Peritoneal dialysis (PD) is an underutilized form of renal replacement therapy. Although a variety of factors have been deemed responsible, timely insertion of a PD catheter may also be a contributory factor. Furthermore, a good catheter implantation technique is important to allow for effective peritoneal access function and long-term technique survival. Studies regarding results obtained by nephrologists in comparison with surgeons have been limited to small single-center experiences. Thus, the objective of this study was to explore the impact of the peritoneal dialysis (PD) catheter insertion by nephrologists compared to surgeons on early catheter complications and on technique survival. We also examine whether PD catheter insertion by nephrologists has a positive impact on the growth in the number of patients using PD. We performed 313 consecutive procedures: 192 catheter insertions and 121 catheter removal from January 1, 2006 to December 31, 2013. The main reasons for catheter removal were: renal transplantation, 52 (43%) follow of transfer to HD, 48 (40%) and catheter malfunction, 16 (13%). The patients were mostly male (63.4%) with the mean age of 50.8±15.1 years and 23.8 were diabetics. We only observed seven (2.5%) early complications (<4 weeks) associated to peritoneal catheter surgery (3 peritonitis episodes, 2 hemoperitoneum episodes, one complicated hernia and one omental entrapment). There were not significant differences in surgery-related complications in both periods. The penetration ratio of PD after 2006 was 117% higher compared with procedures performing before this date. In conclusions, we have demonstrated a positive impact on the growth of the PD population when catheter insertion is performed by nephrologists with a minimal incidence of complications associated.
La diálisis peritoneal (DP) es un tipo de tratamiento de reemplazo renal infrautilizado. Aunque ello se debe a múltiples factores, la inserción puntual de un catéter de DP también puede ser un factor coadyuvante. Más aún, una buena técnica de implantación del catéter es importante para posibilitar una función de acceso peritoneal eficaz y facilitar la continuidad de la técnica a largo plazo. Los estudios sobre los resultados obtenidos por nefrólogos en comparación con los de los cirujanos se han limitado a pequeñas experiencias de centro único. Por ello, el objetivo de este estudio fue analizar el impacto de la inserción del catéter de diálisis peritoneal (DP) por nefrólogos en comparación con el de los cirujanos cuando surgían las primeras complicaciones con el catéter y en relación con la continuidad de la técnica. También examinamos si la inserción del catéter de DP por nefrólogos tenía un impacto positivo en el aumento del número de pacientes con DP. Llevamos a cabo 313 procedimientos consecutivos: 192 inserciones de catéter y 121 extracciones de catéter entre el 1 de enero de 2006 y el 31 de diciembre de 2013. Las principales razones para la extracción del catéter fueron: trasplante renal, 52 (43%), seguido por transferencia a hemodiálisis (HD), 48 (40%) y funcionamiento defectuoso del catéter, 16 (13%). La mayoría de pacientes era de sexo masculino (63,4%) con una media de edad de 50,8±15,1 años y 23,8 eran diabéticos. Sólo observamos 7 (2,5%) complicaciones tempranas (<4 semanas) asociadas con cirugía de catéter peritoneal (3 episodios de peritonitis, 2 episodios de hemoperitoneo, una hernia complicada y un atrapamiento omental). No hubo diferencias significativas en las complicaciones relacionadas con la cirugía en ambos períodos. La tasa de penetración de la DP desde 2006 fue el 117% superior a la de aquellos procedimientos que se habían llevado a cabo antes de esa fecha. Resumiendo, hemos demostrado que existe un impacto positivo en el aumento de la población con DP cuando los nefrólogos realizan la inserción del catéter con una mínima incidencia de complicaciones asociadas.
The increasing prevalence of end stage renal disease over recent years has led to an increased number of both dialysis access procedures, that is hemodialysis (HD) and peritoneal dialysis (PD), as well as an important extra workload for those interventional nephrologists, radiologists or surgeons involved.1,2 Providing an optimal dialysis access care is very important in patients starting renal replacement therapy because the patient's outcome depends on the access procedure survival, especially in patients starting peritoneal dialysis.3,4 The outcome of the access care provided by nephrologists as well as the procedures they perform are comparable to those provided by surgeons and radiologists.4–6 The exact proportion of procedures currently performed by nephrologists is unclear, although it is known to be increasing since the establishment of the American Society of Diagnostic and Interventional Nephrology in 2000.7-9 In addition there is little information comparing the severe complications of the procedure performed by surgeons versus by nephrologists. The aim of our study was to describe the impact of interventional nephrologists on the growth of a peritoneal dialysis program in a regional center and compare life-threatening complications between both procedures.
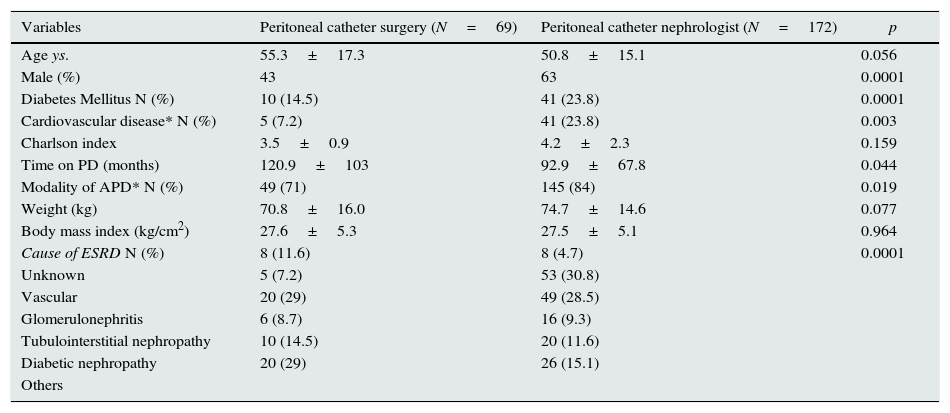
Material and methodsThis is a study purely descriptive of our daily clinical practice when starting PD catheter procedure in our Nephrology unit. In our PD program, catheter surgery was undertaken by surgeons until 2006. Thereafter up to date, the nephrologists have performed catheter surgery. Our center is a third-level hospital, which attends population of Malaga province (the province has 1,600,000h). The PD and HD incidences during both periods (<2006 vs. >2006) were 5.6% (n=69) vs. 94.4% (n=1169) respectively before 2006 and 11.5% (n=172) vs. 88.5% (n=1322) respectively after 2006 (p=0.0001). A total of 313 consecutive procedures were carried out by the same team interventional nephrologists in the Carlos Haya Regional Universitary Hospital (Málaga, Spain). Table 1 depicts demographic and clinical characteristic of our patients who started PD before and after 2006. We used a dissection technique similar to that previously used by surgeons: tissue layers are dissected and separated under direct vision through a minimal parietal peritoneum dissection without the use of trocar devices. The hospital provides an operating room in order to carry out the technique. Patients are admitted and discharged from hospital on the same day provided there are not relevant clinical complications such as fever, severe abdominal pain, or they have to travel a long distance.
Clinical characteristics in patients with peritoneal catheter placement by surgeon (before 2006) versus by interventional nephrologist (after 2006).
| Variables | Peritoneal catheter surgery (N=69) | Peritoneal catheter nephrologist (N=172) | p |
|---|---|---|---|
| Age ys. | 55.3±17.3 | 50.8±15.1 | 0.056 |
| Male (%) | 43 | 63 | 0.0001 |
| Diabetes Mellitus N (%) | 10 (14.5) | 41 (23.8) | 0.0001 |
| Cardiovascular disease* N (%) | 5 (7.2) | 41 (23.8) | 0.003 |
| Charlson index | 3.5±0.9 | 4.2±2.3 | 0.159 |
| Time on PD (months) | 120.9±103 | 92.9±67.8 | 0.044 |
| Modality of APD* N (%) | 49 (71) | 145 (84) | 0.019 |
| Weight (kg) | 70.8±16.0 | 74.7±14.6 | 0.077 |
| Body mass index (kg/cm2) | 27.6±5.3 | 27.5±5.1 | 0.964 |
| Cause of ESRD N (%) | 8 (11.6) | 8 (4.7) | 0.0001 |
| Unknown | 5 (7.2) | 53 (30.8) | |
| Vascular | 20 (29) | 49 (28.5) | |
| Glomerulonephritis | 6 (8.7) | 16 (9.3) | |
| Tubulointerstitial nephropathy | 10 (14.5) | 20 (11.6) | |
| Diabetic nephropathy | 20 (29) | 26 (15.1) | |
| Others |
The patients are administered an enema the day before the procedure. On the day of the surgery they are asked to empty their bladders prior to being taken to the operating room. Patients are also given 1g of cefazolin IV prior to the operation. Most procedures are performed under local anesthesia and sedation. Sedation is administered by the nephrologist with the aid of a nurse. The level of sedation is titrated in order to achieve moderate sedation, where the patient is still able to respond and cooperate with the physician performing the procedure when asked to but is semi-asleep otherwise. We also use intravenous desmopresin before the procedure to reduce the bleeding risk as previously reported.10 We mostly use Swan-neck Tenckhoff catheters. In addition, we use tungsten catheter if there is a risk of catheter migration e.g. obese patients. The skin is prepared with povidone iodine and the abdomen is draped as per the abdominal surgery protocol. Lidocaine 2% is infiltrated into the skin as local anesthetic.11
ResultsFrom January 1, 2006 to December 31, 2013 we performed 313 consecutive procedures by nephrologist team: 192 catheter insertions and 121 catheter removals. Patients are admitted and discharged from hospital on the same day. Only two patients have been discharged on the day after the procedure (one because of discomfort and the other because of a long journey home. We used Swan-neck Tenckhoff catheter in all patients. We only used tungsten catheter in two obese patients without any early or late complications. One catheter insertion was made by surgeon team due to simultaneous repair of an inguinal hernia.
Likewise, from January 1, 1996 to December 31, 2005 catheter surgery was performed by surgeon team. Clinical characteristics in patients with peritoneal catheter placement by surgeon versus by interventional nephrologist are shown in Table 1. Swan-neck Tenckhoff catheter was used in all patients during this period.
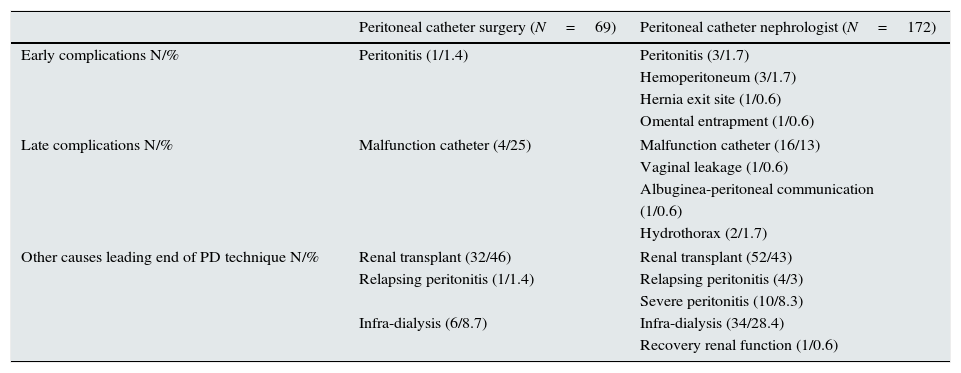
Surgery complicationsTable 2 shows the reasons for catheter removal in patients with peritoneal catheter placement by surgeon versus by interventional nephrologist including procedure-related perioperative complications and complications associated with PD technique. After 2006 we observed seven (2.5%) early complications (<4 weeks) associated with peritoneal catheter surgery: 3 peritonitis episodes, which resolved with antibiotic treatment; 2 hemoperitoneum episodes (one resolved spontaneously but the other required exploratory laparotomy by surgeons); and one complicated hernia through peritoneal catheter exit site and one omental entrapment (both required surgeon intervention by surgeon team). We experienced no episodes of bowel perforation. Finally, other life-threatening complications related to insertion catheter were not observed in our patients during follow-up. Before 2006 one peritonitis episode was observed associated with peritoneal catheter procedure, which resolved with antibiotic treatment.
The reasons for catheter removal of patients who started PD before 2006 versus after 2006.
| Peritoneal catheter surgery (N=69) | Peritoneal catheter nephrologist (N=172) | |
|---|---|---|
| Early complications N/% | Peritonitis (1/1.4) | Peritonitis (3/1.7) |
| Hemoperitoneum (3/1.7) | ||
| Hernia exit site (1/0.6) | ||
| Omental entrapment (1/0.6) | ||
| Late complications N/% | Malfunction catheter (4/25) | Malfunction catheter (16/13) |
| Vaginal leakage (1/0.6) | ||
| Albuginea-peritoneal communication | ||
| (1/0.6) | ||
| Hydrothorax (2/1.7) | ||
| Other causes leading end of PD technique N/% | Renal transplant (32/46) | Renal transplant (52/43) |
| Relapsing peritonitis (1/1.4) | Relapsing peritonitis (4/3) | |
| Severe peritonitis (10/8.3) | ||
| Infra-dialysis (6/8.7) | Infra-dialysis (34/28.4) | |
| Recovery renal function (1/0.6) | ||
Since we started performing peritoneal catheter surgery our PD program has increased significantly. The mean catheter peritoneal insertions per year were higher after 2006 compared with prior to 2006 (22.6±5.3 vs 10.4±3.9; p=0.0001).
DiscussionInsertion of peritoneal catheter performed by an interventional nephrologists team is a very procedure with a very low incidence of surgical complications and lower sanitary costs compared to surgery performed by surgeons.
The number of patients on PD remains low, despite several advantages as compared to HD such as preservation of residual renal function, improved middle molecule clearance, improved fluid and blood pressure control, less likelihood of severe cardiac arrhythmias, reduced mortality (at least in the first years of PD),12 a lower requirement for erythropoietin stimulating agents, a lesser risk of viral transmission, cost-effectiveness and better quality of life and better physician–patient relationship.13,14 However, one of the main pitfalls concerns the availability of a suitable permanent peritoneal catheter. In fact, catheter-related complications currently are currently the second leading cause of technique failure.14 Another problem is the lack of experience and training on catheter implantation during nephrology fellowship programs, or a lack of interest (or time) by nephrologists in these procedures.5–15 Consequently, in most centers PD catheter surgery is usually performed by surgeons. Disadvantages arising from this relate to the lack of surgical teams interested in PD catheter insertion, as it is considered less important than other practices.12 This invariably results in an inherent delay that involves potential patients exposure to HD and loss of interest in PD while waiting for the catheter insertion to be performed, as well as potential increase in complications associated with the catheter placement.4,13 Centers where nephrologists have taken on this surgery have reported better results in terms of complication rates and technique survival, as well as an increase in PD penetration.6,14 In any case, an experienced surgeon should remain essential to treat any possible severe life-threatening complications. Whether this may contribute to increase peritoneal dialysis program worldwide is undetermined yet. Further studies are needed to elucidate this concern.
This study has some limitations. Firstly, this is a study purely descriptive and conclusions should be taken with caution. Secondly, although our patient sample is short, the procedure is performed by the same team and technique which reduces complications and improves the results. Finally, we assume bias derived of retrospective data from patients starting PD before 2006.
In conclusion, since the key to a successful PD program is PD catheter survival, the timing and effective insertion of the peritoneal catheter, as well as prompt management of complications arising from catheter procedure are important factors to guarantee technique survival and consequently to increase the PD program. Improving and stimulating nephrologist's training seems necessary since, when these techniques are performed by nephrologists, there is a decreased incidence of complications, a reduced hospitalization cost, and increased autonomy and efficiency. Accordingly, a potential increase in PD program could be expected. However, the availability of an experienced surgeon remains essential to treat any possible severe complications.
Conflict of interestThe authors declare no conflict of interest.
This study was supported, in part, by the Instituto de Salud Carlos III and Fondos FEDER, RETIC REDinREN, RD12/0021/0015 grant ICI14/00016 and by grant PI-0590/2012 from the Consejería de Salud del Gobierno de Andalucía. The authors thank the Nephrology team from Nephrology Department (Carlos Haya Regional University Hospital) and the Regional Transplant Coordination of Andalusia and all participants in each center for their support in compiling information. We also thank Ian Johnstone for his linguistic assistance in the preparation of the text.