Antecedentes: A finales del siglo pasado, evidencias científicas de nivel II apoyaban una mayor supervivencia en técnicas de hemodiálisis (HD) alternativas a la HD convencional, cuya expectativa de vida a cinco años, en Europa, era inferior al 40 %. Desde el año 2000 nuestros pacientes incidentes se adscribieron a una estrategia de HD no convencional con el objetivo de evaluar su influencia en la supervivencia. Método: Estudio de cohorte realizado en 183 incidentes en HD entre 2000 y 2010. Al inicio de la HD se evaluaron antecedentes de enfermedad cardiovascular (EFCV) e índice de Charlson (ICh). Desde el año 2000 iniciamos la estrategia de HD no convencional que contenía protocolos de HD biocompatible, de alto flujo, objetivo de peso seco, esquema de tres sesiones semanales de cinco horas (HD 5 h x 3) y desde 2003, coexistiendo con el anterior, se inicia el esquema de sesiones de HD de cuatro horas en días alternos sin descanso de fin de semana (every other day dialysis: EODD) para incidentes de mayor riesgo. Resultados: De los 183 pacientes incidentes en el programa de HD, 84 se dializaron en esquema HD 5 h x 3 y 99 en EODD. La edad media fue de 60,6 ± 13,8 años, el 31,7 % eran mayores de 70 años, diabéticos el 43 %, con EFCV el 58,5 % y el ICh medio era de 4,55. La supervivencia (%) del primero al quinto año fue de 92, 82, 75, 62 y 55, con mediana de 5,65 años (intervalo de confianza [IC] 4,18-7,11) y media de 5,4 (IC 4,75-6,1). Conclusiones: La estrategia de HD no convencional que aplicamos a los pacientes incidentes en la técnica proporciona un buen resultado de supervivencia.
Background: At the end of the last century, level II scientific evidence supported higher survival rates for alternative haemodialysis (HD) techniques when compared with conventional HD, whose five-year life expectancy in Europe was below 40%. Our incident patients participated in an unconventional HD strategy from the year 2000, with the aim of assessing its influence on survival. Method: A cohort study on 183 incident HD patients between 2000 and 2010. At the beginning of HD, we evaluated a history of cardiovascular disease (CVD) and Charlson index (ChI). In the year 2000, we began the unconventional HD strategy that included protocols of biocompatible high flux HD, dry weight target, a schedule of three weekly five hour sessions (HD 5h x 3) and from 2003, in combination with the foregoing, we began a schedule of four hour HD sessions on alternate days including weekends (every other day dialysis: EODD) for higher risk incident patients. Results: Of the 183 incident patients in the HD programme, 84 were dialysed in the 5hx3 HD schedule and 99 in EODD. The mean age was 60.6±13.8 years, 31.7% were older than 70, 43% were diabetic, with CVD sufferers at 58.5% and the mean ChI was 4.55. Survival (%) from the first to the fifth year was 92, 82, 75, 62 and 55, with a median of 5.65 years (confidence interval [CI] 4.18-7.11) and a mean of 5.4 (CI 4.75-6.1). Conclusions: The unconventional HD strategy that we applied to incident patients in the technique resulted in good survival.
INTRODUCTION
Since the end of the 20th century, we have witnessed the universalisation of haemodialysis (HD) treatment for an older population with a higher incidence of diabetes (DM) and with increased cardiovascular comorbidity, which are the factors directly related to mortality in HD. Since the inception of the technique, studies1-6 have been published that reported improvements in survival in relation to some of its components, but they did not achieve the maximum range of scientific evidence. However, in the West, we maintain conventional low flux HD schedules with three weekly sessions of four hours, with seventy-two hours at the weekend without HD and without a reduction in mortality.7,8 In this conventional schedule, the recent DOPPS (Dialysis Outcomes and Practice Pattern Study) recorded a duration of HD sessions of four hours in less than 50% of patients and less than four hours in more than 50% for our country.9
Since the year 2000, our unit began an unconventional HD strategy which incorporated a set of actions in HD treatment consisting of biocompatibility-related HD, use of a high-flux synthetic membrane dialyser, sessions with increased time or frequency in accordance with the patient's risk level and control of extracellular volume (ECV), while also incorporating new technologies.10 These protocols were based on previous studies with level II evidence that showed reduced mortality and whose implementation was within the scope of normal clinical practice.
The aim of the study was to evaluate the impact of this unconventional HD strategy on survival of patients who started treatment in our HD unit during the 2000-2010 decade.
PATIENTS AND METHOD
Population
A cohort study conducted in 183 patients with chronic renal failure, incident on HD from any cause between 2000 and 2010 in the HD unit of the Hospital Universitario de Puerto Real, with minimum time in the technique of one month, who accepted HD protocol described later. Of the remaining incident patients for that period, 61 did not complete the full month in the technique and 6 did not accept the unconventional HD schedule protocol.
At the beginning, we evaluated their records: cardiovascular disease (CVD), history of arrhythmia, heart failure or angina/myocardial infarction, cerebrovascular disease or peripheral vasculopathy; a Charlson comorbidity index (ChI) that was low if lower than 4, medium if between 4 and 6 and high if greater than 6. DM was considered as a previous diagnosis and risk in ChI, regardless of the cause of renal disease.
The mean age was 60.6±13.8 years; 57.4% were older than 60 and 31.7% were older than 70. Baseline characteristics are shown in Table 1: the patients are predominantly male (1.5:1 ratio), with initial presence of DM in 43% and CVD in 58.5%.
Unconventional haemodialysis schedule
Patients were treated in accordance with the following protocol:
1. HD schedules: in the year 2000, we began the schedule of three weekly sessions of five hours (HD 5h x 3) with a 72-hour break at the weekend.11 In 2003, and in combination with the previous schedule, we began a schedule of four-hour sessions on alternate days (EODD) every 48 hours4 (Monday-Wednesday-Friday-Sunday-Tuesday-Thursday-Saturday-Monday).
Criteria for the assignment of patients to the schedule:
5h x 3 HD schedule: 2000-2002: all incident patients during that period. 2003-2010: incident patients without CVD with low ChI or who did not accept the EODD schedule. If their body surface was less than 1.5m2 and they fully achieved their dose targets and ECV control, the time was changed to four and a half hours, provided that their dose and weight targets were maintained.
EODD schedule: 2003-2010: incident patients with CVD or medium-high ChI. HD patients who started HD on 5h x 3 HD (2000-2002) and who met any of the criteria for EODD, or who had gained weight >4% of dry weight12 after the weekend, which did not allow them to achieve their weight with an adequate ultrafiltration (UF) rate in HD 5h x 3. These patients were registered in EODD if they remained in this schedule for longer than six months.
2. Vascular Access: native arteriovenous fistula was prioritised as the first target; from 2004 we introduced the double-lumen tunnelled catheter temporarily whenever it was required for more than three weeks13 and, from 2009, prophylaxis protocol for catheter-related infections by filling with gentamicin and heparin of any type of catheter.14
3. High flux HD technique: Ultrapure water-based dialysate15 with flux of 500ml/min, bicarbonate buffer and constant sodium and UF profile. HD monitors with UF control. Sterilisation of the extracorporeal circuit and dialyser without ethylene oxide. Dialysers with synthetic membranes and UF rates >50ml/h/mmHg (polyamide, polyacrylonitrile or polysulfone) and areas of 1.7m2 and 2.1m2, indicated in accordance with the body surface. Blood flow >300ml/min. Convective techniques were not used.
4. ECV control: low salt diet (<4g/day). In each patient, at the start of HD, we aimed to achieve the dry weight target, by progressively withdrawing antihypertensive medication (AHTM)16,17 and linking with the UF rates necessary for reductions of 0.5kg to 1kg with respect to the previous weight, without exceeding, in general, losses above 3% of the weight at the beginning of HD.18
The target dry weight was evaluated after each haemodialysis session, during the time required for its stabilisation with AHTM withdrawal; once achieved, it was reassessed weekly in each patient.
5. The systolic blood pressure (SBP) targets were defined individually according to age and comorbidity.
The ideal profile was: initial SBP ≤180mmHg and end SBP ≥120mmHg19 with a pre and post HD mean blood pressure target not exceeding 150, and in general, the lowest SBP which is well tolerated during the session.20,21 From 2007, UF was limited to 10ml/kg weight/hour.22 From 2006, blood volume change23 was recorded on-line in each session by haemoglobinometry based upon optical absorption with the aim of reducing the time to less than 5%.24
6. HD dose. 2000-2005: Standard Kt/V ≥2. From 2006, Kt by ionic dialysance25 in each session, with on-line follow-up and minimum target according to the body surface,26 with a mean of 47 for HD 5h x 3 and 41 (47 x 13/15) for EODD.27 The session time was completed regardless of the anticipated achievement of the minimum target.
7. The programme contained the protocol for laboratory follow-up and anaemia control with intravenous alpha/beta erythropoietin and intravenous iron, calcium control, phosphorus, parathyroid hormone using phosphate binders, vitamin D analogues and, from 2007, cinacalcet.
All information was recorded on computer databases of the HD unit. Demographic variables such as sex, age at start of HD, history of CVD, ChI, duration of HD sessions, final state and cause of death, as well as session parameters and clinical and laboratory indicators were recorded. To analyse the unconventional HD strategy implementation results in our population, we applied the statistical method for measurements of central tendency and dispersion (means ± standard deviation) for quantitative variables and frequencies for qualitative variables. Statistical significance for P values <.05. For inferential statistics, we compared data by the Χ2 test and the Student’s t-test by types of variables and determined risks and confidence intervals (CI) at 95% and Kaplan-Meier survival curves and we used the log-rank test to compare curves.
RESULTS
Of the total of 183 patients, 84 were dialysed in HD schedule 5h x 3 and 99 in EODD schedule.
Table 1 shows the baseline data of the patients assigned to the two schedules. Age and comorbidity (DM, CVD, ChI) of patients on EODD were higher with significant differences with regard to patients on HD 5h x 3, in accordance with risk criteria for assigning patients to one or the other unconventional scheme.
Table 2 shows clinical and laboratory parameters for all patients. Only one patient required parathyroid surgery due to refractory adenoma; no patients had symptoms of carpal tunnel syndrome.
At the start of HD, 135 of the 183 patients were taking AHTM (74%), which was withdrawn in 126 (93%) during the follow-up period. In 8 patients, a stable dry weight was not achieved due to excess water and sodium intake, but the number of drugs was reduced and one patient had increased SBP not dependent on volume.
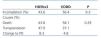
The main causes of discontinuation were death and renal transplantation (51.8% and 41.8%, respectively). The rest (6.4%) changed to peritoneal dialysis. Among the causes of death, the main cause was cardiovascular (42.9%), followed by infection (21.4%), cancer (17.9%) and other/not specified (17.9%). Table 3 shows the comparison of the causes of discontinuation in the two schemes. There were no significant differences. Cardiovascular mortality was similar in the two HD schemes.
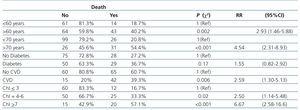
The overall survival curve of patients is displayed in Figure 1. It shows a median of 5.6 years (CI 4.18-7.11) and a mean of 5.4 (CI 4.75-6.1). This survival resulting from unconventional HD was independent of the schedule used (Figure 2), since both maintained this prognosis for the life of the patient (HD 5h x 3: median 6.16 years: CI 4.17-8.18, mean 6.03: CI 4.98-7.10. EODD: median 5.01 years: CI 2.9-7.12, mean 4.92: CI 4.18-5.67), although the baseline characteristics were different, as well as the assignment criteria for one or another schedule within the protocol.
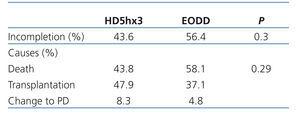
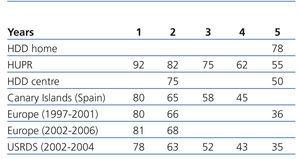
The analysis of risk factors for death (Table 4), using contingency tables, Χ2 and relative risks (with 95% CI) shows that the main risks for survival at the start of HD were: above mean age, being older than 70, having CVD and medium (CI = 4-6) or high (CI ≥7) ChI risk categories. The presence of DM at baseline did not reach significance (P=.17). The factors that were significant in the risk analysis were also significant in the inferential analysis carried out by comparing the survival curves (log-rank test): we highlight the comparison between the ChI categories at baseline (Figure 3).
DISCUSSION
The demographic and comorbidity characteristics of our population are similar to those recorded in our western setting,28-30 showing an increasingly older HD population, with a higher proportion of DM and more cardiovascular risk factors, all inversely related to survival in HD. Since the year 2000, we have applied an unconventional HD strategy to our incident patients by procedures supported by previous studies with a medium evidence level and we have incorporated innovative technologies, already referenced for the method, with the aim of improving the survival rates of our population.
Our study is consistent with most in terms of cardiovascular death being the most common cause and in terms of the main risks at the start of the technique: age above the mean, being older than 70, a history of CVD and medium or high ChI risk categories. Survival in both schedules did not show a significant difference in spite of the group on EODD having a significantly higher baseline risk.
We compared these results with those of recent studies in equivalent populations in terms of demography and risk factors (Table 5). In Spain, the study using Canary Islands Registry data for incident HD patients, in the period 2006-2009, shows that survival is 17% lower after four years28 with respect to our results. In comparison to the data (1997-2006) of the latest European Registry, the latter has results that are 19% lower at five years for the 1997-2001 period and 13% and 16% lower in the first two years for the 2001-2006 period.29 The data of the United States Registry for the period 2002-2004 also showed lower survival: 92% compared to 78% after one year, 82% compared to 63% after two years and 55% compared to 35% after five years.30 We also compared our results with those of short daily HD (unconventional HD with a mean of 13 hours per week). This study showed the survival of 415 patients from 1982 to 2005.31 In the 265 patients who followed this protocol at home, the five-year survival rate was 78%, an excellent result but one that resulted from a system that is difficult to access for the general HD population. Nevertheless, in relation to the 150 patients of the group with sessions in the centre, our survival result was marginally higher (55% against 50% after five years), in spite of our patients having worse risk indicators with a mean age ten years higher and with twice as many cases of DM.
Our results for survival are below those of other previous experiences of unconventional HD due, mainly, to the differences existing in the characteristics of the patient groups. More than twenty years ago, Tassin’s group1 reported the results of a strategy that combined an excellent control of ECV and dialysis dose, through a schedule of three weekly sessions of 8 hours with a cellulose dialyser and a strict follow-up of the dry weight control and SBP without the need for AHTM. The survival rate was 80% after five years and 75% after ten years. Nevertheless, the risk factors of patients who started the technique were very different from those of incident HD populations in the studies of the 21st century: mean age of 48 years, with other risk factors in only 20%. Other experiences of unconventional HD, such as long nightly HD sessions, yielded excellent results;3 however due to the selection of their populations, younger age, risk factors and less chance of general implementation, they are not comparable.
The EODD schedule employed in our medium/high risk patients is based on a study published in 1998 by Mastrangelo et al.4 (used as a variant of their other four weekly session schedule) in their patients with a body surface of less than 1.55 m2, although we did not adjust for body surface and maintained four hour sessions even if the minimum dose target was achieved. Lecce’s unconventional HD obtained an excellent five year survival rate of 75%, but for an incident HD population very different from the current population in terms of risk factors: mean age of 48 years, 22% over 60, 6% over 70 years and 37.5% at high risk. The EODD schedule was subsequently applied in the United States based on its good control of ECV.32
Our HD strategy involves protocols with higher biocompatibility systems, high flux HD, 25% increase in session times, dry weight target after withdrawing AHTM and an individualised SBP profile. Subsequently, from 2003, we implemented the alternative EODD schedule in medium and high-risk patients. The introduction of on-line biosensors allowed a change of method for assessing the dose and improving haemodynamic tolerance. We analysed the role that these protocols may represent in our results.
Increased frequency and duration of sessions. Control of extracellular volume and haemodialysis dose
The 1999 report of the significant increase of mortality in HD after the weekend33 was recently reiterated for all causes of death and particularly that of a cardiac nature34 in patients with a conventional HD schedule. The EODD schedule removes the “non-physiological” 72-hour35 period of ECV expansion, it allows adequate UF rates, control of SBP figures36 and improves session tolerance.37 The application of this protocol to our group of patients with CVD or medium-high ChI assigned to EODD may explain its survival results to a large degree, which confirms the negative influence of 72 hours without HD in patients with a high risk and CVD in conventional HD regimen. Although for the 5h x 3 HD schedule weekends were without HD for the lower risk group, the increase in time per session allowed dry weight to be maintained at the end of the week, and to be recovered at the start of the next week, ensuring ECV stability.
The 2006 DOPPS study recorded a 7% reduction in the relative risk (RR) of death for every 30 minutes that the session duration increased, a protective association between time and dose, and a higher risk of death when UF rates >10ml/hour/kg weight were employed.22 This requirement to adjust UF to the vascular filling capacity of the patient was confirmed for UF >12ml/hour/kg weight.38 The 2006 Australia and New Zealand Registry data corroborate the decrease in mortality for sessions of 4.5 to 5 hours.39 With respect to the conventional HD schedule, we increased the duration of sessions by 20% for 5h x 3 HD and 17% after one week in EODD with a dual effect on the clearance of molecules and the reduction of the UF rate. This made it easier to achieve the dry weight target with good haemodynamic tolerance: 93% of our patients achieved dry weight and discontinued AHTM; furthermore, they maintained a blood pressure profile that was adequate for the individual target and were not adjusted to the K/DOQI recommendations, whose SBP targets are questioned due to their inverse relationship with survival.40 The results of this study by Myers confirm the importance of this objective in maintaining adequate SBP figures in older patients on HD.41
Halfway through the decade, we changed the reference dialysis dose based on standard dialysis Kt/V, abandoning the urea distribution volume in favour of body surface Kt target with on-line follow-up.26 The mean Kt obtained per session (48.3) corresponded to that recommended for the mean body surface of our patients (1.73m2), but we never established a minimum dose for the end of the session. This change, in addition to benefiting patients of a smaller body surface, allowed on-line follow-up and analysis of the dose in each session, rather than once a month, with immediate corrections being available in order to improve it, with a very positive assessment being obtained in the control of its progression.
Biocompatibility and high flux haemodialysis
In the year 2000, all our patients began biocompatible HD with high flux membranes to clear Beta-2-microglobulin (β2-m), although, as has already been mentioned, it is difficult to establish the degree of improvement in morbidity or survival that can be attributed to each variable. In studies after 2000, they are related with higher survival rates with respect to conventional HD. In the initial report of the Hemo study,43 high flux HD improved only slightly, without statistical significance, mortality with respect to low flux HD, although secondary analyses showed a significant reduction in patients on HD for over 3.7 years and a significant reduction of mortality of cardiac cause;44 furthermore, it reflected the predictive value of the RR of death for β2-m levels, as well as the association of its lowest levels with high flux HD.45 Our patients had a pre-HD mean level of β2-m of 20.32mg/l, which was below the level of the high flux group of the study by Cheung et al. In the 2010 group of our prevalent patients according to the groups of risk of death by β2-m levels, 93% of them were in the group with the lowest risk level (<27.5mg/l); this could be explained because our population began and remained on high flux HD the whole period with high β2-m clearance and, furthermore with an increase in the time and frequency of sessions with respect to the conventional schedule of the Hemo study; the zero incidence of the carpal tunnel syndrome secondary to HD amyloidosis supported this argument in our patients during the decade of the study. Subsequently, the MPO (Membrane Permeability Outcome) study, conducted on incident patients,46 shows the positive correlation, with a high level of evidence, between survival and high flux HD, in patients with a level of serum albumin lower than 4g/dl and, in the secondary analysis, in DM. As a result, in 2010 the EDTA Guidelines modified the recommendation level for the indication of high flux HD, raising it to the highest degree in patients with albumin below 4g/dl and of grade B for DM,47 with its generalised use being recommended in patients for reasons of cost/efficiency.
In our patients, we have considered DM as a previous diagnosis and real risk factor in ChI, regardless of the cause of nephropathy. In contrast to many studies, the presence of DM as a factor of comorbidity at the beginning of HD, whether or not it was caused by nephropathy, did not reach significant difference with respect to the non-existence of DM as a risk factor for death. A possible explanation would be to attribute it to the positive effect and synergy that high flux HD contributes to DM associated with long periods on this technique and sessions of longer duration.
During the 2000-2010 period, various studies reinforced the initial level of evidence of each action in which our system was based, although our study has the limitation that, on being applied as a whole, it is difficult to attribute the degree of contribution of each measure to the survival result.
In conclusion, the unconventional HD systems we applied are a viable alternative for HD in the centre and, although they involve an additional cost, they generate significant savings on AHTM, hospitalisation and on the practical disappearance of urgent non-scheduled HD sessions generated due to over-hydration. Our HD strategy achieved good survival in our incident population and this result is possibly related to the joint and synergistic influence of the protocols applied within the unconventional HD strategy.
Acknowledgements
We would like to thank professor Evaristo Fernández Ruiz for his stimulation and support to innovation in dialysis since 1975.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Demographic and clinical data of the total number of incident patients and their group by haemodialysis schedule
Table 2. Clinical and laboratory data of the total number of patients during the period: mean ± standard deviation
Table 3. Causes of discontinuation and death by haemodialysis schedule
Table 4. Analysis of risk factors for death: number and percentage
Table 5. Overall survival (%)
Figure 1. Overall survival
Figure 2. Survival by haemodialysis schedule
Figure 3. Survival by Charlson index