Introducción: Para garantizar una adecuada continuidad de la asistencia de los pacientes que se dializan en centros de hemodiálisis extrahospitalarios concertados (CH), es fundamental que exista una estrecha relación y comunicación entre los propios CH y los hospitales de referencia (HR). El objetivo de este trabajo es conocer aspectos actuales de esta relación para detectar oportunidades de mejora. Material y métodos: Estudio transversal y descriptivo mediante dos encuestas autocumplimentadas, una dirigida a CH (81 preguntas) y otra a HR (56 preguntas), que abordaban distintos aspectos de la relación entre ambos. La encuesta se envió a través del correo electrónico disponible en la S.E.N. Resultados: Se recibió respuesta de 80 CH y 30 HR. De estos últimos, sólo 27 tenían relación con CH dependientes de su área. El 70% de los CH pertenecen a multinacionales y el 16% están ubicados dentro de un hospital. El 64% de los CH precisa la contratación de no nefrólogos para la asistencia. Casi un 40% de los nefrólogos de los CH hace guardias en los HR. Más de tres cuartas partes de los nefrólogos de los CH están solos durante toda su jornada laboral. Respecto a la relación entre ambos tipos de centros, es frecuente la comunicación telefónica bidireccional. Alrededor de un tercio de los pacientes remitidos al centro desde el hospital no aporta serologías actualizadas ni tiene un acceso vascular definitivo realizado. La remisión del paciente desde el centro al hospital suele ser muy completa, con pruebas actualizadas e informe completo. El 41,3% de los CH refería haber sido consultado por el HR con relación a toma de decisiones acerca de sus pacientes. Las analíticas y pruebas complementarias de protocolo en el CH vienen predefinidas por el concierto en el 65% de los casos, pero pueden ser modificadas en su mayoría por los propios centros, siendo consensuadas entre ambos en más de la mitad de los casos. El 60% de los CH puede pedir directamente interconsultas con otros especialistas, pero más de la mitad precisa del nefrólogo del HR para hacerlo. En su mayor parte, la medicación parenteral es suministrada al centro por el HR, pero más de un tercio de los centros tiene limitaciones para solicitar al HR dedicación parenteral de uso hospitalario menos común o no especificada en el concierto. Los HR refieren que la mayoría de los accesos vasculares se realiza en el propio hospital, mientras que los CH refieren que esto ocurre sólo en la mitad de los casos. En más de una tercera parte, las fístulas de pacientes en prediálisis se realizan en el centro como colaboración con el HR. La mayoría de los centros puede intervenir en la decisión de inclusión de sus pacientes en la lista de espera de trasplante. En sólo la quinta parte existe una base de datos común entre el CH y el HR, y menos de la mitad comparte protocolos de actuación u objetivos comunes. El 62,5% de los centros participa en ensayos clínicos conjuntos con el HR. Más de la mitad de las empresas proporciona formación a sus CH, ya sea directamente por la propia empresa o facilitando la asistencia a jornadas congresos. Conclusiones: Algunos de los aspectos que parecen manifiestamente mejorables son: la soledad de los nefrólogos de los CH y su acceso limitado a la formación; la adecuada remisión de los pacientes de los HR a los centros; la autonomía de los nefrólogos a la hora de solicitar interconsultas a especialistas sin precisar de la tutela de los nefrólogos del hospital; o la limitación a la hora de acceder a la medicación de uso hospitalario. Una estrecha relación entre CH y HR es de gran importancia para asegurar una mejor y más equitativa asistencia a nuestros pacientes. La creación de un foro de debate favorecería la puesta en común y la resolución de estos aspectos.
INTRODUCTION
Since haemodialysis began in Spain in 1957, private dialysis has existed as a solution for the slow bureaucratic/administrative process and the scarcity of places in public hospitals. These issues have led to some medical teams responding to demand via independent means. This has always created debate among both parties, as reflected in an editorial by Dr. de Francisco in 1995.1
At present, a large proportion of patients belonging to the public system receive haemodialysis in private outpatient centres, and these centres are also attended by a significant number of nephrologists in order to develop their professional skills. To guarantee fairness in treatment, the services provided by these centres are coordinated with the health delegations in each distinct Autonomous Community across Spain.
In 2003 the Outpatient Haemodialysis Working Group was created as an initiative of the Spanish Society of Nephrology (SEN). Since that time the group has carried out a number of activities, most notable of which are annual meetings where subjects of special interest to outpatient nephrologists are discussed. Such matters include efforts to carry out research and raise awareness in the larger nephrological community on how best to work in private centres,2 something which to an extent provides answers for some of the previously raised issues.1
Starting with the premise that, in order to ensure adequate continuity of care for patients, it is essential that there is a close relationship and tight communication between centres and referring hospitals, as well as a profound understanding of the difficulties and problems faced by each of these sectors in relation to each other, the SEN Outpatient Haemodialysis Group designed an investigation with the goal of analysing these issues and detecting possible opportunities for improvement. This investigation also approached the subject of working systems in hospital centres (HC) and levels of coordination with the referring hospitals (RH), as well as facilities provided by private companies for continued research and training.
The aim of this work is to evaluate the basic aspects of the relationship between outpatient dialysis centres and the RHs o which they report. The study was carried out using the auto-complete investigative technique in order to ensure generalised access and reasonably short evaluation time.
MATERIAL AND METHOD
A cross-sectional descriptive study was carried out, using a questionnaire in the form of a survey. All outpatient dialysis units across the country and all RHs were invited, using the SEN email database, to participate. Data was collected by the study coordinators via email or fax.
Data collection remained open for two months.
Outpatient dialysis centres were defined as those situated in strategic locations around the health district and linked to a hospital nephrology department, where either conventional haemodialysis or other techniques are administered.
Two questionnaires were undertaken: one directed at the outpatient centres and the other at RHs.
The questionnaire for outpatient centres consisted of 81 questions, and the referring hospital questionnaire contained 56 questions, the majority of which had closed (yes/no) answers and others with numerical answers. Some responses were not mutually exclusive and a number of centres display mixed formulas in some of the aspects analysed, meaning that the some percentages total more than 100%.
The questionnaires dealt with the following topics:
1. Type of company to which the centre belongs (multinational, reporting to hospital nephrologists, private, or independent, non-multinational company).
2. Location of centre and type of activity (outpatient, within a hospital).
3. Centre work:
a. Linking of nephrologists with referring hospitals where these exist (via shifts, consultations, etc.)
b. Working within a team or as the only physically present professional
c. Presence of non-nephrologist doctors in the units, and level of involvement
d. Decision-making responsibility in the centre
4. Relationship with the referring hospital:
a. Referral of patients from hospital to centre
b. Admissions
c. Supplementary and analytical testing
d. Vascular accesses
e. Transplants
f. Medication
5. Working procedures
6. Research
7. Training
STATISTICAL ANALYSIS
The responses were incorporated into the SPSS 12.0 program. These were presented as totals and percentages, averages, average standard deviations (SD) and ranges. In accordance with the current notation norms, SD was expressed as a figure in parentheses following the average value.
RESULTS
Responses obtained
Responses were received from eighty centres and thirty hospitals. Of the latter, only 27 were linked with dependent private haemodialysis centres in their area.
Centre features
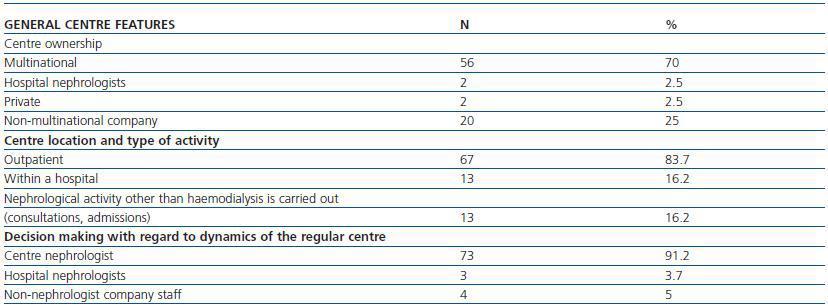
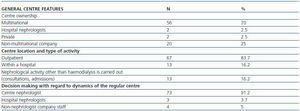
Table 1 shows features of the outpatient centres. In 29 centres (36.2%), care was provided exclusively by nephrologists; the remainder specified no use of nephrologists for care provision. In 57.5% (N = 46) of centres, non-nephrologist doctors were supervised by a nephrologist, in 61.3% (N = 49) doctors were present only during dialysis sessions and 35% (N = 28) provided full care for the patient, including follow-up and monitoring of laboratory tests and treatments. 38.7% (N = 31) of centre nephrologists performed shifts in public hospitals: 20% (N = 16) in the centre¿s RH and 18.7% (N = 15) in hospitals other than that with which the centre is linked. 78.7% (N = 63) of nephrologists working in centres remained alone for the duration of their working day, 41.2% (N = 33) did not meet with colleagues at all and 37.5% (N = 30) met colleagues only during shift handovers. Only 21.2% (N = 17) of doctors worked at the same time as other medical colleagues.
Regarding RHs, 90% of those which responded to the investigation (27/30) had one or more private HCs linked to their hospital, a number which ranged from one to five (average 2.08 centres). Of these centres, 59.2% were part of a multinational organisation, 11.1% belonged to private companies, and 29.6% belonged to independent, nonmultinational companies. Four hospitals (14.8%) stated that centre nephrologists performed shifts in the hospital, and three (11.1%) stated that centre nephrologists carried out tasks other than shifts within the hospital (external consultations, hospitalisations, research, etc.). 22.2% (N = 6) of the hospitals which responded made decisions regarding organisation and spending in the private centre.
RELATIONSHIP BETWEEN PRIVATE CENTRES AND REFERRING HOSPITALS
Initial patient referral from hospital to centre and hospital admissions
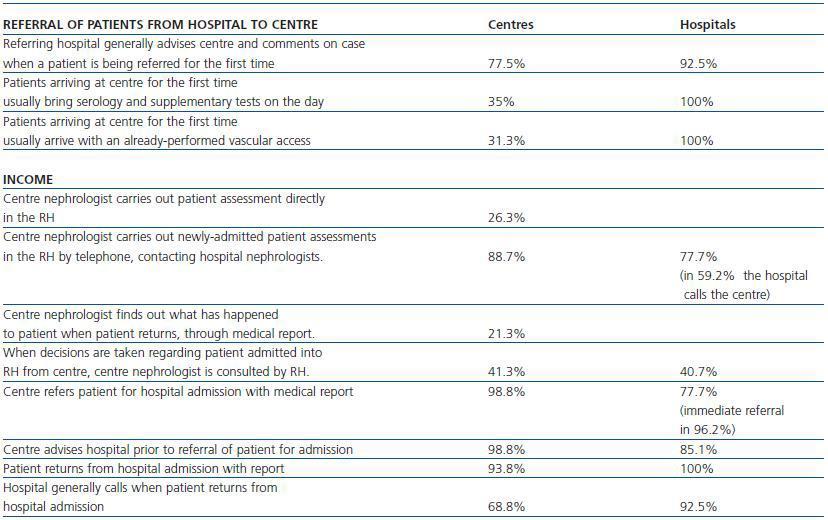
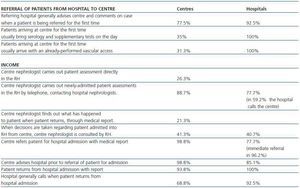
Table 2 shows the manner of patient referrals between centres and hospitals for hospital admission and referral from hospital to centre upon patient discharge, according to the responses given by HCs and RHs.
In 75% (N = 60) of centres, centre doctors report the ability to monitor their patient when the patient is admitted to the RH.
Centre management of supplementary and laboratory tests
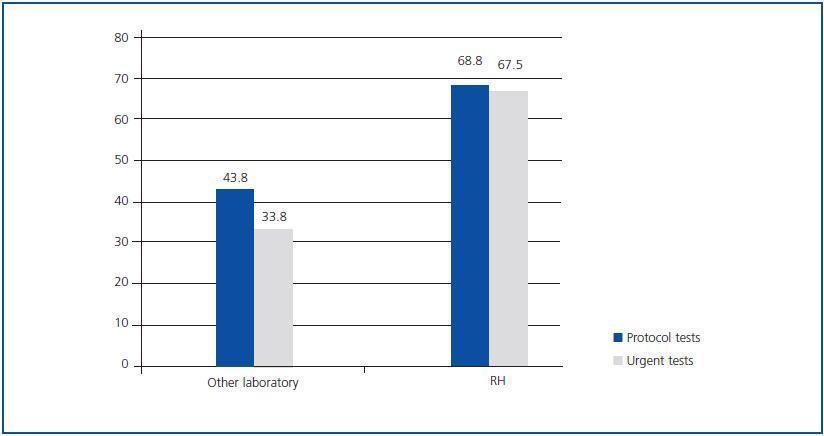
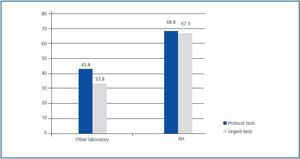
73.7% (N = 59) of the centres which responded to the investigation reported the ability to carry out laboratory tests and supplementary tests within the centre. In 65% of these cases, the decision regarding which laboratory tests and supplementary tests should be carried out is predefined by agreement with the management, but can be modified or influenced by decisions from centre nephrologists (72.5%/N = 58) or the RH (17.5%/N = 14). In eight centres (10%), neither the nephrologist nor the RH can influence this decision. Responses obtained from RHs were in this regard similar to those obtained from the centres: laboratory tests are predefined by agreement with the management in 51.8% (N = 14) of centres. Centre nephrologists can decide in 66.6% (N = 18) of centres, in 18.5% (N = 5) the RH decides, and in 14.8% neither the centre nephrologist nor the RH influences this decision. In 59.2% (N = 14) of cases the centre and hospital reach an agreement.
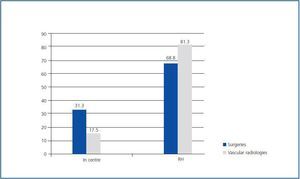
Figure 1 shows where urgent laboratory tests are carried out and centre protocol. 95% (N = 76) of centres report being able to request laboratory tests which are not in the previously stipulated protocol, based on clinical implications from their own dialysis centres, and 77.7% (N = 21) of hospitals second their requests.
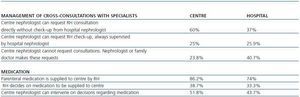
Management of cross-consultations with specialists and the supply of parenteral medication
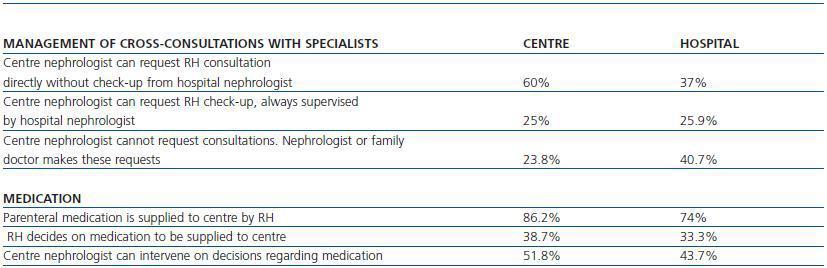
35% (N = 28) of centres report directly maintaining communication with other RH services without the need for mediation from the hospital nephrologist; 43% (N = 35) maintain this link via the hospital nephrologist; in 21.2% (N = 17) of centres no such communication exists. 31 centres (38.7%) report limitations on utilising and requesting parenteral medication from the RH for hospital use which is either uncommon or not specified in the agreement, such as antibiotics, urokinase, etc. (table 3).
Management of vascular accesses
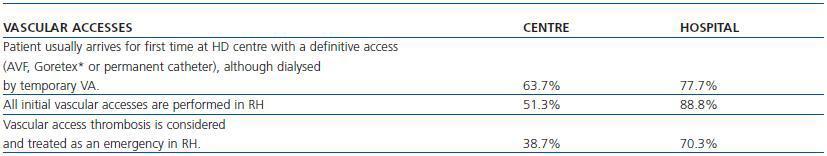
Table 4 shows how vascular accesses are managed between HC and RH. Up to 33.8% (N = 27) of centres state that fistulae for predialysis patients are performed by the centre, in collaboration with the RH, to try to alleviate the waiting list for vascular accesses.
85% (N = 68) of centres state that urokinase is used in the centre, only 13.8% (N = 11) perform venographies in the centre, 12.5% (N = 10) fit temporary catheters and 13.8% (N = 11) change temporary catheters. The remainder is referred to the referring centre.
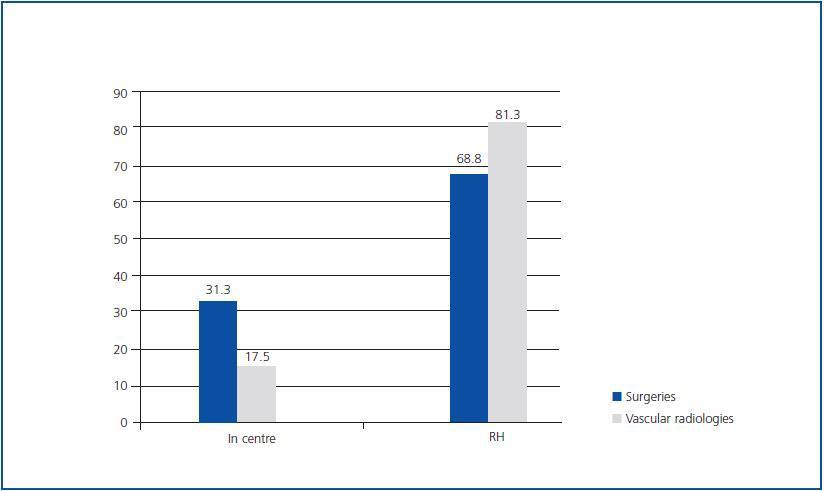
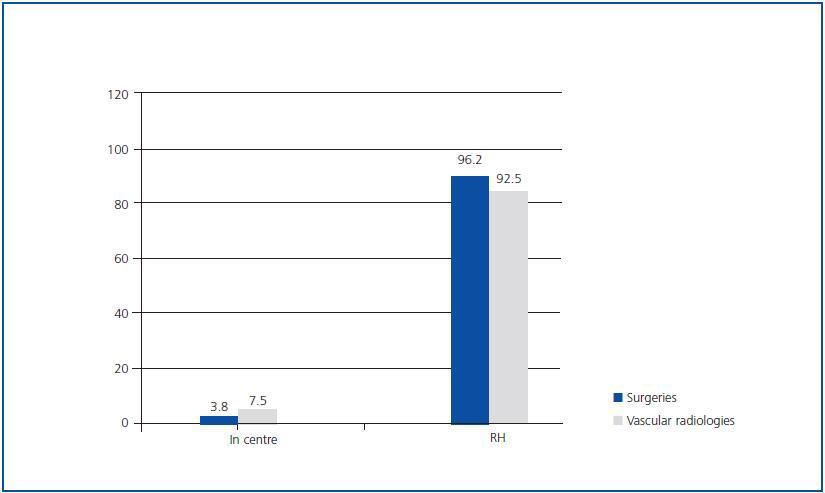
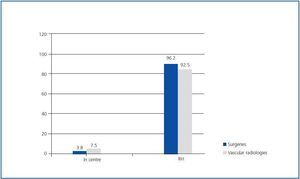
Figures 2 and 3 show the capacity for making decisions related to surgery and vascular radiology, with regard to the centres in both surveys. This is taking into account that decisions regarding such surgeries are made in the private centres in those cases where it is possible to refer the patient to a private department of surgery or vascular radiology, authorised by agreement.
Management of transplant waiting list
35% (N = 28) of centres control transplant waiting lists themselves (decisions regarding adding patients to the list, requesting tests, etc.), while in 65% (N = 52) of centres, these are managed by the RH. According to 81.4% of hospitals, a centre can intervene on a decision regarding whether to include a patient on the transplant waiting list, and 55.5% of hospitals allow for the requesting of supplementary tests necessary for transplant.
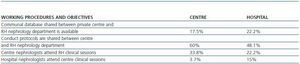
Working procedures and objectives
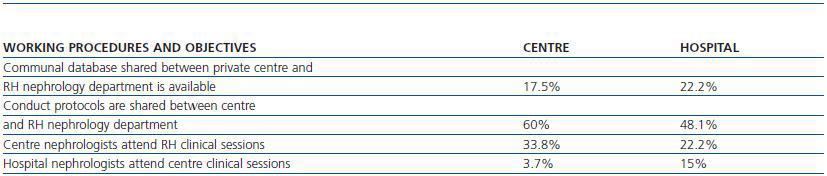
Table 5 illustrates features of the links between centres and hospitals with regard to working procedures and objectives. 72.5% (N = 58) of centres share protocols with other clinics in the same dialysis company. These protocols are designed by staff who work in the centres in 81.2% (N = 65) of cases.
44.4% (N = 12) of hospitals report sharing common objectives with the centres.
Research in private centres
70.3% (N = 19) of RHs report that they involve centres in clinical studies, and 32.5% (N = 26) of centres report that research is performed by and within their own centre. With regard clinical studies in centres, 62.5% (N = 50) participate in clinical studies together with the RH: of these, the RH is the principal investigator in 53.7% (N = 36) of cases and the centre is the principal researcher in 46.3% (N = 31).
Training in private centres
Regarding the training of nephrologists in private centres, 58.8% (N = 47) report that the parent company provides training: in 31.3% (N = 25) of cases this training takes place within working hours and counts as time spent working, and in 67.5% (N = 54) attendance to conferences or meetings is allowed. In the case of a request to attend courses or conferences, in 63.7% (N = 51) of centres the company allows for the necessary days, and in 36.2% (N = 29) the staff member is required to make up the days or take them as leave. In 21.2% (N = 17) of cases the company makes a partial or total contribution towards the attendance to courses/conferences.
DISCUSSION
The SEN is interested in homogenising the monitoring of renal patients. Hence the publication of distinct guidelines for clinical conduct, including that of HCs,3 and a push for the creation of guidelines and standards of care in haemodialysis by the SEN Quality Control Group,4 which has significant private centre representation.5 This task is more complicated when it comes to the dialysis patient. The existence of different dialysis companies, with centres located in different cities with different RHs and distinct conduct criteria based on the existing public health agreements, which themselves differ among the various Autonomous Communities, creates additional factors in the task of monitoring renal patients. To ensure adequate continuity of care for patients who receive dialysis outside the hospital setting, a satisfactory link between RHs and private HCs is fundamental.3 This study describes, for the first time, certain features of this link.
One of the limitations of this study is the low response rate, particularly from RHs; however, this is similar to other comparable Spanish studies based on surveys.2,6,7 This low response rate could have been due to the fact that the questionnaire involves time and effort, and that participation was voluntary and did not result in any practical or individual benefits. However, the questionnaire was distributed solely via the SEN mailing list, meaning that it is possible that some centres did not receive it. We believe that the results of this study, although not representative of the entire Spanish nephrological community, illuminate problems which should be understood and discussed. Indeed, the small number of hospitals which responded possibly corresponds to those with the closest links to private dialysis and their own responses; therefore they are not representative of all hospitals. Meanwhile, due to the survey being anonymous, we are unable to compare responses from centres linked with specific hospitals, although this was not one of the aims of this article.
The majority of private HCs in the country are located outside of hospitals, and most of these are run by multinational companies. Almost three quarters of centres employed nonnephrologist staff, most likely due to the scarcity of nephrologists available for these positions. Faced with a balanced supply and demand for public health institutions, work in a hospital becomes more attractive to new specialists (even partial contracts or as interns for a short while), since this is their most familiar environment and one which holds better prospects for promotion. The hiring of non-specialist staff means that, in a high percentage of cases, a guiding relationship exists between specialist nephrologists and nonnephrologist doctors employed in haemodialysis units. In some cases this is owing to the limitations imposed by the agreement, which stipulates that a qualified nephrologist should be the one responsible for prescription of treatment and monitoring of patients, even though the non-nephrologist doctor may have many years of experience working in a centre.
Almost 40% of HC nephrologists maintain a link with the RH in the form of shift working, and a small percentage perform other tasks within the hospital (external consultations, hospitalisations, research, etc.), despite the existence of a national incompatibility law which prohibits this.8
This law dates from 1984 and has not been altered since this time. However, and in spite of this, a position of ¿certain tolerance¿ exists on the part of some public health administrations, which allow nephrologists working in private centres to perform shifts in public hospitals, as this survey reflects. This situation does not apply to all the Autonomous Communities and we understand that this is a topic which should be further investigated, since the creation of an exception in the field of nephrology would, on the one hand, given the ageing personnel, allow for the growing need in public hospitals to be covered by young staff performing night shifts and, on the other hand, contribute to improving the continuity of care for HCs and the link between the two sectors. During times when there is a shortage of specialists, this law, in the areas in which it applies, creates competition between the two sectors which benefits neither side and does not provide for the overall care of renal patients.
Over 75% of nephrologists who work in centres are unaccompanied during their entire working day and 40% do not meet with colleagues during their shift. This situation, which is fundamentally due to the strict optimisation of human and economic resources, results in a decline in communication between colleagues, a decline in consensus and homogeneity of conduct (although this is currently minimised in the majority of centres through the application of norms and procedures),9 a feeling of isolation at work, and an overload of care which it would be advisable to reduce. However, this could mean a lack of fairness for patients in centres where a non-nephrologist doctor is in charge of care, due to a lack of nephrological experience when compared with HCs managed by nephrologists. This issue becomes worse if, in these centres, there is no overlap in working hours to enable doctors to consult with one another, or if the centres are not supervised by nephrologists. These principles, based on efficiency (the best post-effectiveness) and fairness (equality of opportunity),3 and indicated by the SEN in their Guidelines for Haemodialysis Centres, should be guaranteed for all patients.
Decisions made in each centre are largely the responsibility of nephrologists, thus they enjoy a certain level of freedom o operate. However, it is worth noting the increased percentage of supervised cross-consultations by hospital nephrologists, when it is not them who directly make the request for consultation. It is possible that this demonstrates, in some way and in some cases, a certain underestimation or lack of confidence in the work of HC nephrologists by their hospital colleagues. This is something which should without doubt be improved. Similarly, direct contact with other specialists or hospital departments improves and speeds up patient care, as well as the integration and fulfilment of professionals working in HCs. This can already be seen in some centres where this type of relationship between HC and RH has been attained.
In general, a good relationship and level of communication between HCs and RHs seems to exist, subjectively better for RHs than for HCs, although this feedback could be due to the fact that the RHs who responded to the survey were those most involved with their linked private centres.
There are still more than a quarter of centres where patients are not adequately referred from RH to HC and important data, such as up-to-date serologies, is missing. Note the discrepancy in responses between centres and hospitals: whereas RHs report referring 100% of cases along with reports and up-to-date serology, only 65% of centres report receiving patients with this data. This discrepancy could reflect a lack of self-assessment on the part of RHs, who have detailed in their responses what ¿should¿ occur rather than what occurs in reality. Alternatively it could be that there is a bias, and the RHs who responded to the survey are, probably, those most involved with the HCs, and many of those who did not respond to the survey are those who do not refer their patients to centres along with duly completed reports and serologies. This explanation could also account for other discrepancies found in the survey, such as prior telephone notice on discharge or discussion of admissions.
There is also a significant discrepancy with respect to initial vascular access, which, according to the RHs, is performed on 88.8% of patients, and in centres where this procedure occurs, it is performed on 51.3% of patients. The figures are similar with regard to urgent revisions of VAs (70% according to RHs and 38.7% according to centres). In this case it is necessary to bear in mind that, as has been pointed out before, some autonomous community agreements allow private centres to perform vascular accesses.
Part of the relationship between RH and HC is based on good will and respect, on the part of both HC and RH nephrologists. The majority of HC nephrologists have the option of maintaining contact with the RH and following up on their patient, either directly or via telephone, when they are admitted, and this is the case in more than 80% of incidences. Even so, up to 21% do not maintain this relationship, instead waiting for the arrival of medical reports to find out the outcome for their patient. Responsibility for the relationship between RH and HC lies with both parties: both the centre and the RH need to have an approachable attitude. Respect for the HC from the RH is reflected in the fact that 41% of centres report having been consulted on occasions by the RH in relation to making decisions regarding recently admitted inpatients. Centre nephrologists can provide valuable information to the hospital with regard to patients with whom they have a close and long-term relationship, and this communication can lead to patient benefit. In many cases centre nephrologists have valued, together with the patient and even the patient¿s family, a more conservative approach with respect to a situation where there is great risk to the patient. In some cases they may be aware of, or even be able to provide, signed documents detailing the patient¿s advance wishes.
One of the objectives that we wished to establish is that all outpatient units strengthen their links with the hospitals upon which they depend. The existence of both clinical and research links are fundamental to the improvement of quality of care within centres, and encourage professionals to work in centres.10 It is clear that this percentage does not reflect the majority. Indeed, it does not account for even half of centres, but could be a starting point for further research and may hold value as an opportunity for improvement in centres and hospitals which do not act in this way.
Table 1. General centre features (N = 80 centres)
Table 2. Manner of referring patients between centres and hospitals for hospital admission, and referral
from hospital to centre on patient discharge
Figure 1.
Table 3. Management of cross-consultations with specialists and of medication supply to centre
Table 4. Management of vascular accesses
Figure 2.
Figure 3.
Table 5. Relationship between centres and hospitals in working procedures and objectives