In recent years in the scientific community, the harmful effect of a phenolic type of environmental toxicant, known as bisphenol A (BPA), has achieved great relevance (Fig. 1). The interest in this compound is increasing owing to its possible adverse effects on several organs, which has led several organisations to recommend the prohibition or at least use reduction, with wide repercussions in the media. BPA has also aroused interest in the nephrological community, as it has been linked to kidney and endocrine disorders. Since BPA is cleared by the kidneys, plasma and tissue levels of BPA are markedly increased in patients with impaired renal function.
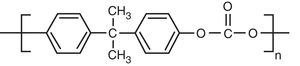
But what is bisphenol A and why does it arouse such interest? The significance of BPA stems from its ubiquity, because it is a compound that is found in the most commonly used plastic containers (polycarbonates) and epoxy resins in packaging. BPA is released from these plastic containers and it is absorbed by humans that consume food or liquid that is being stored in these containers. BPA was synthesised in the 1930s as a synthetic oestrogen,1 and was subsequently replaced by diethylstilbestrol.2 It is converted into a monomer during the manufacture of various commonly used products, such as plastic bottles, baby bottles or contact lenses. BPA-containing epoxy resins are used as a coating in cans used for food, although there is now a tendency to be substituted by polyesters.3 Given the widespread use of BPA, its potential risk to human health as a synthetic oestrogen for daily consumption has been a topic of debate in regulatory agencies for many years.
BPA generally passes into the bloodstream through the oral route, usually accompanying the products contained in the plastic containers. It is immediately absorbed (5–20min) and has a bioavailability greater than 70%.4,5 As with phenols produced by gut bacteria, BPA is conjugated in the intestine and liver with glucuronic acid and is eliminated almost exclusively in the urine.6 Exposure in ways other than the oral route may also occur, and so it is considered an environmental toxic, e.g. by inhalation (this may cause cough, asthmatic attacks and bronchospasms); eye exposure (causing swelling around the eyes, facial pruritus and conjunctivitis) or skin exposure (redness and roughness).
However, more controversial is its role as an endocrine agonist after prolonged constant exposure for many years. BPA is commonly referred to as an endocrine “disruptor”. Despite the evidence published,7 the European and American authorities consider that, because it is eliminated rapidly, BPA may be considered as a relatively safe compound. Daily oral and cutaneous exposure to bisphenol has recently been estimated to be 0.2–0.3mg BPA μg/kg of weight.8
In the absence of conclusive scientific evidence, it is recommended to reduce exposure as much as possible,9 with maximum safety levels of 5mg/kg/day in adults. However, following a precautionary principle, baby bottles and rubber nipples were banned throughout the EU from June 2011 onwards, since much greater potential harm has been observed in newborns.
The reasons why a more widespread ban has not been imposed are based on the following:
- •
High economic cost of completely eliminating the containers currently used.
- •
The strongest evidence has been seen in animals, with limited information of toxicity in humans.
- •
Differences in the metabolism between laboratory animals and humans.
- •
Complete renal elimination immediately after ingestion.
However, other authors support the elimination of its industrial use due to the increasing amount of evidence on the association of BPA exposure with the development of diseases, both in laboratory animals and based on observational studies in humans.
Evidence in animal testingThere are direct data on BPA's toxicity in laboratory animals. They include the following:
- a)
Effects on the reproductive system: In rats given high doses of BPA there is an increase in immature spermatozoa.10 The effects of BPA exposure in neonatal mice was different depending on the amount of BPA administered. At 2mg/kg, the weight of an adult prostate increases11 and at 10mg/kg, prostate development stops.12 In adult male rats, a dose of 10mg/kg increases the susceptibility of the prostate gland to develop hormonal carcinogenesis10 and sperm counts and testosterone levels are reduced, with a significant impact on fertility.13
- b)
Neurological effects: A study of developing zebrafish embryos showed that BPA may influence brain development, including the hypothalamus, telencephalon and preoptic area.14 Studies in rodents showed that perinatal or uterine-related BPA exposure can cause permanent changes in behaviour, including increased levels of aggression and anxiety, and changes in learning, memory, searching and emotional responsiveness.15 Several studies with mice concluded that exposure to low doses of maternal BPA has long-term consequences on neurobehavioural development.16 Also, neonatal BPA exposure may affect brain morphology, with sexual dimorphism and adult neuronal phenotypes.17
- c)
Effects on weight: Continued BPA exposure has lasting effects on body weight and adiposity.18 One study performed on rats showed that perinatal exposure to drinking water with 1mg/L of BPA increased adipogenesis in females at weaning.19
Many of the findings observed in laboratory animals have been confirmed in clinical studies.
- a)
Reproductive system and endocrine disorders. It has been observed that even very low concentrations of BPA are capable of producing changes in spermatogenesis20 and oestrogen production,21 pancreatic damage,22 thyroid problems23 or liver damage.24
- b)
Tumourigenesis. BPA exposure has been associated with the appearance of neuroblastomas and breast tumours.25
- c)
Neurological effects. In a subgroup of young children, prenatal BPA exposure may be associated with an increase in hyperactivity and aggressiveness.26
- d)
Obesity and diabetes. BPA exposure has been associated with the onset of obesity,27 insulin resistance and diabetes,14,28,29 and BPA inhibits the release of adiponectin.30
- e)
Cardiovascular disease. In recent years, numerous studies have related this compound with various abnormalities in the cardiovascular system, such as arrhythmias, by binding to calcium channels,31 and an increase in cardiovascular risk. For every increase of 4.5mg/L of BPA in urine, the increase in the incidence of coronary disease goes up by 13% over a 10 years’ time.32 But it cannot be ruled out that this increase may be due to other cause since that the negative effect of BPA was lost after adjusting for traditional cardiovascular risk factors. it is likely that blood pressure is influenced by BPA. In healthy adults in the United States, urinary BPA levels greater than 4g/L have been associated with a 50% increase in the prevalence of hypertension as compared with urinary BPA levels <1.5mg/L.33 Recently, the relationship between BPA and vascular damage has been reviewed by Bosch et al.34Table 1 summarises some of the most relevant articles.
The relationship of BPA to kidney disease merits a separate chapter, given that, in this case, not only is it a compound that plays a direct role in kidney damage, but it is also cleared mainly in urine; therefore it accumulates in these patients.
The greater the decrease in glomerular filtration, the lower the rate of elimination of BPA in urine. Thus, patients on haemodialysis are not able to clear BPA,35 and there is a strong correlation between BPA accumulation and impaired renal function.36 However, the 2003–2006 National Health and Nutrition Examination Survey (NHANES III), with a sample of 2573 patients, also found a decrease in the elimination of BPA in relation to the level of impairment in renal function, although it was only significant in women.37 Only few studies have measured the plasma concentration of BPA in renal patients; Krieter et al.38 observed a correlation between the impairment in renal function and plasma concentrations of BPA, regardless of gender. In CKD stages 1–2, the levels are similar to healthy controls and below the levels of detection used (<0.2ng/mL), and in stages 3–4 patients the levels of BPA rise sharply, to 0.7±1.0ng/mL. In stage G5 the values are up to 1.6±1.8ng/mL (p<0.05), while in G5D the values were 10.0±6.6ng/mL. Although it is known that chronic kidney disease decreases urinary excretion, the pharmacokinetics, bioavailability and tissue accumulation in humans are not known.
Among the evidence that points to a possible causal role in kidney disease is the fact that in healthy adults, urinary BPA levels >1.4mg/L are associated with a 23% higher risk of microalbuminuria than in adults with levels <0.5mg/L37 and in children.39 It has also been associated with low-grade albuminuria in Chinese adults.40 The suggested possible mechanisms of BPA-mediated nephrotoxicity include increased oxidative stress, inflammation and induction of hypertension.41,42
It has also recently been reported that serum BPA may be a predictor of kidney disease progression in patients with Type 2 Diabetes,43 such that patients with elevated plasma levels of BPA experience greater kidney disease progression. Table 2 lists the principal publications that relate BPA exposure and kidney damage.
Significance of bisphenol A in nephrology. Main publications relating the effects of BPA on the kidneys, impaired elimination or its relation to dialysis.
| BPA in urine and microalbuminuria | Urinary BPA>1.4mg/L: A 23% increase in albuminuria | Li et al., Kidney Int, 201440 |
| BPA in urine and microalbuminuria in children | Increase of 0.28mg/g and MA per unit of urinary BPA | Transande et al., Kidney Int, 201339 |
| BPA podocytopathy in laboratory animals | BPA ip 50mg/kg induces proteinuria, glomerular hyperfiltration and podocytopenia | Olea-Herrera et al., Cell Physiol, 201441 |
| BPA and hypertension | The NHANES study found a correlation between BPA and HTN | Shankar et al., J Environ Public Health, 201233 |
| BPA and progression of type 2 DM | Serum BPA correlates negatively with GF (OR: 6.65) | Hu et al., Acta Diabetológica, 201543 |
| BPA and renal function | Serum BPA: inverse correlation with GF | Krieter et al., Artif Organs, 201338 |
| Serum BPA increases in HD | 15 patients on HD saw elevated BPA with PS | Murakami et al., Blood Purif, 200736 |
| Serum BPA is affected by the type of dialyser | In 69 patients on HD (crossover study), BPA increased with PS and decreased with PN | Bosch, J Am Soc Nephrol, 201547 |
| Serum BPA was associated with inflammation and oxidation in HD | BPA and dialyser fibres with BPA increased inflammation and oxidation in mononuclear cells | Bosch, J Am Soc Nephrol, 201547 |
GF: glomerular filtration; HD: haemodialysis; MA: microalbuminuria; PN: polynephron; PS: polysulfone; Urinary BPA: bisphenol in urine.
However, it is the accumulation of this substance in patients with decreased glomerular filtration that has motivated the analysis of the compound as a possible uraemic toxin.44 One of the arguments put forward by the various Official Agencies for considering the use of BPA in ordinary consumption to be safe is its almost complete elimination in urine as a conjugated compound.45 Therefore, patients with kidney damage, in whom elimination is impaired, should be considered a population especially susceptible of the potential adverse effects of BPA exposure.
BPA in patients on dialysisPatients on haemodialysis are particularly susceptible to the risk of toxicity due to BPA, as renal elimination is completely impaired. This is further exacerbated in patients on haemodialysis, since BPA, being a ubiquitous component, is part of the composition of the plastic material of some dialysers and commonly used dialysis systems, in the form of polycarbonate in the casings and in multiple dialysis membranes, such as polysulfone (PS) or polyester-polymer alloy (PEPA).
In these dialysers, the polymer is in constant contact with the blood and it may be released into the circulatory system, so that the increase of BPA in haemodialysis patients may be due not only to environmental exposure, but possibly also to the method itself.46 Several studies have reported that effluents from dialysers made of these materials have higher concentrations of BPA,36,44,45 with increased BPA migration when blood is used instead of saline.46 Therefore, in these patients it is very difficult to determine whether the plasma concentrations exceed recommended levels.
Despite all this information, there are practically no long-term prospective studies that relate haemodialysis to the presence of BPA and its possible effects. In 2013, Krieter et al.38 studied the effect of haemodialysis on BPA over a 4-week period and concluded that the differences between membranes with bisphenol (polysulfone) and without bisphenol (polynephron) were not significant. However, the fact that the casings of all the dialysers used contained BPA and the short duration of the study might explain that the values of BPA were not different.
To evaluate this discrepancy between in vitro studies or studies in a single session and Krieter's results, we have recently published (Bosch-panadero et al.47) a longer-term study (3 months); this is a crossover study of 69 patients, comparing dialysers with BPA (polysulfone) and without BPA (polynephron), we found that serum and intracellular levels of BPA increased with the use of polysulfone (48.8±6.8 to 69.1±10.1ng/mL), and decreased with dialysis with polynephron (70.6±8.4 to 47.1±7.5ng/mL; p<0.05). The increase in BPA were associated with elevated levels of intracellular free radicals and circulating inflammatory markers (IL-6, TNF-α, C-reactive protein). It was also observed in in vitro experiments using circulating cells that BPA polysulfone membranes released bisphenol into the culture medium and resulted in the increased production of cytokines in lymphocytes in culture.47
Regarding haemodiafiltration, there are currently no well-designed studies to determine the effect of this technique on the elimination of BPA. Although it would be expected better elimination with haemodiafiltration, the reinfusion of fluid used circulates by BPA membranes, which may increased the infusion of BPA.
Lastly, in the case of peritoneal dialysis, there is only one study that looks at the impact of BPA, which found that its concentration in dialysis fluid is well below the permitted value. Although only 4 patients were studied, levels only seemed to increase in one of them, so the authors conclude that BPA does not appear to be reduced or increased by peritoneal dialysis.48
Some considerations regarding bisphenol in nephrologyCan BPA be considered an uraemic toxin? Do serum and tissue levels increase in chronic kidney disease? We know that patients with kidney disease have elevated serum levels of BPA and that some of the effects of BPA in laboratory animals also appear in uraemic patients on haemodialysis, but it is not known whether there is a direct relationship. It is not yet known whether removing BPA from the material and the solutions will solve signs and symptoms associated to BPA. Our study47 showed how the use of membranes with BPA increases serum and intracellular levels of BPA in haemodialysis patients. There was no correlation with time on dialysis, and there was also high variability among the different individuals, which may suggest that there the metabolisation process is not uniform in all patients. BPA may be responsible, at least in part, for the increase in the inflammatory markers and oxidation observed in these patients. However, it seems appropriate, as recommended by FDA in other situations, to attempt to reduce BPA exposure as much as possible, as it seems likely that it may be considered to be an exogenous uraemic toxin with possible clinical implications.
Recent evidence has led the Scientific Committee on Emerging and Newly Identified Health Risks commissioned by the European Union to issue in early 2015 a report entitled “Final opinion on the safety of the use of bisphenol A in medical devices”, in which they conclude that there is a risk of adverse effects from BPA when it is “available for systemic exposure after non-oral exposure routes, especially for neonates in intensive care units, infants undergoing prolonged medical procedures and for dialysis patients”,49 and they therefore recommend limiting its use whenever possible and emphasise that the beneficial effects of the material used (rigidity, durability, etc.) do not exceed the potential risk of BPA.
The decrease in the urinary elimination of BPA in patients with chronic kidney disease, in the stages before dialysis, should lead to specific studies to determine whether this population should be considered, together with newborns, as an at-risk population in terms of environmental exposure to this compound.
Conflicts of interestThe study published by our group mentioned in the text was funded by a research grant from Nipro Corporation (Bosch et al. JASN 206). The sponsors had no influence in the design, the interpretation of the results or the drafting of the manuscript.
The Kidney Disease and Diabetes Research Group (IIS-FJD) is funded by the following agencies: Health Research Fund (PI14/00386; PIE13/00051 and PI16/01298), the Spanish Society of Nephrology (SENEFRO) and Fundación Renal Íñigo Álvarez de Toledo (FRIAT).
Enrique Bosch, Alberto Ruiz-Piego, Esther Civantos and Sebastián Mas, of the Kidney Disease, Vascular Disease and Diabetes Laboratory, Fundación Jiménez Díaz, Madrid.
Didier Sanchez-Ospina, of the Dialysis Unit, Fundación Jiménez Díaz and Fundación Renal Iñigo Álvarez de Toledo, Madrid.
Vanesa Camarero, Isabel Saez-Calero and Pedro Abaigar, of the Nephrology Department, Complejo Hospitalario de Burgos, Burgos.
Vanesa Pérez-Gómez, Alberto Ortiz, Jesús Egido and Emilio González-Parra, of the II-S Nephrology and Hypertension Department, Fundación Jiménez Díaz, Universidad Autónoma, Madrid.
Please cite this article as: Mas S, Egido J, González-Parra E. Importancia del bisfenol A, una toxina urémica de origen exógeno, en el paciente en hemodiálisis. Nefrologia. 2017;37:229–234.