Objetivo: analizar las características del fracaso renal agudo (FRA) en nuestro centro y determinar su influencia en el pronóstico del mismo y en la mortalidad. Material y métodos: estudio retrospectivo de los episodios de FRA valorados por nuestro Servicio durante un período de dos años (2005-2007). Los criterios de inclusión fueron: elevación de la creatinina sérica 0,5 mg/dl en pacientes con función renal previa normal y de 1 mg/dl en aquéllos con insuficiencia renal crónica previa. Se registraron factores epidemiológicos, clínicos, analíticos, terapéuticos y pronósticos. Resultados: valoramos 201 episodios de FRA. El 62,7% 16,38 (63,68% ±) eran varones. La edad media fue de 67,35 >65 años). El índice de comorbilidad de Charlson (ICCH) mostraba unos valores de 3,49 ± 2,43. Ciento quince pacientes tenían IRC previa al ingreso. El 52,7% fueron prerrenales, el 34,8% parenquimatosos y el 8,5% obstructivos. El 35,8% cursaron con oligoanuria. El tiempo medio de ingreso fue de 22,47 ± 21,3 días. El 70,1% de los pacientes recuperaron función renal al alta. La mortalidad fue del 30,8%. En el estudio univariante se asociaron significativamente con la mortalidad (p <0,05): ICCH, oliguria, hipoalbuminemia, niveles bajos de colesterol y anemia. En el análisis de regresión lineal múltiple, los factores que mejor la explicaban fueron: ICCH, oliguria y niveles bajos de colesterol. Realizamos un modelo predictivo de mortalidad con estos factores. Conclusión: la mayor complejidad clínica basal de los pacientes, el desarrollo de oliguria y la presencia de datos de malnutrición-inflamación aparecen como los principales factores pronósticos y de mortalidad en el FRA que valoramos los nefrólogos en el momento actual.
INTRODUCTION
ARF and chronic renal failure are the most common diagnoses in nephrology practice at this moment. ARF is a common problem in clinical practice, whether in outpatient or in-patient medicine, and with respect to the latter, it is present across all sections, in medical, surgical and intensive care units (ICU). At present, nephrologists in many centres share this disease and its treatment with other specialties, including Internal Medicine (pre-renal ARF and acute tubular necrosis [ATN]) and Intensive Care units (ARF in the critically ill, continuous extracorporeal dialysis techniques).
ARF is defined as a syndrome that arises from a rapid decrease in glomerular filtration rate, over hours or days, that presents as an increase in blood concentrations of nitrogenised products (urea, creatinine, etc.) with alterations in fluid and electrolyte homeostasis. The lack of simpler, more specific renal damage markers explains why there are more than 30 definitions of ARF, which make comparing different studies difficult.1 Recent articles focussing on analysing the concept of ARF have not proposed any definitions, although they do list varying opinions about what characteristics the disease should present.2-5
ARF has become one of the most serious problems faced by nephrologists8 due to its increasing incidence rate,6,7 its high mortality rate (near 50% in general series) and its global prognosis, which has hardly changed in the last 30 years.
The objective of our study is to perform a retrospective analysis of ARF characteristics in our Centre ¿a hospital with 406 beds in the Community of Madrid which provides care to a population of 182,431 inhabitants¿taking epidemiological, clinical analytical and therapeutic factors into account. Likewise, we will determine what influence these factors have on ARF prognosis and mortality.
MATERIAL AND METHODS
The study included ARF episodes that the Nephrology Division at Severo Ochoa Hospital recorded in all hospital areas, regardless of whether the disease developed in the Community or at the hospital, between 1 January 2005 and 1 January 2007.
ARF as defined as an increase in serum creatinine (CR) of 0.5mg/dl above the baseline in patients with normal renal function, and 1mg/dl for patients with a previous history of CRF.9 Recovery criteria were serum Cr returning to its baseline values (full recovery), or improvement of renal function by at least 50% (partial recovery) if the clinical profile suggested acute renal failure.
The following factors were recorded:
- Epidemiological: age, sex, section of admission, length of stay.
- Clinical:
- Associated comorbidity factors that could influence the development of ARF and its subsequent evolution: arterial hypertension (AHT), diabetes mellitus (DM), Charlson comorbidity index (CCI), prior potentially nephrotoxic treatment.
- ARF aetiology was grouped according to the normal physiopathological criteria:
- Pre-renal: functional, due to decrease in effective circulating volume.
- Cardio-renal: decrease in cardiac output with secondary renal hypoperfusion.
- Renal or parenchymatous: acute pathologies due to anatomical lesions to any of the renal structures (glomeruli, tubules, interstitium or vessels): acute primary or secondary glomerulonephritis, acute tubulointerstitial nephritis (TIN), acute tubular necrosis (ATN) caused by haemodynamic, toxic or both reasons (contrast, pigmenturias, sepsis, surgery, nephrotoxicity, other), cortical necrosis, vasculitis and atherombolic renal disease.
- Obstructive: pathologies that arise with an intrinsic or extrinsic obstruction of the urinary tracts. Those of tumourous and non-tumourous origins are considered separately.
- Development of oliguria, arterial hypotension.
- Analytic:
- Serum creatinine and urea (baseline, at admission, maximum and at discharge).
- Haemoglobin. Serum potassium. Urine sodium content. Acid-base equilibrium.
- Nutritional parameters: cholesterol, albumin, prealbumin.
- Inflammatory parameters: Ferritin, C-reactive protein (CRP).
- Therapeutic:
- Conservative treatment: diuretics, hydration.
- Kidney replacement therapy (haemodialysis, ICU extracorporeal continuous filtration techniques).
- Prognosis: The following are considered prognostic factors:
- Length of hospital stay.
- Need for ICU treatment.
- Need for kidney replacement therapy.
- Recovery of renal function.
- Mortality.
Statistical analysis
Quantitative variables were described using the mean and standard deviation, and qualitative variables, by frequency distribution. Qualitative variables were compared using the Chi-square test. We used the Student t-test for quantitative variables with a normal distribution and the Mann-Whitney test for those with a non-parametric distribution. The results obtained from the single variable study were introduced in the logistic regression analysis. Values of p < 0.05 were considered statistically significant. Odds ratios are given with a 95% confidence interval. Statistics software was used for the analysis (SPSS 10.0).
RESULTS
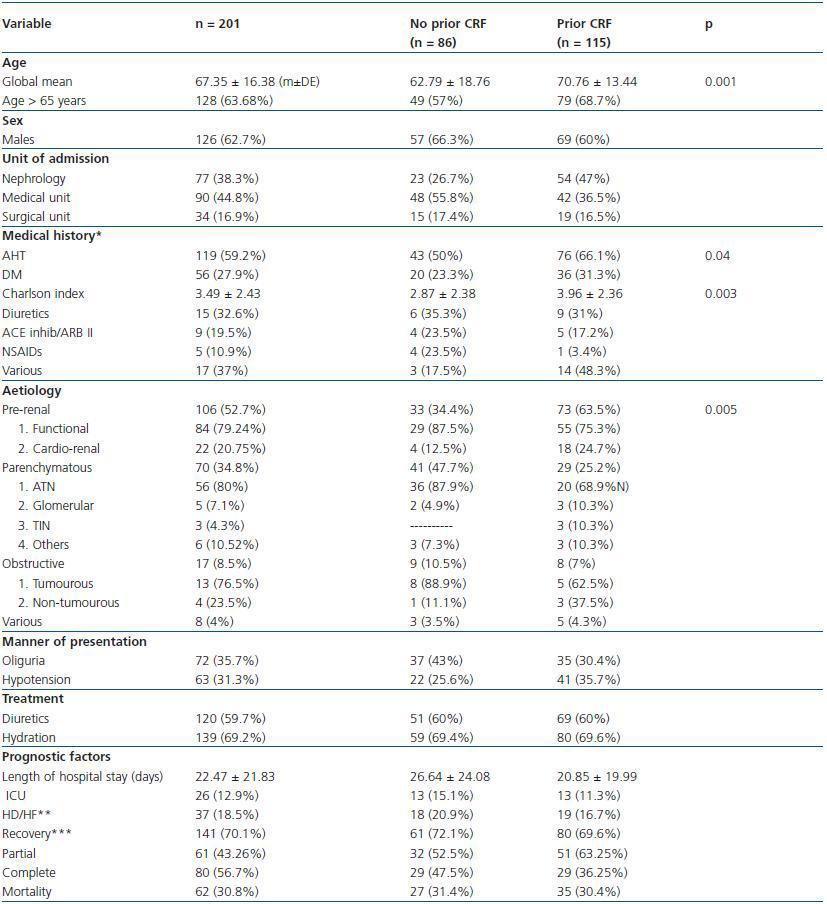
Study population: 201 ARF episodes that occurred over a period of 24 months were studied retrospectively. The mean patient age was 67 years (range: 19 to 99) and there were 126 males and 75 females. Age was similar for both sexes (65.88 ± 16.43 vs. 69.81 ± 16.07). Out of the patient total, 128 (63.68%) were 65 years old or older. 38.3% were admitted to the Nephrology Department, and 61.7% were admitted to other divisions (44.8% medical and 16.9% surgical). The mean hospital stay was 22.47 ± 21.83 days. Table 1 summarises the characteristics of patients included in the study.
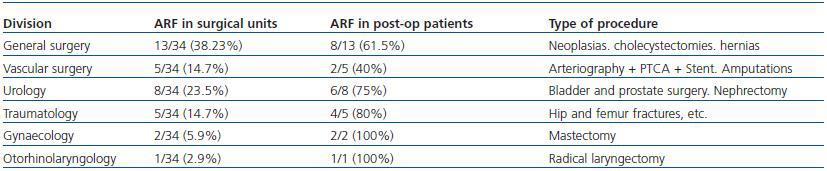
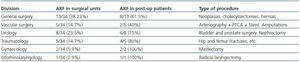
Out of the 34 patients who presented decreased renal function while admitted to the care of surgical units (general, vascular, urological, traumatological, gynaecological, otorhinolaryngological and ophthalmological surgery), only 23 (67.6%) underwent some type of surgical procedure (table 2).
Clinical characteristics
59.2% of the patients were hypertensive and 27.9% were diabetic. Associated comorbidity was evaluated using the CCI, which showed values of 3.49 ± 2.43. We found drugs that were able to the influence renal function in 44 patients (21.9%), whether alone or in association with another treatment (diuretics 7.5%, ACE inhibitors/ARB II 4.5%, NSAID 1.5%, various 8.5%).
The most frequent aetiology was pre-renal, which accounted for 52.7% of the cases (79.24% functional, 20.75% cardiorenal). The second aetiological group corresponded to renal or parenchymatous origin, and made up 24.8% of the cases. Within this group, ATN was the most frequent type (80%) with particular mention of drug-induced nephrotoxicity (15.7%), particularly from aminoglucosides. Obstructive causes accounted for 8.5% of the total ARF episodes, and their most frequent origin was tumoral disease (76.5%). Of the total tumours, 53.8% were urinary tract tumours, 38.7% solid organ tumours and 7.7% of haematological origin. A total of six renal biopsies were performed (3%).
The CCI showed no significant differences among the three aetiological ARF groups.
35.8% of the patients presented oliguria, and arterial hypotension was present in 31.3% of cases, regardless of ARF aetiology.
Analytical data
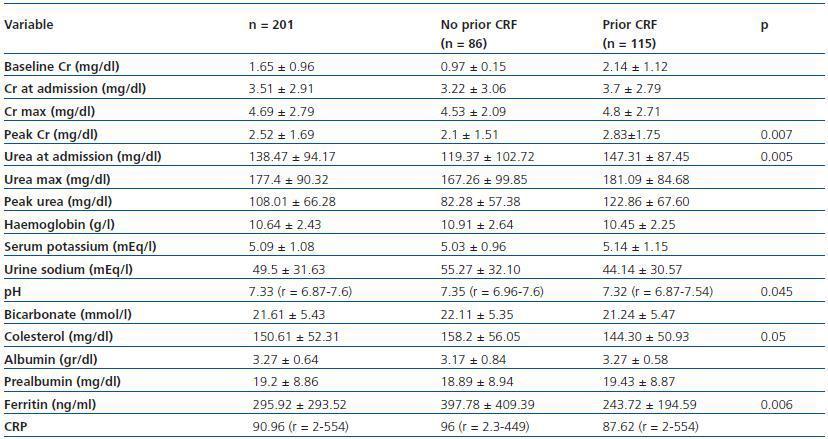
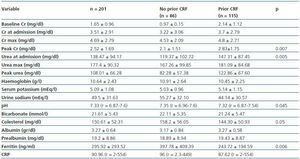
Analytical data appears in table 3.
Therapeutic results
59.7% of the patients received diuretic treatment and 69.2% received hydration.
During the episode, 18.5% of cases (37 patients) required kidney replacement therapy using invasive techniques: haemodialysis in 59.5%, continuous veno-venous haemofiltration (CVVH) in 10.8%, and both techniques in 29.8% of patients.
Prognostic factors
The mean hospital stay was 22.47 ± 21.83 days. Patients who developed oliguria had the longest hospital stays (27.94 ± 22.52 vs. 19.42 ± 20.90, p = 0.0009). The presence of hypoalbuminaemia (p = 0.009, r = 0.29) and high CRP values (p = 0.0001, r = 0-29) were a constant for patients with a longer hospital stay.
26 patients were admitted to the ICU (12.9%). On average, these patients were younger than those who were not admitted to the ICU (63.06 ± 15.62 vs. 68.28 ± 16.43 years, p = 0. 059). Parenchymatous aetiology was the most frequent cause of ARF in this group (p = 0.06). Patients requiring admission in the ICU had a higher frequency of oliguria (p = 0.001 and arterial hypotension (p = 0.001) compared to those who were treated in other units. Serum prealbumin levels were significantly lower in patients who were admitted in Intensive Care (14.75 ± 8.03 vs. 20.22 ± 8.77, p = 0.001), whereas ferritin and CRP levels were significantly higher (373.66 ± 224.86 vs. 289.92 ± 301.23, p = 0.03, and 146.27 ± 128.66 vs. 78.78 ± 98.27, p = 0.003, respectively) in the ICU patient group.
Kidney replacement therapy was more frequent for the patient group with parenchymatous aetiology (p = 0.0001) and in those who developed oliguria (p = 0.0001) or arterial hypotension (p = 0.018) during the episode. It was also more frequent in the group of patients admitted to the ICU (p = 0.0001). It is also associated with elevated figures for Cr (6.91 ± 4.16 vs. 4.17 ± 2.09, p = 0.001), plus inflammation (CRP: 145.10 ± 143.92 vs. 75.86 ± 89.47, p = 0.019) and malnutrition, with lower figures for albumin and prealbumin (2.96 ± 0.78 vs. 3.34 ± 0.58, p = 0.0007 and 15.16 ± 7.89 vs. 20.46 ± 8.9, p = 0.01, respectively). Of the 37 patients (18.5%) who required renal support techniques, three remained on chronic haemodialysis (8.1%).
70.1% of the patients had recovered renal function at the time of discharge, according to the criteria described previously (partial recovery, 43.26%; complete recovery, 56.7%). Associated comorbidity was significantly lower in patients who recovered their renal function (3.17 ± 2.35 vs. 4.27 ± 2.46, p = 0.003), compared with those who did not recover it. Pre-renal aetiology was associated with better recovery of renal function (p = 0.07). The development of oliguria/arterial hypotension was not shown to be a determining factor for recovery. Treatment with diuretics and expansion were significantly associated with renal function recovery (p = 0.026 and p = 0.001, respectively). Patients who recovered their renal function had lower maximum Cr levels (4.32 ± 2.49 vs. 5.94 ± 2.16, p = 0.003), higher haemoglobin levels (10.95 ± 2.58 vs. 9.7 ± 1.82, p = 0.002) and a lower tendency toward acidosis (bicarbonate: 22.09 ± 5.74 vs. 20.51 ± 4.49, p = 0.06).
30.8% of the patients died, a higher percentage of males than females (67.74 vs 32.25%). Mortality was similar among older and younger patients (31.25% in patients > 65 years and 30.14% in patients < 65 years. The CCI was significantly higher for the patients who died (4.52 ± 2.77 vs. 3.04 ± 2.12, p = 0.0001). Patients who developed oliguria during the episode had a higher mortality rate (p = 0.002). Mortality rates varied according to the unit of admission: Medical 63%, Surgical 5%, Nephrology 22.6%. Patients who were admitted to the ICU tended to have a higher mortality rate (p = 0.07). The aetiology of the renal failure, length of the hospital stay and need for kidney replacement therapy were not determining factors for mortality in our sample. The presence of hypoalbuminaemia (3.12 ± 0.71 vs. 3.33 ± 0.61, p = 0.045), lower cholesterol levels (134.67 ± 55.18 vs. 157.07 ± 51.22, p = 0.008) and lower haemoglobin levels (10.83 ± 2.56 vs. 10.23 ± 2.08, p = 0.08) were present in the patients who died.
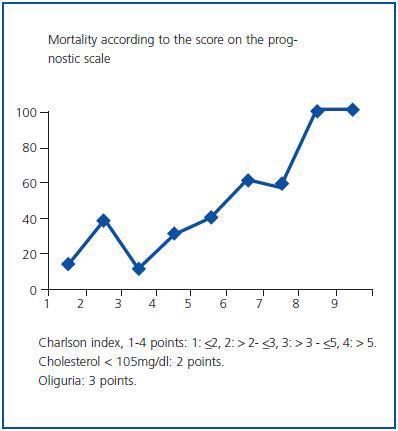
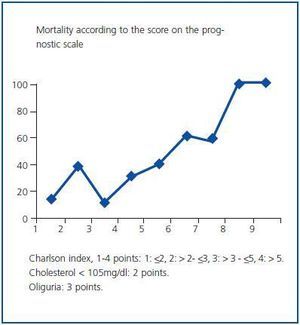
In the logistic regression analysis, the factors that best explain mortality during the hospital stay were the CCI (ExpB: 1.517, CI 95% 1.1-2.01), the development of oliguria (ExpB: 2.847, CI 95% 1.4-5.6) and serum cholesterol levels (ExpB: 2.165, CI 95% 0.9-4.9).
With the above data, we created a mortality prediction model and assigned the following values according to the OR: CCI, 1 to 4 points according to the quartile the patient belonged to: (1: ≤2, 2: >2- ≤3, 3: >3- ≤5, 4: >5); the presence of oliguria, 3 points; and cholesterol lower than 105mg/dl, 2 points. By thismethod, we obtained values from 1 to 9 for all cases. This scale was used to elaborate the prognostic curve shown in figure 1.
Previous normal renal function/previous CRF
Patients with a previous history of CRF who developed acute renal failure were older than those whose renal function had previously been normal (70.93 ± 13.49 vs. 62.75 ± 18.54, p = 0.001). The CCI showed significantly higher values in this patient subgroup (3.94 ± 2.38 vs. 2.92 ± 2.38, p = 0.003). 62% of the patients with a previous history of CRG were hypertensive, while only 37% of the group with a normal renal history had hypertension (p = 0.04). Patients admitted to the Nephrology division had a higher prevalence of prior CRF (46.96% Neph, 36.52% Med and 16.52% Surg, p = 0.009), with significantly higher Cr figures at time of admission (Neph: 4.26 ± 2.39, Med: 2.79 ± 1.93, Surg: 3.74 ± 5.04 (r = 1.99-5.51) (p = 0.004). Pre-renal aetiology was the most frequent cause of acute renal failure of patients who had CRF prior to admission (p = 0.005). Patients with a history of CRF had lower cholesterol levels (143.59 ± 51.13 vs. 158.89 ± 55.46, p = 0.05); a greater tendency toward acidosis (pH: 7.33 ± 0.10 vs. 7.36 ± 0.09, p = 0.045) and significantly lower levels of ferritin (229.20 ± 173.54 vs. 416.54 ± 409.49, p = 0.006), (Tables 1 and 3).
Older patients (± 65 years) vs. younger patients (< 65 years)
The older patient group had a higher AHT prevalence than the younger patient group (68.72 vs 42.46%, p = 0.0001) and a significantly higher CCI (3.75 ± 2.27 vs. 3.04 ± 2.64, p = 0.046). The most frequent cause of ARF in the older population was pre-renal in origin, followed by parenchymatous and obstructive (59.3, 31.25 and 8%,
respectively); in the younger patient group, 41% of the cases were of pre-renal origin, 41% renal and 8%, obstructive episodes. There were also differences in the serous ferritin values, which were higher in the < 65 population (225.89 ± 164.69 vs. 366.20 ± 245.20, p = 0.001). We found no differences regarding length of stay, recovery of renal function or mortality.
DISCUSSION
The progressive increase in ARF¿s incidence rate6,7 and its high morbidity and mortality8 have led us to assess the characteristics of the ARF episodes evaluated by the Nephrology Department in our hospital. Our intention was for the studied population to be representative of the type of patients who are seen in our hospital. However, considering that other specialties are also involved in treating this disease at present (pre-renal ARF with good evolution, ARF in the ICU, patients with serious pathologies that suggest a rapid decline), its incidence rate is sure to be even higher.8,10-12 On the other hand, each centre¿s characteristics and the divisions at its disposal will also affect the incidence of different types of ARF.
As in other series, ARF is very frequent in males and in the elderly.10-16 On many occasions, the patient has an underlying associated condition (AHT, DM, cardiovascular disease, etc.) for which normal treatment includes diuretics, reninangiotensin-aldosterone blockers or NSAIDs. Although these drugs produce benefits by lowering cardiovascular risk, controlling pain etc.,there are clinical risk situations in which they could lead to decreased renal function by reducing volume or altering renal adaptation mechanisms.17 In daily clinical practice, it is becoming increasingly frequent to find several of these drugs implicated simulaneously in cases of acute renal failure.
In this series, the most frequent aetiology was pre-renal,11,17 with renal hypoperfusion or decreased cardiac output as the emerging physiopathological mechanism; it is very likely that this aetiology will increase in the coming years. Within the parenchymatous aetiology group, ATN was the most frequent cause, and a sizeable proportion of that subgroup was due to nephrotoxicity from drugs, particularly aminoglucosides. It is therefore necessary to insist once more on adjusting doses according to renal function, controlling levels, and identifying risk factors that favour a drug¿s toxicity to the kidneys.18 The incidence rate for obstructive ARF is lower than in other series,19 and its most common aetiological subgroup is that of tumour origin. It is becoming increasingly common to find patients with multiple pathologies or varyingly serious inflammatory processes that involve different aetiological factors (mostly pre-renal and renal), and these require joint global assessment.17
Our data, like those described by other authors,19 demonstrate that ARF is a universal problem in clinical practice. It develops in all hospital areas, whether medical or surgical (Nephrology 38.3%, Med 44.8% and Surg 16.9%), in addition to the ICU. This means that any doctor, regardless of his or her specialty, must be capable of identifying these episodes. The aetiology of the ARF that nephrologists treat (pre-renal 64.93%, parenchymatous 24.6%, obstructive 2.5%, various 7.79%) is different from that observed in the medical division (pre-renal 46.67%, parenchymatous 44.44%, obstructive 7.78%, various 1.11%) or the surgical division (pre-renal 41.17%, parenchymatous 32.35%, obstructive 23.53%, various 2.94%).
Approximately two thirds of patients received treatment with diuretics or hydration for the ARF episode, and generally responded well.
The mean hospital stay was longer than that described in other studies,19-24 and developing oliguria and the presence of inflammation/malnutrition indicators were the main factors determining the length of the stay. This could be due to the presence of an increasingly older population with more baseline comorbidities, and which is therefore more complex to treat clinically.
Patients who were admitted to the ICU were younger, with a more serious state of inflammation and presenting established acute renal failure, which was possibly indicative of their clinical situation. In this context, they developed oliguria and arterial hypotension and needed kidney replacement therapy more frequently than the patients who did not require admission to the ICU.
Replacement therapy was necessary in 18.5% of the patients we evaluated. These figures are 36% lower than those reported in similar studies.11,12,19,20 This may be due to continuous extracorporeal filtration techniques being performed by the ICU in our centre (and many others); nephrologists do not generally participate in follow-up for this type of patient. Intermittent haemodialysis is still the most frequent kidney replacement therapy (16.4 vs. 7.5%) recorded in our hospital; on some occasions, it may be preceded or followed by CVVH in critical patients. For all cases, a low-flux polysulphone dialysis membrane with a surface area of 1.7m2 was used. The mean number of sessions was 4.05 ± 2.95 (r = 1-12). Parenchymatous aetiology, the development of oliguria or arterial hypotension, higher levels of serum Cr and the inflammation/malnutrition data had a significant presence in patients who needed kidney replacement therapy. In our study, three patients (1.49% of the patient total and 8.1% of those who needed KRT) did not recover their renal function and were included in a chronic haemodialysis programme. Liaño and Kjellstrand19,24 describe a similar incident.
70.1% of patients recovered kidney function by the discharge date. Pre-renal aetiology, absence of oliguria, the presence of lower Cr values and a higher level of haemoglobin were associated with recovery.
The global mortality rate of patients attended by nephrologists in our centre is 30.8%, which is significantly less than that described in other series.19,22-24 These differences may be related with ARF episodes that are not evaluated by our Department (ARF in the ICU, patients with serious diseases that suggest a rapid decline). However, two recent studies that describe the epidemiogical and prognostic evolution of ARF throughout the last decade point to a recrease in the disease¿s mortality rate although an increased number of ARF episodes were observed during that period.6,7 As we described previously,25-27 mortality rates are significantly lower among patients who are admitted to the Nephrology division. On the one hand, this could be due to the aetiological differences in renal failure according to the unit admitting; it could also be due, as Feest, Round and Haman,14 Liaño19 and other authors28-30 suggest, to a more precise initial diagnosis permitting better treatment. Once again, associated comorbidity and the development of oliguria appear as prognostic factors for mortality. It is being debated whether or not advanced age is a mortality index in published studies on that topic. Some found a clear correlation;11,14,21,31 others have not shown that it has weight as an isolated factor, although it may have when associated with underlying disease.29,32-34 In our sample, we did not observe a higher mortality rate among the older patients.
However, comorbidity (measured using the CCI) appears to be a determining factor for mortality, and it is significantly higher in this patient group. This supports the importance of the connection between advanced age and associated disease as a mortality risk factor. As described in the literature, the mortality was higher in the population that required admission to the ICU.29,30,35 Inflammation and malnutrition data were significantly present in the patients who died. In the logistical regression analysis, the factors best explaining mortality were the CCI, the development of oliguria and the serum cholesterol levels.
With these data, we have developed a predictive model in which a patient with a CCI higher than 5 (top quartile: 4 points), oliguria (3 points) and cholesterol levels below 105mg/dl (2 points), would total 9 points for a mortality risk of 100%. Meanwhile, a patient with a CCI below 2 (bottom quartile: 1 point), with no oliguria and cholesterol levels above 105mg/dl, totalling 1 point, would have a mortality risk of 12% during an ARF episode.
These data show that baseline comorbidity, the development of oliguria and malnutrition/inflammation data are important prognostic factors. Nephrologists are assessing an increasing number of ARF episodes in older patients, and more particularly, in patients with significant associated comorbidity.36 This baseline complexity may be more important factor in determining the global prognosis for ARF (recovery of renal function, mortality) than those factors related to the renal failure episode itself (duration, aetiology, analytical values, etc.). Apart from this patient group, we also have the patients admitted to the ICU (26 in our study, and therefore, not very representative of this population). ICU patients are younger, frequently with associated cardiovascular collapse (oliguria, arterial hypotension) and with more inflammation (increased CRP and decreased prealbumin). In the ARF prognosis for these patients, it is likely that baseline comorbidity would be less important than the inherent seriousness of the episode itself. A prospective study published by Liaño et al. in 2007 covered a long-term follow-up on 187 patients who had developed ATN and established that evolution following ARF was better in young patients with no associated comorbidity and in those who were admitted with multiple trauma, surgical pathology or requiring a stay in the ICU. Renal function during follow-up was normal in 81% of the patients. The delayed mortality rate was high and related to the underlying disease.37 These long-term follow-up data show similar results to those that we suggest for the acute phase of renal failure.
Our new social health situation (increasingly older patients with significant associated comorbidity) may require a new approach for the ARF patient, which should not be limited to purely renal factors (uraemic or hydroelectrolytic metabolism). Rather, it should consider the patient¿s associated comorbidity with a view to making preventative, diagnostic and therapeutic decisions.
In conclusion, the patients who were examined by the Nephrology Division in our hospital while suffering an ARF episode can be described as follows: 1) they required a longer stay that described in other series; 2) the development of oliguria and arterial hypotension, and data showing malnutrition/inflammation were present for patients who were admitted to the ICU; 3) 18.5% required kidney replacement therapy, which was related to parenchymatous aetiology, the development of oliguria and arterial hypotension and the presence of inflammation/malnutrition data; 4) 70.6% recovered their renal function, and absence of oliguria, lower Cr figures and higher haemoglobin levels were the principal factors determining recovery; and 5) mortality was higher in the group with the most baseline clinical complexity (highest CCI), in those that developed oliguria (resulting in more cardiovascular damage) and in those with lower cholesterol levels (MIA syndrome). These data reflect the change in the type of population that nephrologists are treating with increasing frequency.
Table 1. Characteristics of patients with ARF. Comparison between patients with prior normal renal function
and those with baseline CRF
Table 2. ARF in surgical units
Table 3. Laboratory analyses for patients with ARF. Comparison between patients with prior normal renal
function and those with baseline CRF
Figure 1.