Dear Editor,
Syndrome of inappropriate antidiuretic hormone hypersecretion (SIADH) should be suspected in patients with hypoosmolar hyponatraemia, elevated urinary osmolality, sodium concentration in urine above 40mEq/l, normal acid-base balance and blood potassium, and a low concentration of uric acid in plasma. Extracellular volume should be normal and the presence of kidney failure, hypothyroidism, cortisol deficiency and diuretic treatment should be ruled out.1
Among the causes of SIADH, those that are secondary to lung diseases have been described.2-4 Possible mechanisms of induced vasopressin secretion are: hypoxaemia and hypercapnia, haemodynamic abnormalities, alterations in the regulation and release of desmopressin caused by tumours, different drugs and stress.4
We would like to describe the case of a 68-year-old male patient who was taken to the Emergency Department because of diffuse abdominal pain and vomiting, as well as alarming symptoms that included slow mental reactions and disorientation. The patient had a history of chronic obstructive pulmonary disease caused by severe asthma treated chronically with oral corticosteroids, non-insulin-dependent diabetes mellitus, arterial hypertension and a transurethral resection of the bladder because of a neoplasia four years before. The patient¿s usual treatment consisted of metformin, simvastatin, enalapril, alendronic acid, calcium carbonate, omeprazol, methylprednisone and inhaled bronchodilators.
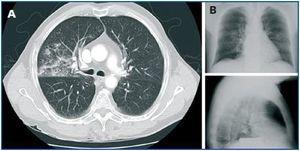
A blood test was carried out which revealed severe hyponatraemia 115mmol/l with plasma hypoosmolality 243mOsm/kg and hypouricaemia 2.4mg/dl, with normal blood potassium and renal function. There was elevated sodium loss in urine of 148mEq/l. The presence of hypothyroidism and adrenal failure was ruled out. The patient appeared to present SIADH and so water was restricted and hypertonic intravenous saline solution was administered. The patient¿s hyponatraemia progressively improved and his cognitive state normalised. When searching for the cause of SIADH, a brain MRI scan was carried out but no significant findings were made and a chest CT was performed which showed increased density of alveolar characteristics limited to basal segments of the right upper lobe that was very suggestive of pneumonia (figure 1A). However, a chest x-ray had been carried out on admission that did not show significant changes with regard to previous tests (figure 1B), the respiratory auscultation was normal and there were no leukocytes or other values that indicated infection. During admission the only significant symptom was an occasional fever of 37.2-37.4º C. Therefore, oral levofloxacin treatment was started and six days later a new chest CT showed significant improvement in the pneumonia. The urinary antigen tests for Legionella and Pneumococcus were negative. Gradually, the withdrawal of hypertonic saline solution was possible. It was administered until discharge following 15 days in hospital with water restriction, 6g per day of salt and 10mg/day torsemide. Plasma sodium levels remained stable at 131mmol/l. In the GP follow up, salt and diuretics were withdrawn and a month after admission the patient had fully recovered from SIADH, with plasma sodium levels 136mmol/l.
The following lung diseases have been described in the literature as potential inducers of SIADH: pneumonias, (viral, bacterial, tuberculous, mycotic), pumonary abscesses, asthma, atelectasis, pneumothorax and fibrocystic disease.2-4 With regard to pulmonary tumours, small cell carcinomas are most likely to be involved, since induced SIADH is a paraneoplastic condition due to the ectopic secretion of vasopressin.4 In the cases described, the symptoms of pulmonary diseases stand out first and foremost. In the case of our patient, it is interesting that the aetiological study of SIADH led to the diagnosis of pneumonia after the chest CT was carried out. Therefore we would like to highlight the importance of examining the lungs in cases of SIADH, especially when dealing with immunodepressed patients who are generally treated with corticosteroids and whose symptoms of infection may be latent, and thereby associated with very low clinical suspicion.
Figure 1.