Objetivos: determinar la prevalencia y gravedad de hiperplasia gingival en un grupo de pacientes con trasplante renal (TR) y analizar el efecto del uso de los inmunosupresores ciclosporina A (CsA), tacrolimus (Tac), sirolimus (Siro) y azatioprina (Aza) o micofenolato de mofetilo (MMF) sobre esta complicación. Métodos: se clasificó la presencia y gravedad de la hiperplasia gingival. Se analizó el impacto de los medicamentos inmunosupresores, edad, higiene bucal, verapamilo y nifedipina sobre esta complicación mediante regresión logística múltiple. Resultados: fueron 172 pacientes. Usaban CsA 137, Tac 25, Siro 6, Aza 107 y MMF 56. Tuvieron hiperplasia gingival el 59,1% con CsA, 12,0% con Tac, y 16,7% con Siro. Aumentaron la frecuencia de hiperplasia gingival CsA con razón de momios (RM) 15,2, edad <45 años con RM 5,6 y mala higiene bucal con RM 3,2, y la disminuyeron Aza con RM 0,05 y MMF con RM 0,03. Conclusiones: Aza y MMF ofrecieron protección significativa contra el desarrollo de hiperplasia gingival en este grupo de pacientes con TR.
INTRODUCTION
The use of cyclosporin A or tacrolimus in kidney transplant patients is frequently accompanied by side effects.1 Oral Adverse effects are mainly cosmetic, but opportunistic fungal or viral infections may also flare up.2,3 The most common orallesion is the firm, lobulated enlargement of the gums known as gingival overgrowth (GO) or gingival hyperplasia, with reported prevalence as high as 74%,2-4 arising as a result of the interplay of several factors, including CyA and calcium channel blocker anti-hypertensive drugs use, gingival inflammation and poor oral higiene.4 Histologically, GO is marked by fibroblast proliferation, deposition of amorphous extracellular material and mononuclear inflammatory infiltrate.5 Tac - associated GO prevalence is much lower.6 There have been only a few literature reports on Sirolimus - associated GO.7
The aims of the study were to assess GO prevalence and severity in a group of KT patients using CyA, Tac or Siro as principal immunosuppressor drugs and to evaluate the effect of the following factors on GO prevalence: use of Aza or MMF as a secondary immunosuppressor drug, calcium channel blocker anti-hypertensive drugs, kidney graft function level, fasting glycemia, oral hygiene and age.
MATERIAL AND METHODS
It was a cross ¿ sectional study, carried out in the nephrology service outpatient clinic at HGZ # 50 IMSS, San Luis Potosí. The study was approved by the hospital¿s research and ethics committees. All participants were asked for permission to perform an oral examination, which included an evaluation of gingival overgrowth and oral hygiene. Consecutive KT cases attending nephrology consultation follow ¿ up were examined. The total group was split into cases using CyA, Tac or Siro as principal immunosuppresor drug. Demographic and clinical data was gathered from medical records, including cause of end stage renal disease before KT, elapsed time since transplant surgery, CyA, Tac and Siro doses and blood levels, use of MMF or Aza, use of Calcium channel blocker anti-hypertensives, and laboratory results. For GO diagnostic evaluation purposes, the dental arches were divided into sextants (three upper and three lower). GO severity was classified into four categories using the criteria established by Pernu et al.:4 score 0, no gingival overgrowth; score 1, slight overgrowth with thickening of marginal gum tissue; score 2, moderate gum overgrowth extending to half of the crown, and score 3, severe overgrowth, covering two thirds of the crown and affecting Inserted gum. Oral hygiene was classified as good, fair, or poor according to the simplified oral hygiene index,8 assessing amount and location of bacterial plaque on tooth crowns. We carried out a descriptive statistical analysis for the following demographic and clinical variables: sex, age, body mass index, cause of end stage renal disease before KT, elapsed time since transplant, medications used and clinical laboratory results. Continuous variables were compared using the Student t-test or ANOVA, and proportions using Chi2. Associations were analysed with Chi2 or multiple logistic regression as applicable, using Excel 2007 and Epi Info version 3.4.3. The multiple logistic regression model included independent variables potentially associated with GO, i.e sex, age, oral hygiene, CyA, Tac or Siro doses and blood levels, secondary immunosuppressor drug and doses, calcium channel blocker anti-hypertensive drugs, elapsed time since kidney transplant and diabetes. Variables with a value p > 0.50 were excluded from subsequent analyses. Values of p < 0.05 were considered statistically significant.
RESULTS
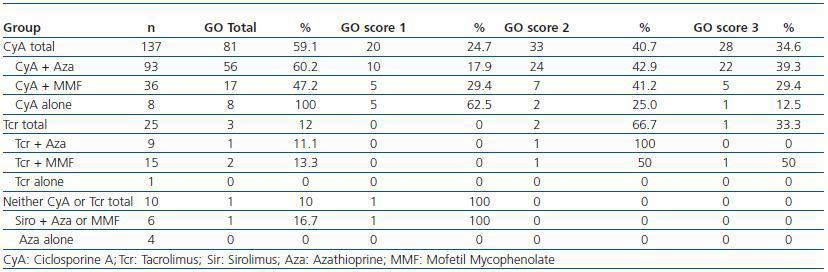
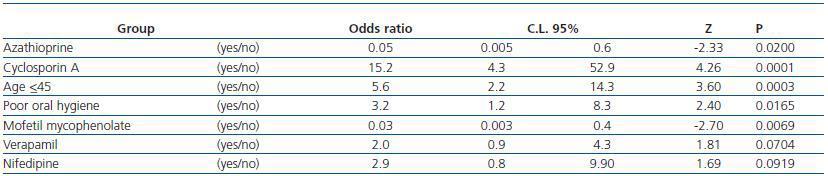
The study included 172 kidney transplant patients: 103 men and 69 women, aged 33.0 ± 13.7 (9 to 66) years; 48 (27.9%) had a primary-level education or lower. 19 patients (11.2%) were diabetic before KT and nine others (5.3%) had a fasting glycemia > 126mg/dl on lab results closer to oral examination date. Mean elapsed time post ¿ KT was 22 (1¿157) months. Ten patients were transplanted three or less months before oral examination. Serum creatinine was 1.4 ± 0.4 mg/dl, for an estimated glomerular filtration rate (Levey) of 66 ± 28ml/min. The principal immunosuppressor drug was CyA in 137 patients, Tac in 25, Siro in 6 and Aza in 4 (table 1). The secondary immunosuppressor was Aza in 107 cases, MMF in 56 and Siro in just one patient. Mean CyA and Tac doses were 3.0 and 0.016 mg/kg/day, Siro 2.0 mg/day, MMF 1.25 g/day, Aza 1.4 mg/kg/day and prednisone 0.14 mg/kg/day. Eight cases used CyA (plus prednisone) but not a secondary immunosuppressor, and ten used neither CyA or Tac. GO prevalence with CyA as the principal immunosuppressor was 59.1%, 12.0% with Tac, and 16.7% with Siro. Within the CyA group, GO prevalence was 60.2% for Aza, and 47.2% for MMF subgroups, p=0.18, and 100% in those cases not using a secondary immunosuppressor, p = 0,015 vs. the combined CyA+Aza and CyA+MMF group (Table 1). There were no differences in the degree of CyA exposure among subgroups using CyA + Aza, CyA + MMF and CyA alone, whether measured by mg/kg/day dosage, with CyA + Aza 3.5 ± 1.6, CyA + MMF 3.4 ± 1.9 and CyA alone 3.3 ± 1.1, p > 0.50, ANOVA, or by C12 CyA blood levels with CyA + Aza 175 ± 52, CyA + MMF 174 ± 52, and CyA alone 156 ± 53 ng/ml, p >0,50, ANOVA. Concerning the effect of other drugs associated with gingival overgrowth, 95 cases used verapamil and 17, nifedipine; out of those groups, 76 and 13 patients, respectively, belonged to the CyA group. GO prevalence was 56% for cases <45, and 26.3% for those > 45 years old (p = 0.001). For groups with good, fair or poor oral hygiene, GO prevalence was 30.3, 60.7 and 70.6% (p<0.001). In the multiple logistic regression analysis (table 2), GO prevalence increased with CyA use, (p <0.0001), age <45 years (p <0.001), and poor oral hygiene (p <0.016), and decreased with MMF (p = 0.007) and Aza (p = 0.020) use. GO association with verapamil and nifedipine use was not statistically significant. No association was found between GO and glomerular filtration rate or the diagnosis of diabetes mellitus. We were not able to analyze oral steroids effect on GO, because all cases used prednisone
DISCUSSION
GO in KT patients is a multifactorial condition. It is triggered by gingival inflammation from mixed etiologies: bacterial dental plaque, chemical irritation by CyA secreted with saliva at crevicular sulcus, and high CyA blood levels.9,10 Both situations generate aninflammatory response with mononuclear cell (mainly lymphocyte) infiltration, fibroblast proliferation, and extracellular matrix deposition.5,10 In this study, a repeat observation has been made of a higher GO prevalence in CyA ¿ treated patients: 59.1%, vs. 12.0% and 16.7% for patients treated with Tac and Siro respectively.11,7 The comparative effect with Tac has been previously known11,12 In 2008, Cota et al. found a 20.8% GO prevalence in Sirolimus ¿ treated KT patients7 The striking 100% GO prevalence in the eight CyA-alone (plus prednisone) cases, as compared to 60.2% and 47.2% figures for CyA+Aza and CyA+MMF cases (table 1), a difference not accounted for by disparities in CsA dose or blood levels, suggest unhindered CyA gum toxicity. Other authors recognized a sparing effect of Aza on CyA- or Tac- associated GO prevalence and severity, and point to gingival inflammation as a risk factor for developing GO.4,9,11 Azathioprine¿s protective effect against the risk of GO has been explained by its antiproliferativa and anti-inflammatory action, but it has also been recognized as having a proapoptotic effect on T cells.15 As far as we know, MMF has not previously been shown to have a protective effect against GO. Our finding for this drug is that of a sparing effect, quantitatively similar to that offered by Aza (tables 1 and 2). Some of MMF known actions include inhibiting T and B lymphocyte proliferation, suppressing cell immunity and antibody production, T-cell apoptosis, antagonising IL-1 actions, inhibiting lymphocyte and monocyte recruitment to the inflammation area,16 inhibiting over-expression of the profibrotic agent TGF-b,17 indirectly decreasing local tissue damage caused by macrophages, and reducing the proliferation of arterial smooth muscle.16 The gradual discovery of these actions has led to the use of MMF for nontransplant conditions, and it has been shown to provide protection against tissue damage from autoinmune, toxic, or reduced renal mass causes, sharing inflammation as tissue damaging mechanism 18,19 Some of these actions could explain MMF¿s protective effect against the development of GO in this patient group. The review of CyA ¿ associated GO pathology and pathophysiology, and the sparing effect of Aza and MMF, prompts a consideration about parallel pathogenesis in chronic allograft nephropathy, raising the hypothesis that CyA¿s known allograft nephrotoxicity does usually coexist with an as yet not clearly recognized opposing or buffering action by the secondary immunosuppressor drug, hinted at by the 100% GO prevalence in Cya-alone cases. We weren¿t able to find an association between GO prevalence and severity, on the one hand, and kidney allograft function level, on the other, as other authors did20, possibly because of a rather short mean time from KT surgery in our group, or perhaps because we weren¿t able to search for an association to earlier markers of allograft nephropathy, instead of the late markers of a rising serum creatinine or a dropping GFR.
GO prevalence is higher amoung young people.9,10 We found indeed a 5.6 GO odds ratio in cases <45, as compared with patients >45 years old. As for poor oral hygiene, the OR was 3.2 as compared to good hygiene. Previous studies explained these findings based on younger patients rising a stronger inflammatory response to poor oral hygiene, and to hormonal differences.9,10 The 12% GO prevalence found in the Tac group agree with findings from other studies;5,6 the observed severity was also low. GO Risk factors from these studies were previous use of CyA, use of Calcium channel blocker anti-hypertensives,5 inflammation and gingival/papillary bleeding, and bacterial plaque deposits.12,21 The association between using Tac and GO has been called into question. Some authors have reported partial or total resolution after substituting Tac for CyA.22 Nassar et al.23 concluded that Tac produces a less severe form of GE, and the risk factor was the length of exposure to the drug. In our cases treated with Tac, GO prevalence was low and gum disease less severe. We didn¿t find GO associated to calcium channel blocker antihypertensive drugs.
CONCLUSIONS
MMF and Aza had a GO-sparing effect in this group of patients.There will be a need to further explain the protecting mechanisms and to find out if these drugs do really grant a similar protective action on CyA nephrotoxicity in KT patients.
Table 1. Prevalence and severity of gingival overgrowth in groups using Cyclosporin A, Tacrolimus, or neither one
Table 2. Multiple regression analysis, risk factors for gingival overgrowth