To the Editor,
In a typical case of sarcoidosis, the patient will present with pulmonary lesions, be diagnosed, and later develop renal disorder. Nevertheless, in rare cases, renal symptoms may precede pulmonary symptoms.1-3
In this article, we present the case of a male patient aged 18 years, employed as an animal caregiver. He was admitted to the emergency department of his referral hospital due to a long-term fever, and while hospitalised, he developed sub-acute renal failure. He was subsequently referred to our department for evaluation; with plasma creatinine (PCr) values of 6mg/dl.
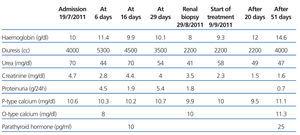
He had experienced a high fever during 2 months, which began a week after a suspicious tick bite. Fever was present daily following no particular schedule, and he also had night sweating. The local hospital had provided him with different empirical antibiotic treatments for a suspected case of boutonneuse fever or other infectious diseases. Upon admission, antibiotic treatment had been discontinued for 20 days and fever persisted. Results from the analysis upon admission are shown in Table 1. Other relevant data: circulating immune complexes, 54.9µg/ml; 1.25(OH)2D, 8.6pg/ml; 25(OH)D, 8.1pg/ml; ACE, 23IU/l. All results were negative for a wide-range of infections. Thoracic x-ray: normal upon admission; 1 month later, signs of small bibasilar pulmonary infiltrates with halo sign. Axial computed tomography was normal. Renal ultrasound was normal. The lung scintigraphy image is shown in Figure 1.
The decrease in renal function initially suggested a pre-renal +/- post-infectious origin, possibly in association with acute tubular necrosis. During the first days, renal function improved progressively before worsening once again, with values returning to those measured upon admission (Figure 2). Proteinuria, which was initially in the non-nephrotic range (1-2g/24h), later reached the nephrotic range (Figure 2). In light of the above data, doctors decided to perform a renal biopsy (26 August 2011). After receiving the results from the biopsy and the lung scintigraphy, treatment was initiated with prednisone 1mg/kg/day; the fever resolved, PCr improved (1.5mg/dl) and proteinuria also improved.
Our final diagnosis was stage II chronic kidney disease secondary to sarcoidosis with mild hypercalcaemia and granulomatous interstitial nephritis +/- associated with glomerular process, secondary hypoparathyroidism and distal tubular acidosis secondary to interstitial nephritis.
DISCUSSION
Hypercalcaemia is the most frequently detected abnormality in sarcoidosis, and is present in between 10% and 15% of cases. The mechanism leading to hypercalcaemia works due to activated macrophages in the lungs and lymph nodes being capable of increasing calcitriol production. In our patient, 1,25(OH) and 25(OH) vitamin D levels were low, possibly due to the long period of hospitalisation without exposure to sunlight. In addition, we detected severe suppression of parathyroid hormone (PTH) despite the fact that PTH levels should have been higher according to the patient's stage of chronic kidney disease. We concluded that the decrease in PTH levels was caused by hypercalcaemia, despite the fact that vitamin D values were not elevated.4,5
Approximately 20% of patients with sarcoidosis have a granulomatous renal disease. Granulomatous interstitial nephritis is common in sarcoidosis6,7; however, development of manifest clinical symptoms of renal failure is unusual. In the case in question, however, the patient did present evident kidney disease, and made good progress when treated with steroids. The decrease in renal function in such cases is mild to moderate, and on other occasions, glycosuria, renal tubular acidosis and abnormal values due to tubular damage have been observed. This was probably also true for our patient, who suffered from metabolic acidosis throughout the hospital stay, with polyuria, no aminoaciduria, and requiring oral bicarbonate even when renal function was at its best levels. For this reason we suspected distal tubular acidosis, and the condition resolved with treatment.8
Lastly, glomerular damage in sarcoidosis is the third and least frequent form of renal involvement. Membranous glomerulonephritis is the most widely-documented histological form, and nephropathy with minimal changes (which we suspected of in our patient) is rarely observed. It progresses clinically with varying levels of proteinuria, and it is frequently accompanied by nephrotic syndrome with active sediment. In our case we did not detect complete nephrotic syndrome, but proteinuria within the nephrotic range was found in some samples, and this cannot be attributed to the tubular disease alone. For this reason, and given the absence of glomerular disease according to the simple microscope image and the absence of immune deposits, we believe that an additional glomerular process was involved. We think that minimal lesions were present, but cannot confirm this hypothesis since no electron microscope examination was made that would confirm presence of such lesions.9,10
Our case stands out because our patient presented all 3 basic kidney abnormalities that can be caused by sarcoidosis (and response to treatment was excellent). It was also interesting that he would experience hypoparathyroidism and distal tubular acidosis, both secondary to sarcoid infiltration.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Table 1. Evolution of analysis results
Figure 1. Lung scintigraphy of sarcoid lesions
Figure 2. Table showing evolution of proteinuria and renal function