Pregnancy is uncommon in women on dialysis, although an increase in the frequency has been seen in recent years. Owing to the higher maternal-foetal morbidity and mortality rates compared to healthy women, women on dialysis are advised to avoid pregnancy.1,2 However, multidisciplinary management and appropriate adaptation of dialysis therapy reduce complications and allow for a successful pregnancy. These measures include increasing dialysis time, maintaining low levels of urea pre-dialysis, and providing haemodynamic stability, avoiding intra-treatment hypotension and fluid-electrolyte fluctuations.1,2 With regard to the type of dialysis, the literature describes haemodialysis or peritoneal dialysis, but there is scant or no mention of the application of online high-volume haemodiafiltration (HVHDF).
We present the case of a patient who had HVHDF throughout her pregnancy, with the result being an uncomplicated, successful term pregnancy.
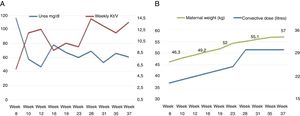
She was a 32-year-old woman with CKD secondary to lupus nephropathy and loss of the kidney graft due to rejection, restarted on haemodialysis in December 2017. She was receiving post-dilution HVHDF 3 times a week, 255 min per session, through a native arteriovenous fistula. Six months later, she had a positive pregnancy test after reporting 8 weeks of amenorrhoea. In view of the patient's complexity, a multidisciplinary group was established for her care and monitoring. Taking into account her uraemia levels, the number of weekly sessions was increased to 6 for 270 min each, maintaining the blood flow at 400 ml/min and dialysate at 500 ml/min. The Fresenius Medical Care 5008 machine was used, with a High Flux FX600 Helixone filter. In the dialysis bath, bicarbonate was reduced to 28 mEq/l, calcium 3 mEq/l, potassium 3.5 mEq/l, sodium 136 mEq/l and a temperature of 36 °C. Up to week 16, the post-dilution modality was continued with the use of total 5,000 IU heparin, which was changed to pre-dilution modality in order to restrict the use of heparin (2,500 IU total) due to metrorrhagia and placental haematoma. The convective dose was initially 20 l/session, increasing progressively to 24 l/session. At week 28, the obstetric ultrasound showed a maximum vertical pocket (MVP) of 8.8 cm, which was interpreted as polyhydramnios, owing to which we decided to increase the session time to 300 min and the replacement volume to 30 l/session, significantly reducing the MVP. The diffusive dose of dialysis was recorded with the determination of Kt/V by on-line clearance monitoring (OCM) in each session, achieving a Kt/week of 12. Mean arterial pressure was 120/75 mmHg controlled with labetalol 100 mg orally/24 h, without intradialytic hypotension (Fig. 1).
The patient had a successful pregnancy with no complications. There was no reactivation of her lupus disease. There were no relevant abnormalities in laboratory parameters, except for mild hypomagnesaemia, which was treated with oral supplements. The foetus showed successful intrauterine growth. A successful caesarean section was performed at 37 weeks, with the baby weighing 2.9 kg. Both were discharged home 72 h post-partum.
Although the benefits of post-dilution or pre-dilution HVHDF are known3 there are no reports in the literature on its application in pregnant patients, since, although some reports refer to haemodiafiltration, it involved low convective doses.1,4 It should be noted that the pre-dilution modality would provide the security of restricting the use of heparin, as was the case in our patient. Although the convective dose obtained per session in the pre-dilution HDF modality had an absolute value lower than that recommended in conventional patients with a three-week schedule, it is worth pointing out that, in our patient, the weekly number of sessions was doubled and, in addition, the convective dose corrected for body surface area5 and applying the dilution factor6 was 24 l. Although there is no recommended dose for on-line haemodiafiltration in the literature for pregnant patients, considering that the known treatment objectives were met (e.g. uraemia levels), we consider that the dose implemented was adequate.
We believe that, in our case, the HVHDF allowed us to optimise efficiency in the removal of medium molecules and the high clearance of small solutes, ensuring haemodynamic stability during the dialysis. Adaptation of the dose reduced the occurrence of polyhydramnios, attributable to the maintenance of low uraemia levels. At the same time, the safety of HVHDF was evidenced by the absence of complications during treatment and the maintenance of biochemical parameters such as vitamin B12 levels. We also saw no evidence of reactivation of lupus disease, unlike one report in the literature.4
It has been found that more frequent dialysis and over a longer time may be associated with greater fertility, as has been seen in patients with nocturnal haemodialysis.7 This has been attributed to a greater clearance of medium molecular weight uraemic toxins. It is worth considering whether HVHDF may enhance fertility, and whether this was the case with our patient.
In conclusion, we believe that when deciding on the appropriate dialytic technique for pregnant patients on dialysis, HVHDF may be the preferred indication. Reporting cases, as we have done with this patient, and the construction of suitable registry, will allow to confirm and established HVHDF as an additional recommendations for this vulnerable population of dialysis patients.
Please cite this article as: Crucelegui S, Luxardo R, Philipi R, et al. Embarazo exitoso en paciente con hemodiafiltración on-line de alto volumen pre-dilucional ¿La mejor opción dialítica en mujeres con enfermedad renal crónica y embarazo? Nefrologia. 2020;40:683–684.