morbidity Index,3 calculated for the beginning and the end of the study.
63 patients began LTH during the period of the study. 41 of them (65%) were men. The average age was 60 ± 16 years for men and women. Fifty one percent of the patients were 65 years old or older. The average amount of time in the study was 9.3 ± 6.3 months. Of the 63 patients, 40 completed the study, The reasons for early termination of the study were exitus (four patients), transfer to another centre (four patients) and transplant (15 patients). The diabetic patients (19%) were older (66 ± 10 vs. 59 ± 17 years old), more obese (BMI 28 ± 7 vs. 25 ± 3) and they had a higher co-morbidity index than the rest of the patients.
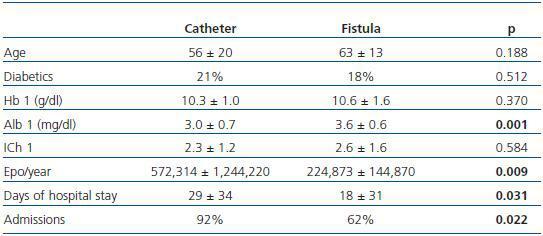
39 patients began dialysis with AVF (62%) and 24 patients with catheters (38%). At the end of the study, 6 patients were using catheters for dialysis. There were no differences in type of vascular access according to age, in diabetics or non-diabetics or to co-morbidity index. Statistically significant differences were found in the level of albumin, dose of erythropoietin received and in the number of hospital admissions (table 1). The average annual dose of erythropoietin was practically double in those patients that started dialysis with a catheter compared to those that began with an AVF.
There were no differences if the vascular access in the results at the end of the study was considered. Kt/V at the end of the study was similar in the group of patients using catheters or an AVF for dialysis. Seventeen patients (27%) were never hospitalized, 22 (35%) were hospitalized once, and the rest, 24 patients (38%), more than once. Only 8% of those that began with a catheter were never hospitalized.
Having an AVF prior to the commencement of HD is not only associated with better patient-reported quality of life,4 but is also linked to lower morbidity and mortality and healthcare expenditure.5-7 Our study confirms the fact that those patients that began LTH with a catheter have a greater number of hospital admissions, longer hospital stay and need higher doses of erythropoietin for similar levels of haemoglobin. Therefore, although the situation in Spain is fortunately better5,6,8 than in other countries,4 more work must be done to ensure the timely formation of an AVF as recommended in in the clinical practice guidelines.9,10
Table 1. Patient characteristics according to their first vascular access at the start of haemodialysis