Until 1970, Spanish patients with advanced chronic kidney disease died inexorably. Since then, our health system has undergone immense development in renal replacement therapy programmes using dialysis and transplants, and currently, these patients can fortunately be treated with high levels of quality.
The progressive increase in the number of patients requiring this type of treatment, as well as the costs it entails, has been the object of several different publications and many special issues in our Nefrología journal. In 1994, we put together a Nefrología supplement based on the conference on economic and organisational aspects of the treatment of chronic renal failure, which took place at the summer Menéndez-Pelayo University in Santander.1 Recently, another special supplement was published regarding the sustainability of renal replacement therapy that has served as information for reflection on several of the socioeconomic aspects of this type of treatment.2
Finding ourselves in the midst of an economic crisis, and looking towards the future, what can we nephrologists do in order to ensure the continuity and equity of renal replacement therapy in Spain? This is the issue that we will debate here.
THE SUSTAINABILITY OF THE SPANISH HEALTH SYSTEM IS AT RISK
The life expectancy at birth from 2006 placed Spain as the highest country in the 15 member countries of the European Union, and this came at the lowest health costs as well. With a mean 81.1 years life expectancy, Spain is at the forefront of countries such as France, Italy, Sweden, Austria, etc., and the health costs (public + private) are only 8.4% of the gross domestic product (GDP), whereas the mean for the 15 countries of the EU is 9.2%, with extreme values in Luxembourg (7.3%) and France (11.1%) (Sources: Organisation for Economic Cooperation and Development [OECD], the World Health Organisation [WHO], and Instituto Nacional de Estadística (National Institute of Statistics) [INE]). However, this value rose to 9% for Spain in 2008.
In the coming 10 years, one in five Spanish citizens will be older than 65 years, and per person health costs will range between 4 and 12 times greater than for those younger than this age. The mean annual cost per capita for the year 2025 is estimated at €2192 for people younger than 65, €8570 for those between the ages of 65 and 79, €14 996 for those between the ages of 80 and 94, and €28 479 for those older than 95 years (sources: INE [2009], Statistical Office of the European Communities [EUROSTAT], OECD, and WHO). Given the current growth rate, health costs could double in the next 10 years. In other words, in 2020, 50 of every €100 in public spending in the Spanish Autonomous Communities could be destined to health care, as opposed to the current amount of €35.3
One of the components in this health cost is renal replacement therapy. Although these patients make up only 0.1% of the population, they consume 2.5% of the National Health Service (NHS) budget, i.e., in spite of being a small proportion of the total population, they consume a significant amount of resources. This is the problem that must be resolved, or at least given an in-depth analysis, by health authorities and with the help of nephrologists.
RENAL REPLACEMENT THERAPY IN SPAIN
According to the most recent dialysis and transplant report from 2009, from the Spanish registry of renal patients, developed by the Spanish Society of Nephrology (S.E.N.) and the Spanish National Transplant Organisation,4 the number of new patients has stabilised since 1999, with an incidence of 129 new patients per million population (pmp) in the year 2009, as opposed to 126 pmp 10 years earlier. In this group, 85.1% of new patients are treated using haemodialysis, 12.1% using peritoneal dialysis, and 2.8% using renal replacement therapy and a kidney transplant before initiating dialysis.
This stabilisation in the incidence of the disease has not been mirrored in the prevalence. In 2001, 885 patients pmp were treated using renal replacement therapy, and this value increased to 1039 patients in 2009. Of the patients receiving treatment, 47.67% are on haemodialysis, 47.51% undergo kidney transplants, and 4.82% are on peritoneal dialysis.
As we commented on earlier, the general population being treated with dialysis and transplants is aging. In the report from 2009, the incidence was 169 (45-64 years), 390 (65-74 years), and 464 (>75 years) pmp.
For example, when comparing the years of 2008 and 2009, we observe a 4% increase in the number of patients on peritoneal dialysis, a 3% increase in the number of patients on haemodialysis, and a 2% increase in the number of patients living with a functioning kidney transplant.
DIALYSIS TREATMENT IN SPAIN
Using public financing, an offer currently exists for both public and private sectors to administer replacement therapy for chronic kidney failure in Spain. According to Largo, who was the assistant director for contracting health services in the Spanish Ministry of Health and Consumer Affairs, it is a sector in which the public-private collaboration within the NHS has contributed efficiently to the resolution of a serious health problem.5 In Spain in 2009, there were 363 dialysis centres, attending 21 297 patients on haemodialysis (453 pmp). In 2007, 45% of dialysis centres were owned by companies such as Fresenius, FME, Braun, Diaverum, Baxter, etc. Fifteen percent were managed by private centres, and 40% were located in public facilities. Between 2005 and 2009, the number of dialysis centres managed by companies increased by 3%, the number of private centres decreased by 3%, and the number of public centres increased by 19%.
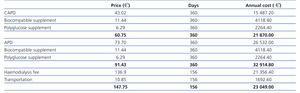
The costs for dialysis in Spain during 2010 can be observed in Table 1 (source: Industry). These prices only include treatment during the dialysis session, and do not include medications, which must be considered separately. As we can see, the cost of basic peritoneal dialysis is the lowest, although the use of biocompatible supplements, polyglucose, and automation of the process all raise the price even above that of haemodialysis. In 2010, 53% (1237 patients) were on automated peritoneal dialysis, and 47% (1090 patients) on continuous ambulatory peritoneal dialysis (CAPD).
With this in mind, the presentation of peritoneal dialysis as an option must be based primarily on aspects of quality rather than costs, such as the excellent techniques for starting treatment, the preservation of residual kidney function, patient independence, nutritional freedom, reduced need for medication, etc.
Even though renal replacement therapy implies costs during the first year that are similar to those of dialysis treatment (including all medical costs), it is the best cost-effective technique, since the cost in subsequent years is only 20% of this amount.
HOW CAN THE DECISIONS OF THE NEPHROLOGIST IMPACT THIS INCREASE IN HEALTH COSTS THAT PLACES THE FUTURE OF RENAL REPLACEMENT THERAPY IN DANGER?
We can list several different possibilities:
1. Increase the rate of kidney transplants;
2. Increase the percentage of patients on peritoneal dialysis;
3. An honest reflection regarding the costs and benefits of prescribing medications;
4. Integrated management contract;
5. Consider the use of non-universal dialysis.
Increasing the rate of kidney transplants
The actions taken by the Spanish National Transplant Organisation, consolidating the concepts already put into place by the Spanish Society of Nephrology in the development of coordinated kidney transplant programmes, has elevated our country to become the leader in cadaveric kidney transplantation. Currently, based on the transplant and dialysis report from 2009,4 47% of the patients living with renal replacement therapy do so through kidney transplants.
The use of cadaveric kidneys probably will not surpass the current rates. In 2009, 2328 cadaveric kidneys were transplanted, with 2225 in 2010. It would be difficult to augment this level, although some programmes do exist that could facilitate an increase to some degree, such as implementing kidney transplants from non-heart beating donors, which has produced very positive results in some Spanish health centres.6
Another possibility for increasing the number of kidney transplants is to promote living-donor transplantations, which are currently on the rise in Spain, although only modestly. In 2001, 26 kidneys were transplanted from living donors, whereas this amount rose to 148 in 2009.4 The majority of health centres have developed a sufficiently consolidated protocol for us to hope for a significant increase in these numbers, as well as new programmes such as the cross-over kidney transplantation. However, we must keep in mind that only 20% of patients receiving dialysis treatment are also included in waiting lists for kidney transplants, and so global implementation of this type of treatment is impossible.
Increasing the percentage of patients on peritoneal dialysis
After kidney transplantation, (non-automated) peritoneal dialysis is the most economically viable option for renal replacement therapy after the first year. In spite of this, only 4.8% of patients were receiving this type of treatment in 2009. Some Autonomous Communities have reached rates as high as 25%, but in spite of blatant promotion of this technique (in our nephrology department, all patients that are to be treated with dialysis start out with a consultation for peritoneal dialysis), we have not been able to increase the overall number. The primary reasons for this failure are that this technique becomes considerably less effective after 2 years, it is given up by tired patients, is interrupted for kidney transplantation and, primarily, the lack of patient dedication to this technique. We must also add to this list the lack of enthusiasm presented by some physicians for this technique, which could increase significantly until all of Spain reaches mean values such as those from Galicia, Cantabria, and Basque Country.
Drug prescriptions
The concept of cost-effectiveness is still far from being universally adopted by the medical community, and especially so by nephrologists. The problem we deal with is not based on whether or not a drug should be financed, or the financing of drugs that have demonstrated costs and benefits, but rather the financing of drugs that have not demonstrated them.7 A very clear example is that of phosphate binders.8 The decision made by a nephrologist can imply a cost that varies between €61 (calcium carbonate), €219 (calcium acetate), €410 (calcium acetate and magnesium carbonate), €2178 (lanthanum carbonate), and €2512 (Sevelamer). Along with other authors,9 we have defended the stance that agents based on calcium compounds should be the first choice in binders used for dialysis patients, since these are the cheapest and best tolerated compounds in the treatment of hyperphosphataemia, with similar results to other binders. Sevelamer and lanthanum carbonate have not been shown to be superior to calcium-based products. They are much more expensive and are also associated with more side effects. In the absence of a clear clinical benefit proven by these compounds, they should not be recommended as an initial therapy. The calcium issue can be easily resolved using calcium acetate with or without magnesium carbonate (this reduces the quantity of calcium with proven efficacy).10 In 2008, we spent many millions of Euros in Spain on non-calcium binders in order to control hyperphosphataemia, even when other cheaper and more effective options were available. A recent Cochrane review on phosphate binders also concluded that the most expensive compounds were no better than the cheapest ones.11
This is simply one example, and we could also discuss other concepts such as erythropoietic products, vitamin D compounds, etc. The point is that there are many ways to reduce costs. In a study from 2009 with dialysis patients, the greatest economic burden was erythropoietin (€22.6 per patient per day), approximately 68% of total drug costs.12 A more recent estimate from the region of Murcia13 showed that, from a total cost of €197 per patient per week, 34% went towards phosphate binders, 25% was for erythropoietin, 16% for calcimimetics, 3% for iron, 5% for vitamin D, and 16% for other drugs. These values have changed somewhat since then, with an increase in calcimimetics and a decrease in erythropoietin, and there is room for the nephrologist to manoeuvre, adjusting and controlling the costs derived from prescribed medications.
Integrated management
This is a new process with as yet undemonstrated results, but that initially appears to positively influence the costs of renal replacement therapy. The Health Department of the region of Murcia is developing this methodology, which requires tight cooperation between the company in charge of managing dialysis care and the nephrology department from the reference hospital.
An integrated management contract would mean state-subsidised treatment with regard to:
1. Dialysis treatment of any kind (haemodialysis, on-line haemodiafiltration, peritoneal dialysis, daily haemodialysis),
2. Medications (intra- and extra-dialysis),
3. Laboratory analyses,
4. Other diagnostics and tests,
5. Vascular and peritoneal access,
6. Patient transportation.
As we have seen, all types of dialysis are included in this type of integrated contract, which allows the nephrology department in the reference hospital to treat the patient being limited only by the clinical characteristics and condition of the patient, and keeping in mind the objectives set forth regarding quality.
Among the benefits provided is the indication of the type of treatment, a greater ease of administering home treatment when indicated, which includes better clinical results and lower overall costs, and an agreement that efficiency is not attained at the cost of lower quality of treatment.
DIALYSIS FOR END-STAGE PATIENTS
When dialysis programmes were started, the objective was to facilitate the return of relatively healthy patients to work and society. The reality is that many patients older than 75 years with advanced renal failure have three or more comorbidities and very low life expectancy. The ethical issues must be approached with courage and honesty: should dialysis be for everyone?
Currently, developed countries have no limitations in the application of renal replacement therapy. This situation frequently implies that the suitability of treatment for each particular patient may not be adequately evaluated, although it is evident that not all patients can receive the same benefits from this treatment. Some studies have retrospectively analysed the survival of patients older than 75 years with stage 5 chronic kidney disease in specialised clinics for this pathology, finding that the advantages provided by dialysis are substantially reduced by comorbidities in these patients, and by ischaemic heart disease in particular.14 The study performed by Couchoud et al15 was a truly practical assessment of this subject, and using a simple grading system for comorbidity, they were able to predict the short-term prognosis of patients older than 75 years starting dialysis. In many of these cases, conservative treatment produces equal survival and a better quality of life for the patient and his/her family. This is not simply a question of making renal replacement therapy sustainable, but there is also an ethical issue in protecting a severely incapacitated sick person and the patient’s family from prolonged agony. End-stage dialysis should be reconsidered against medical treatment without dialysis.
SUSTAINABILITY OF THE SPANISH NATIONAL HEALTH SYSTEM
All the measures that nephrologists may take to control the costs derived from renal replacement therapy will be very ineffective if not accompanied by a restructuring of our current NHS model. This restructuring cannot logically be discussed in this brief editorial, but the Spanish society, and we especially, the professionals working in the health sector, must express ourselves clearly regarding the current state of affairs. We will comment on just a few of these aspects.
Co-payment
Current data indicate that the rate of patients seeking medical attention in Spain is 40% greater than the mean for the 15 European Union countries.3 The logical consequences are a saturation of health services and an increase in expenditure.
The Comisión de Análisis y Evaluación del Sistema Nacional de Salud (analysis and evaluation committee of the NHS) (Abril’s Committee) from 1991 produced an excellent report elaborated by all sectors of Spanish society.16 This report informed that we must adopt measures that limit the over-prescription of drugs. Acknowledging that these measures would be unpopular, participation in assuming these costs and compensation in other sectors such as pensions and fiscal reimbursements was recommended. The rule of thumb would be participation in assuming costs, except for certain groups when deemed necessary. If, for political reasons, it were not convenient to globally implement cost participation, expenditure could be analised and later reimbursements of 40% could ensue.
The majority of European countries use health care co-payment and drug payment plans (Germany, Belgium, France, Italy, Portugal, and Sweden), although with one exception (United Kingdom). This idea has always been rejected in Spain with arguments of social protection and elevated management costs. In our opinion, it would be unlikely that a political group would assume this idea due to the impact it would have on elections, but we must abandon the idea of “political opportunity,” and instead adopt a concept of “social opportunity.”
Government health agreement
Professor Segovia de Arana, one of the main actors in developing the current excellence provided by the Spanish health system (founder of the internal medicine residency programme), has worked along with other very important representatives of Spanish medicine in the European Academy of Sciences and Arts to edit a Libro Blanco sobre el Sistema Nacional de Salud (white paper on the Spanish health system). They predict that if the political parties in Spain do not come to an agreement, the Spanish health system as we know it will be drowned in the sustainability issues that plague it.
On September 30th 2010, President of the House of Commons’ health committee Gaspar Llamazares concluded that two years of work had been a failure in the attempt to reach a government agreement in order to safeguard the viability of the NHS.
Governmental restructuring
The debt for health products and medications on 31 December 2010 was 8.739 billion Euros, of which the Communities of Andalusia, Valencia, and Castile and Leon made up more than 35%. Many health care providers have to wait up to 600 days to receive payment, with the greatest delays produced in the Communities of Cantabria (709 days), Baleares (645 days), and Murcia (612 days).17 Although some of these areas already have a disbursement centre within their territory, it is surprising the frivolousness with which the concept of economies of scale is ignored. Very wide ranges of prices are charged for the same product, causing a rupture in the equity of the system.
The existence of different vaccine calendars among Autonomous Communities is a clear expression of the idiocy that permeates our health system. There are also different models for financing certain drugs for particular patient groups. For example, in Castile and Leon, a decreased amount is paid for antifungal and antiviral medications in cancer patients; in Extremadura, the overall cost of drugs is financed when prescribed to large families and patients with chronic diseases that are younger than 14 years of age, and in Valencia, the full cost of treatment for tuberculosis is financed.18
It would be logical to restructure the system in such a way that would concentrate resources, make purchases cheaper, pay for services on time, and ensure equity in the health services provided to any Spanish citizen. Currently, the financing of our health system shows major differences between the Autonomous Communities, with a €560 difference between the territory with the highest per capita budget (Basque Country) and the lowest (Baleares).18
Structural changes that involve the concept of concentration, such as attempts at synergy, shared diagnostic platforms (both imaging and laboratory), restructuring of diagnostic and therapeutic indications, and improved management (human resources, information, equipment, etc.) could be implemented in order to save costs.18
In our opinion, a restructuring of the NHS along with a Government Agreement is necessary for ensuring sustainability.
Need for leadership
Our NHS has a general lack of leadership, and this is mirrored in all of the institutions that compose it. Nor does it have a governmental entity that must be answered to and that requires proper use of public resources, whether centralised or autonomic. For this, we must have a government that ensures the sustainability of our health system, and therefore, of renal replacement therapy. This government would have to exert political, economic, and knowledgeable authority for the management of national affairs.
Conclusion
Although the nephrology service provided in Spain is cost-effective and of very high quality, some measures which have been discussed here could be incorporated by nephrologists into our daily practice in order to ensure the sustainability of renal replacement therapy. However, our compliance with our responsibilities as vectors for health costs will be for nothing if it is not accompanied by changes in our NHS. Several of these necessary changes will not come about simply due to the electoral interests of politicians. Perhaps the first step we must take is to demand a global accord to ensure the sustainability of our NHS, both in its social (equity) and economic aspects.
Table 1. Mean dialysis costs in 2010 in Spain (¿)