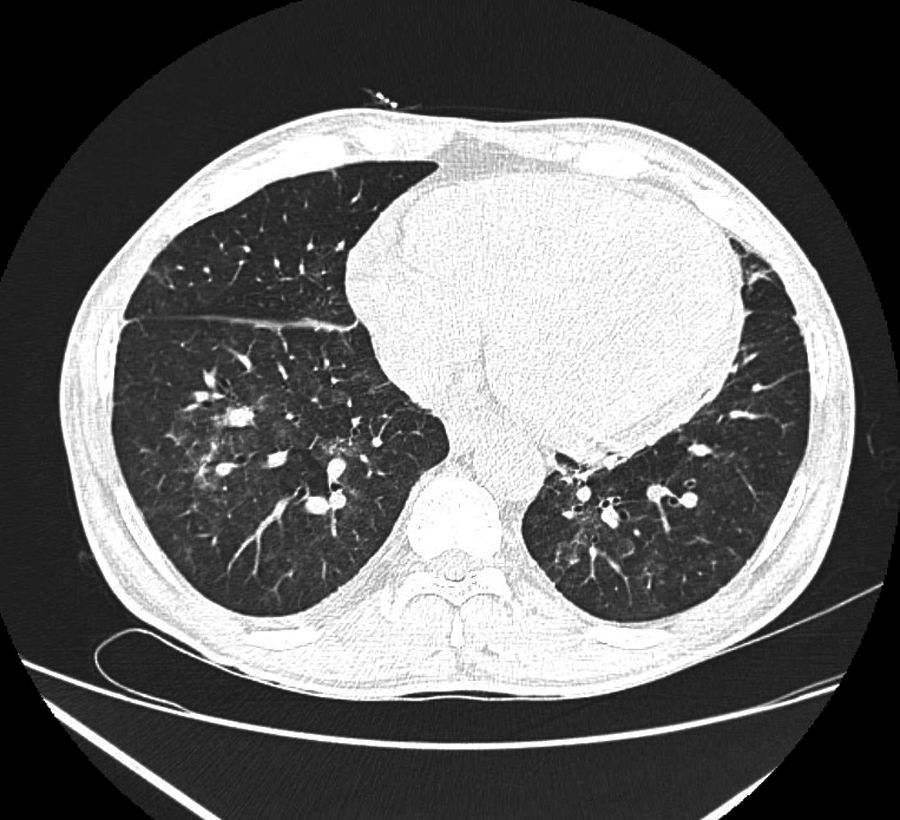
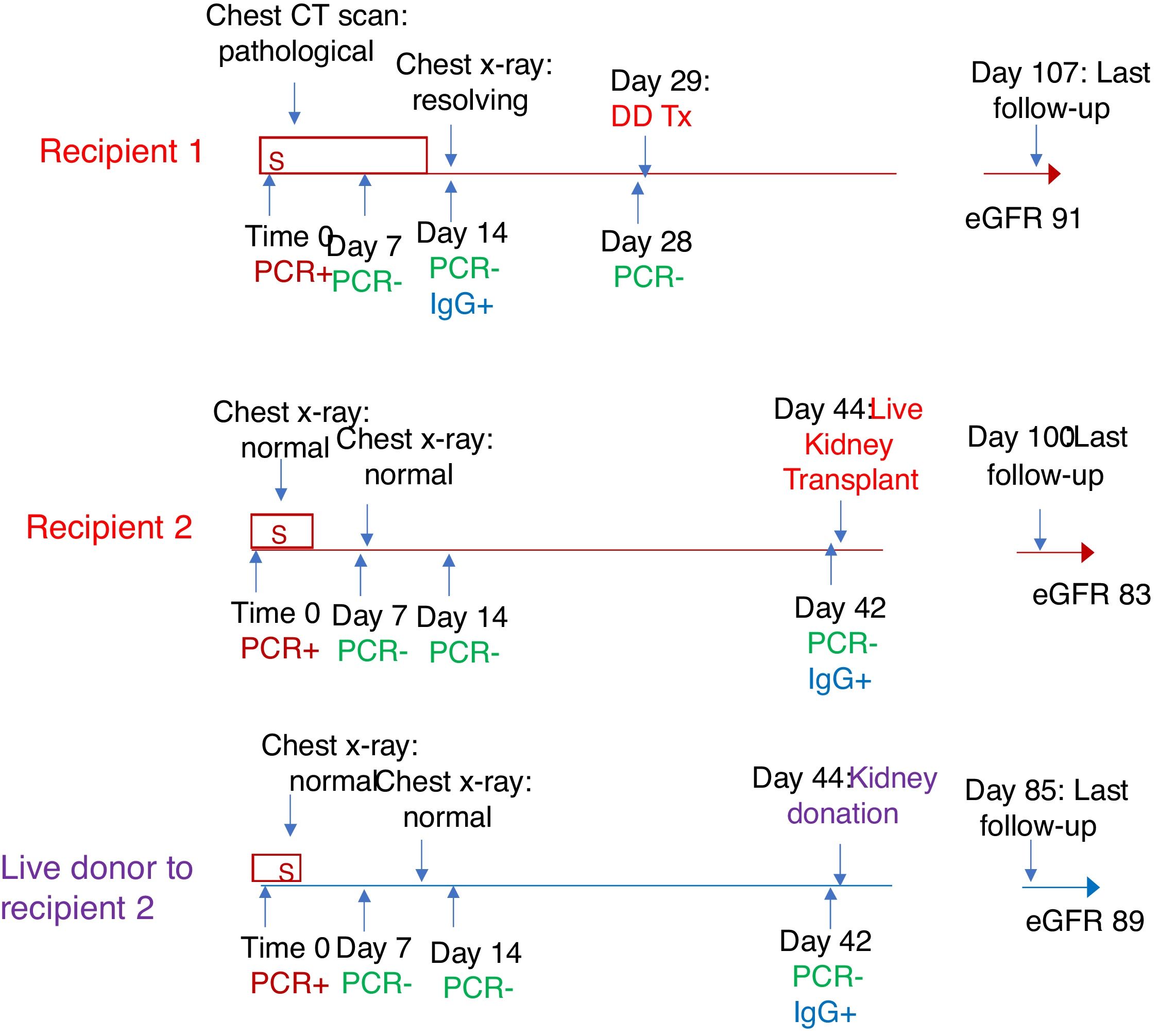
We hereby report two successful kidney transplants done during the pandemic of COVID-19. The first case was a 44-year-old male chronic kidney disease stage 5 secondary to diabetic nephropathy on haemodialysis, with left arteriovenous fistula as vascular access, who presented with myalgias for one day. There was no associated cough, sputum, fever or loss of smell. He was diagnosed to be positive for COVID-19 reverse transcriptase polymerase chain reaction (RT-PCR, cobas® SARS-CoV-2 test, Roche Diagnostics). Subsequently, he was diagnosed to have COVID-19 pneumonia (Fig. 1) and was treated for same with dexamethasone, oxygen support (oxygen saturations 87% at the time of oxygen initiation) and other symptomatic treatment. He improved clinically and was tested negative for COVID-19 PCR twice over next two weeks. Subsequently, serum IgG titres against SARS-CoV-2 (done at 2 weeks after the initial diagnosis) by chemiluminescence enzyme immunoassay (CLIA, CPC Diagnostics) were positive. A deceased donor kidney was offered and a calculated and explained risk was taken considering his recent recovery from COVID-19 pneumonia and the severe nature of his condition. The patient underwent a successful deceased donor kidney transplant after 4 weeks of initial diagnosis of COVID-19 with a negative pre-operative RT-PCR for SARS-CoV-2 and did not require any additional dialysis post-transplant. Basiliximab induction with triple drug immunosuppression consisting of prednisone, tacrolimus and mycophenolate mofetil was used. His post-operative period was uneventful and was discharged with a good graft function. He remains well at last updated follow-up of 15 weeks (at the time of writing this report) post-transplant with an eGFR of 91ml/min/1.73m2 (Fig. 2). His current daily immunosuppression included prednisolone 10mg, mycophenolate mofetil 1500mg and tacrolimus 7mg.
Conceptual timeline depicting course from initial diagnosis of COVID-19 to kidney transplantation and most recent follow-up of both recipients (labelled in red) and live donor to second recipient (labelled in purple). (abbreviations: S- in the box refers to days with symptoms, DDTx: deceased donor transplant (recipient 1), eGFR: estimated glomerular filtration rate in ml/min/m2).
The second case was a 35-year-old female, on haemodialysis and was being worked up for live related kidney transplant, with her sister as prospective donor. Unfortunately, both the donor and the recipient developed fever, sore throat, myalgia and tested positive for COVID-19 by RT-PCR. Luckily, the disease course was not severe, and they only required quarantine and symptomatic treatment. Both donor and recipient were negative for COVID-19 RT-PCR done at 1, 2 and 6 weeks. However, both of them were positive for IgG titres against SARS-CoV-2 (by CLIA) at 6 weeks. A laparoscopic left kidney donor nephrectomy was then performed followed by a successful graft anastomosis. Induction was not given and standard triple drug immunosuppressive regime was prescribed. Post-operative period was uneventful and graft functions remained good at the last follow-up (at 14 weeks, at the time of writing this report, eGFR of 83ml/min/1.73m2) (Fig. 2). Her present immunosuppression included prednisolone 10mg, mycophenolate mofetil 1500mg and tacrolimus 3mg daily.
COVID-19 has brought about a complete stand still of transplant programmes across the globe.1,2
Dialysis and transplant population are both subject to morbidity and mortality from COVID-19.3 As a result, there is a dilemma if transplants should be undertaken or not. Guidelines regarding the indications and timing of kidney transplants during this pandemic lack good evidence.4 The current guidelines of our country do not recommend COVID-19 positive live donor and are silent on COVID-19 infection in prospective recipients.5 They also fail to give timelines for sequential retesting in these individual. We feel that these guidelines need to be updated in view of rapidly evolving transplant scenarios. A certain subset of dialysis patients do not do well on dialysis or may even die, owing to a lack of transplant. To support these patients, most of the centres offering transplant programmes continue to do so by keeping in mind, their infrastructure to deliver quality service and their medical capacity.
In the current scenario, there is little to no data on the appropriate management of dialysis patients and ideal wait-times for transplant surgeries for those who have recovered from COVID-19. Till date, there is only one documented case of deceased donor transplant in medical literature, wherein a 28-year-old woman underwent kidney transplant after recovering from COVID-19.6 In this case, wait time for transplant after initial diagnosis of COVID-19 was 6 weeks and RT-PCR for SARS-CoV-2 was negative twice in third week as well as pre-operative. Her renal functions were reported to be normal at 60 days post-transplant.
We herein report two cases of kidney transplant after recovery from COVID-19 infection, one of which was a laparoscopic live donor kidney transplant. Ironically, the donor and the recipient both were positive for SARS-CoV-2. This is the first case report of a successful live renal transplant where both recipient and donor had COVID-19 infection. The other patient is the first reported patient in the world with COVID-19 pneumonia who underwent kidney transplant after recovery from pneumonia. Both cases were negative for COVID-19 at the time of transplant. Transplant nephrologists have a challenging task to choose the ideal patient who deserves a timely transplant during this pandemic. They also have the responsibility to prevent and treat COVID-19 in these recipients. COVID-19 is expected to continue for months from now with no definite cure or effective vaccine in immediate future. Kidney disease can be more deadly than COVID-19 itself in some patients. The balancing act of transplant and immunosuppression in the era of COVID-19 will be an uphill task for the Nephrology community with more lessons to be learnt.
Consent: Informed and written consent has been taken from both patients.