We present the Spanish adaptation of the 2021 European Guidelines on Cardiovascular Disease (CVD) prevention in clinical practice. The current guidelines besides the individual approach greatly emphasize on the importance of population level approaches to the prevention of cardiovascular diseases. Systematic global CVD risk assessment is recommended in individuals with any major vascular risk factor. Regarding LDL-Cholesterol, blood pressure, and glycemic control in patients with diabetes mellitus, goals and targets remain as recommended in previous guidelines. However, it is proposed a new, stepwise approach (Step 1 and 2) to treatment intensification as a tool to help physicians and patients pursue these targets in a way that fits patient profile. After Step 1, considering proceeding to the intensified goals of Step 2 is mandatory, and this intensification will be based on 10-year CVD risk, lifetime CVD risk and treatment benefit, comorbidities and patient preferences. The updated SCORE algorithm—SCORE2, SCORE-OP— is recommended in these guidelines, which estimates an individual’s 10-year risk of fatal and non-fatal CVD events (myocardial infarction, stroke) in healthy men and women aged 40–89 years. Another new and important recommendation is the use of different categories of risk according different age groups (< 50, 50−69, ≥70 years).
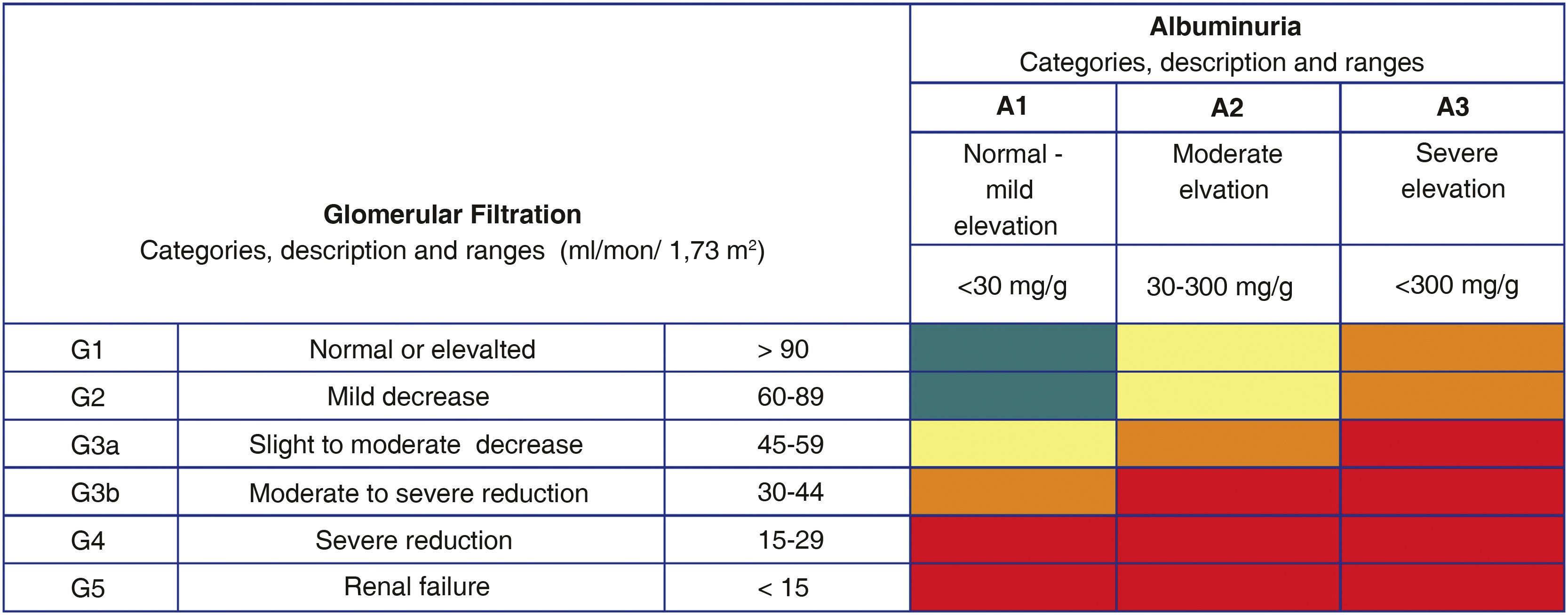
Different flow charts of CVD risk and risk factor treatment in apparently healthy persons, in patients with established atherosclerotic CVD, and in diabetic patients are recommended. Patients with chronic kidney disease are considered high risk or very high-risk patients according to the levels of glomerular filtration rate and albumin-to-creatinine ratio. New lifestyle recommendations adapted to the ones published by the Spanish Ministry of Health as well as recommendations focused on the management of lipids, blood pressure, diabetes and chronic renal failure are included.
Presentamos la adaptación española de las Guías Europeas de Prevención Cardiovascular 2021. En esta actualización además del abordaje individual, se pone mucho más énfasis en las políticas sanitarias como estrategia de prevención poblacional. Se recomienda el cálculo del riesgo vascular de manera sistemática a todas las personas adultas con algún factor de riesgo vascular. Los objetivos terapéuticos para el colesterol LDL, la presión arterial y la glucemia no han cambiado respecto a las anteriores guías, pero se recomienda alcanzar estos objetivos de forma escalonada (etapas 1 y 2). Se recomienda llegar siempre hasta la etapa 2, y la intensificación del tratamiento dependerá del riesgo a los 10 años y de por vida, del beneficio del tratamiento, de las comorbilidades, de la fragilidad y de las preferencias de los pacientes. Las guías presentan por primera vez un nuevo modelo para calcular el riesgo SCORE2 y SCORE2-OP de morbimortalidad vascular en los próximos 10 años (infarto de miocardio, ictus y mortalidad vascular) en hombres y mujeres entre 40 y 89 años. Otra de las novedades sustanciales es el establecimiento de diferentes umbrales de riesgo dependiendo de la edad (<50, 50−69, ≥70 años).
Se presentan diferentes algoritmos de cálculo del riesgo vascular y tratamiento de los factores de riesgo vascular para personas aparentemente sanas, pacientes con diabetes y pacientes con enfermedad vascular aterosclerótica. Los pacientes con enfermedad renal crónica se considerarán de riesgo alto o muy alto según la tasa del filtrado glomerular y el cociente albúmina/creatinina. Se incluyen innovaciones en las recomendaciones sobre los estilos de vida, adaptadas a las recomendaciones del Ministerio de Sanidad, así como aspectos novedosos relacionados con el control de los lípidos, la presión arterial, la diabetes y la insuficiencia renal crónica.
The new European cardiovascular (CV) prevention guidelines1 have been published 5 years after the last ones of 2016,2 although an update was made in 2020,3 of which the Spanish Interdisciplinary Committee for Vascular Prevention made a critical commentary.4
The 2021 guidelines have been elaborated by 13 European scientific societies and have introduced noteworthy novelties that are discussed below. In addition to the individual approach to CV prevention, they make special emphasis on the population and public health strategy, which the Spanish Interdisciplinary Committee for Vascular Prevention has always considered highly relevant, as reflected in the documents being published and the programs of the biennial conferences organized by the Ministry of Health. These guidelines are more complex than the previous ones because they seek a more personalized approach, which certainly reflects the phenotypic diversity of the patients seen in clinical practice.
Assessement of vascular riskThe new CV prevention guidelines recommend calculating vascular risk (VR) systematically in all adults with any VR factor, and it can also be considered in men >40 years and women >50 years, and that can be repeated every 5 years. Some publications5 have evidenced potential risks of labeling individuals as low VR, as they may be perceive false reassurance that they are protected from vascular disease, compromising their motivation for risk factor prevention. The majority of the population is in these risk groups (moderate or low), where more cases of vascular disease occur in absolute numbers. For this reason, it is essential to promote healthy lifestyles in the entire population.
The therapeutic targets for low-density lipoprotein cholesterol (LDL-C), blood pressure (BP), and glycemia have not changed with respect to the previous guidelines, but the way in which they are controlled in the individuals has been modified, in a stepwise fashion (stages 1 and 2). This approach is not conceptually new, and reflects the usual clinical practice of progressive intensification of therapeutic strategies, as part of a shared decision-making process between health professionals and patients. It is always recommended to reach stage 2, and treatment intensification will depend on 10-year and lifetime risk, treatment benefit, comorbidities, frailty and patient preferences. However, we should not forget that according to the results of the EUROASPIRE study6 conducted in 27 European countries, we are still far from achieving therapeutic targets (71% of people with coronary artery disease had a c-LDL≥70mg/dl), and this staged strategy could facilitate inertia, compromising the achievement of targets as soon as possible, especially in patients with high or very high VR. Therefore, in patients with high or very high VR, particularly those who have already suffered a vascular event, we continue to recommend strict achievement of c-LDL targets along with reduction ≥50% of c-LDL from baseline in a single phase and as soon as possible. Regardless of risk, it is reccomended smoking cessation, adoption of a healthy lifestyle, and having a systolic blood pressure (SBP)<140mmHg for all individuals.
The guidelines present for the first time a new model for calculating risk-SCORE27 and SCORE2-OP8—which has been calibrated for 4 European regions according to vascular mortality rates, and Spain belongs to the countries with low VR. This tool allows calculation of the risk of vascular morbidity and mortality in the next 10 years (myocardial infarction, stroke, and vascular mortality) in men and women between 40 and 89 years of age. The colored tables that appear in the guidelines (using SBP, age, sex, smoking, and non-high-density lipoprotein cholesterol), the App of the European Society of Cardiology, or the tool available on the web (https://u-prevent.com), allows the entry of total and high-density lipoprotein cholesterol. Using these applications it is also possible to calculate lifetime VR (LIFE-CV model) and the benefits of treatment in terms of years of life gained without vascular disease. In addition, there are specific tools for calculating risk in people with diabetes (ADVANCE risk score or DIAL model) and with established vascular disease (SMART REACH score or SMART REACH model).
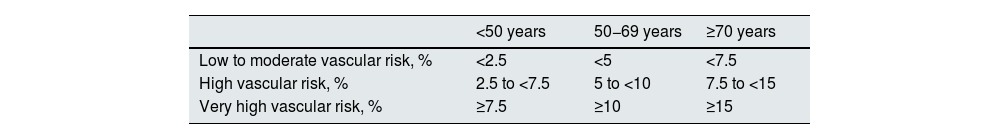
Categories of vascular risk according to SCORE2/SCORE2-OP in apparently healthy individualsAnother substantial novelty is the establishment of different risk thresholds depending on age, as shown in Table 1. This is in contrast to previous versions, which established a single risk threshold, in order to avoid undertreatment in young people and overtreatment in older people, since the long-term benefit of treatment of VR factors is greater in young patients.
Vascular risk categories according to age groupsa.
| <50 years | 50−69 years | ≥70 years | |
|---|---|---|---|
| Low to moderate vascular risk, % | <2.5 | <5 | <7.5 |
| High vascular risk, % | 2.5 to <7.5 | 5 to <10 | 7.5 to <15 |
| Very high vascular risk, % | ≥7.5 | ≥10 | ≥15 |
It is recommended to treat all very high-risk individuals and treatment should be considered for those at high risk, depending on risk modifiers, lifetime risk, treatment benefits, and personal preferences.
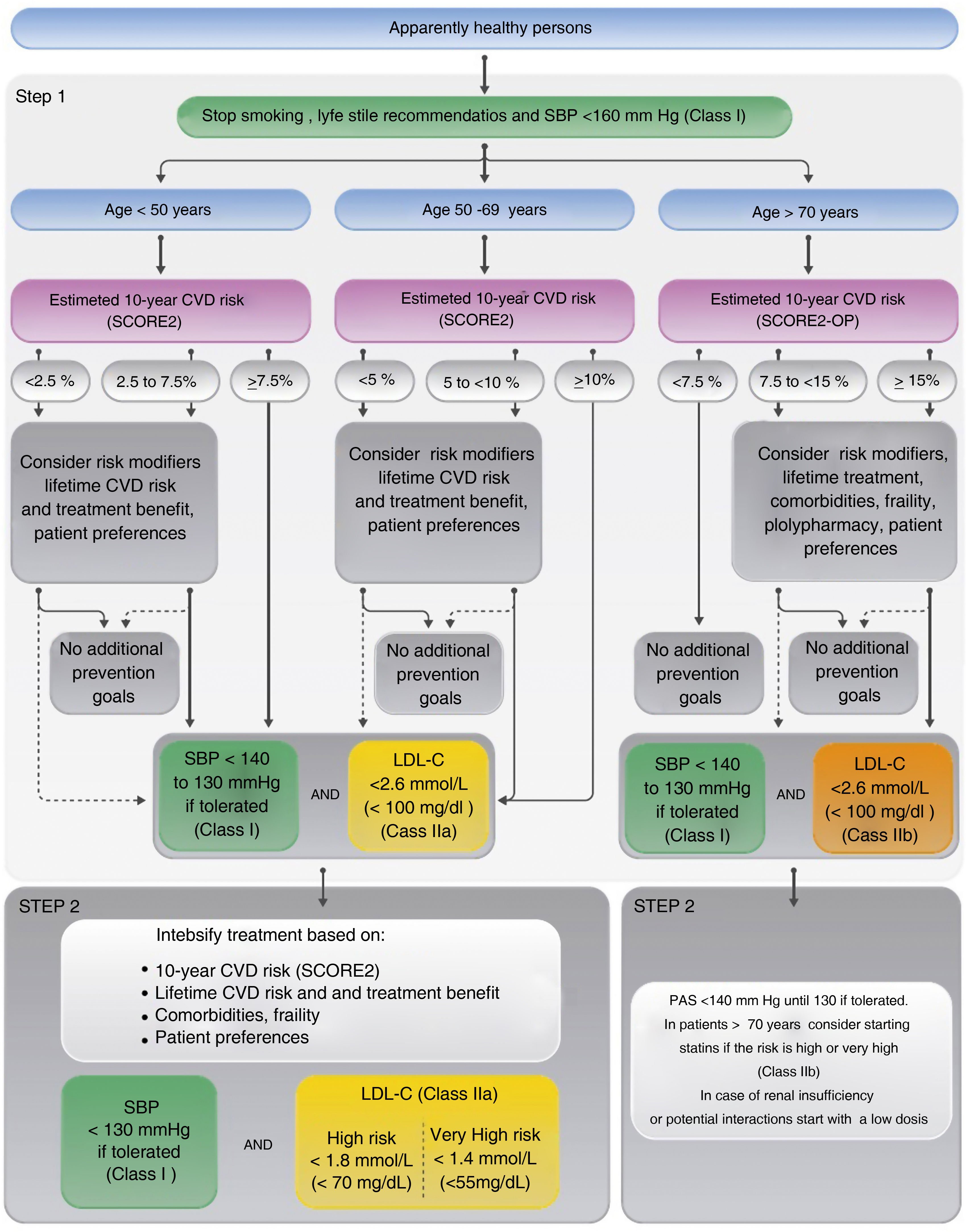
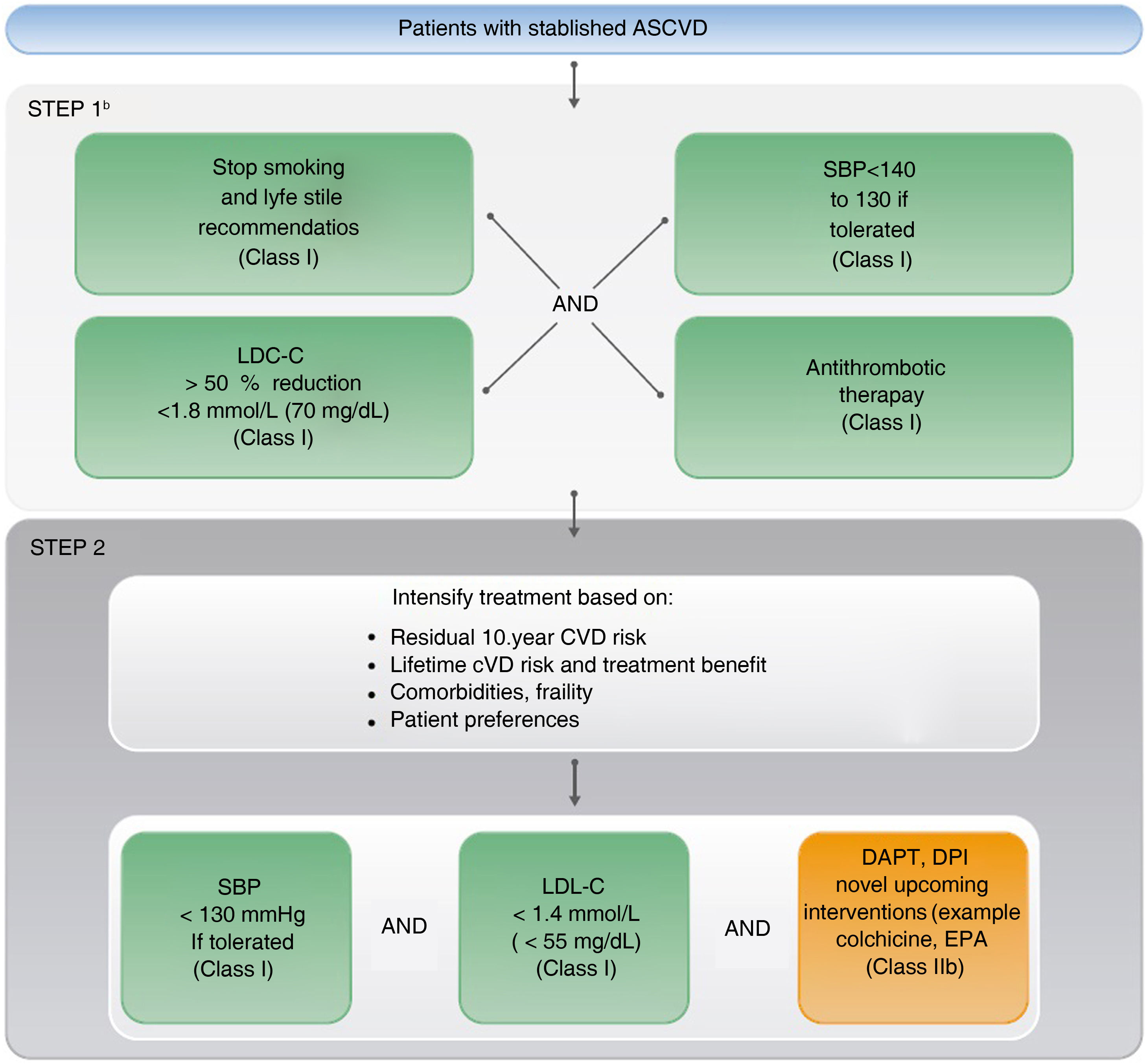
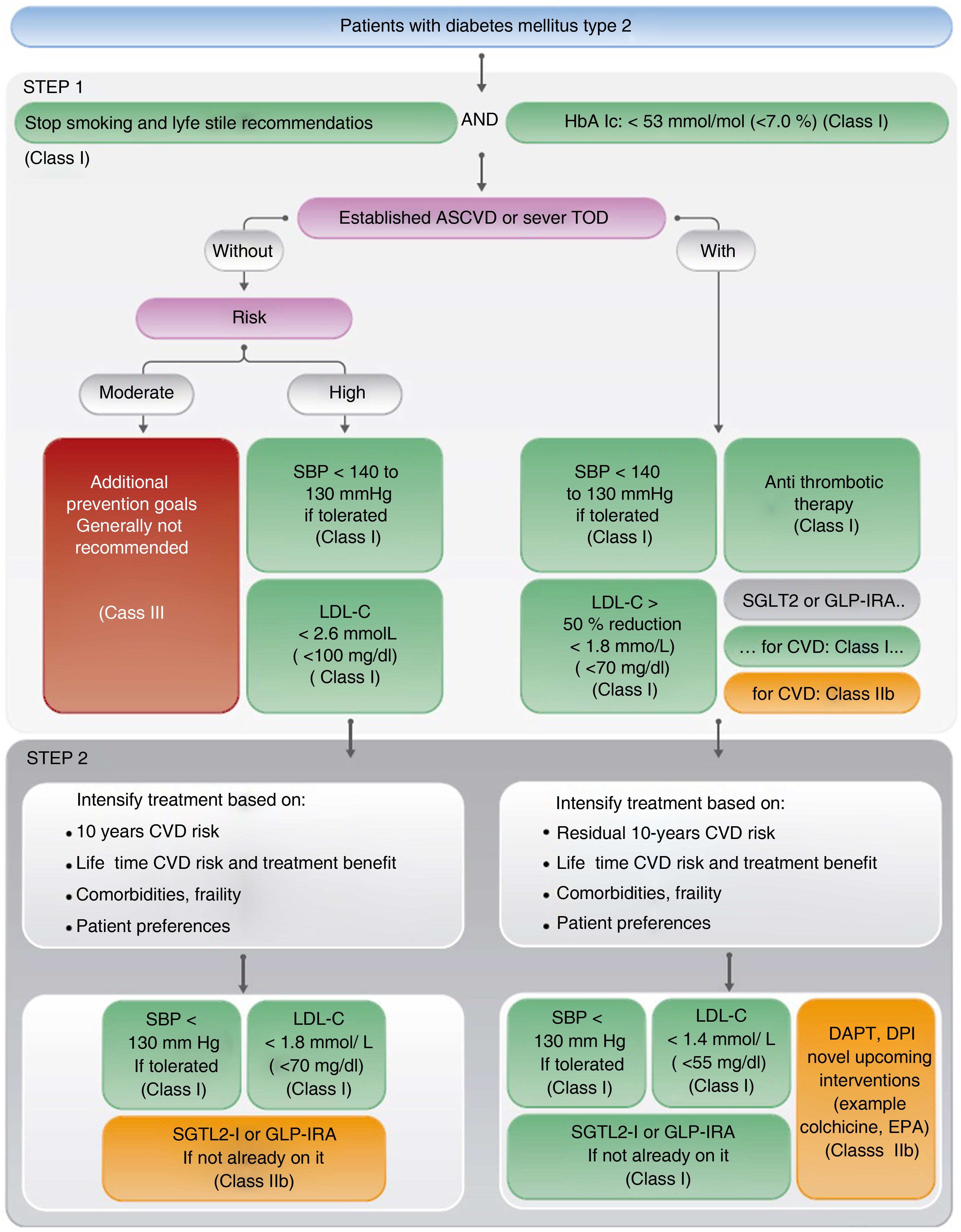
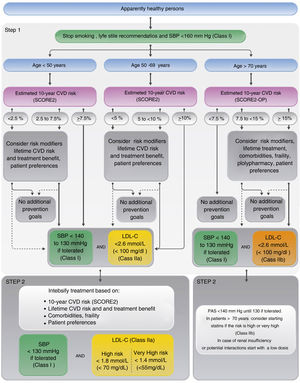
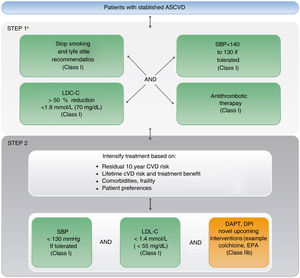
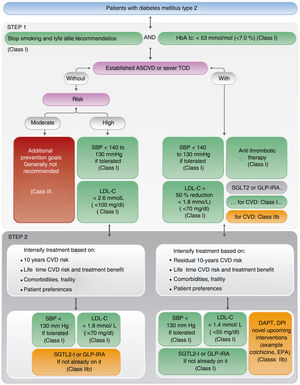
Figs. 1–3 outline the algorithms for VR calculation and treatment of VR factors for apparently healthy individuals, patients with atherosclerotic vascular disease, and patients with diabetes. Patients with chronic kidney disease (CKD) will be considered high or very high risk based on glomerular filtration rate and albumin/creatinine ratio (ACC). Patients with familial hypercholesterolemia are considered high risk.
Vascular risk algorithm and therapeutic targets in apparently healthy patients.
Adapted from Visseren et al.1 (Fig. 6, p. 26).
CV, cardiovascular; C-LDL, low-density lipoprotein cholesterol; SBP, systolic blood pressure; SCORE2, Systematic Coronary Risk Estimation 2; SCORE2-OP, Systematic Coronary Risk Estimation 2-Older Persons.
Algorithm of therapeutic targets and pharmacological treatment in patients with established vascular disease.
Adapted from Visseren et al.1 (Fig. 7, p. 27).
CV, cardiovascular; DAPT: dual antiplatelet therapy; DPI: dual pathway inhibition; C-LDL: low-density lipoprotein cholesterol; CVD: cardiovascular disease; SBP, systolic blood pressure; EPA: eicosapentaenoic acid.
Vascular risk algorithm, therapeutic objectives and pharmacological treatment in patients with diabetes.
Adapted from Visseren et al.1 (Fig. 8, p. 29).
C-LDL, low-density lipoprotein cholesterol; DAPT, dual antiplatelet therapy; DPI, dual pathway inhibition; CVD, cardiovascular disease; GLP-IRA, glucagon-like peptide type 1 receptor agonists; HbAIc, glycosylated hemoglobin; LOD, target organ damage; SBP, systolic blood pressure; SGLT2-i, sodium-glucose cotransporter inhibitors; EPA, eicosapentaenoic acid.
The importance of communication with the patient is highlighted, recommending an informed discussion about the risk and therapeutic benefits, adapted to the needs of the individual. Specifically, the need for lifelong use of VR is discussed, especially in younger patients, or the lifelong benefits after the intervention or vascular age.
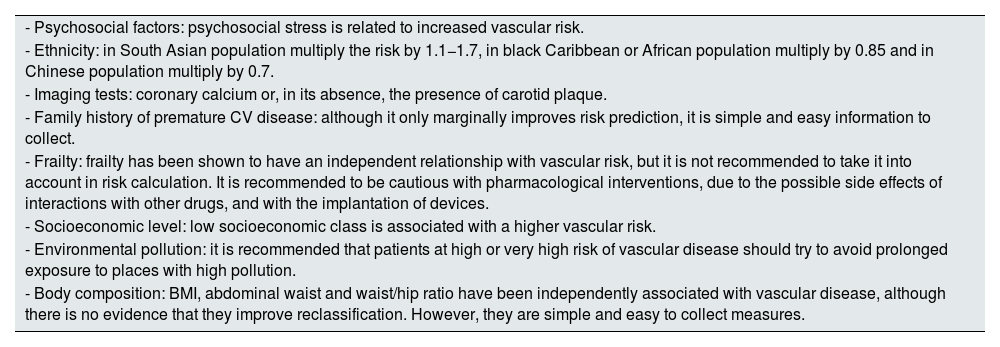
Risk modifiersFew risk modifiers meet the criteria to be considered in the calculation VR: improve prediction (discrimination and reclassification), have a clear impact in public health (number of patients to be treated or screened) and be feasible to implement in clinical practice. Table 2 summarizes the most relevant modifiers.
Risk modifiers.
| - Psychosocial factors: psychosocial stress is related to increased vascular risk. |
| - Ethnicity: in South Asian population multiply the risk by 1.1−1.7, in black Caribbean or African population multiply by 0.85 and in Chinese population multiply by 0.7. |
| - Imaging tests: coronary calcium or, in its absence, the presence of carotid plaque. |
| - Family history of premature CV disease: although it only marginally improves risk prediction, it is simple and easy information to collect. |
| - Frailty: frailty has been shown to have an independent relationship with vascular risk, but it is not recommended to take it into account in risk calculation. It is recommended to be cautious with pharmacological interventions, due to the possible side effects of interactions with other drugs, and with the implantation of devices. |
| - Socioeconomic level: low socioeconomic class is associated with a higher vascular risk. |
| - Environmental pollution: it is recommended that patients at high or very high risk of vascular disease should try to avoid prolonged exposure to places with high pollution. |
| - Body composition: BMI, abdominal waist and waist/hip ratio have been independently associated with vascular disease, although there is no evidence that they improve reclassification. However, they are simple and easy to collect measures. |
CV: cardiovascular; BMI: body mass index.
The Spanish Interdisciplinary Committee for Vascular Prevention has adapted the recommendations of the new guidelines based on those of the World Health Organization and the Ministry of Health. It is recommended:
- -
Perform moderate physical activity at least between 150 and 300min a week (or between 75 and 150 of vigorous activity or an equivalent combination of both) and practice at least 2 days a week muscle strengthening, bone mass improvement and flexibility activities.9,10
- -
Reduce sedentary periods, with active breaks every 1 or 2h, increase active transport and limit time in front of a screen.9,10
- -
Adopt a healthy and sustainable diet based on fresh, seasonal and local foods: eat at least 5 servings of fruit and vegetables per day, whole grains, prioritize vegetable protein (legumes, nuts) and fish, preferably blue fish, incorporating eggs, chicken, natural yogurt and milk in moderation, and avoid red or processed meats, precooked foods, industrial pastries and sugary drinks.11
- -
Avoid consumption of alcoholic beverages, as this is the only recommendation that avoids the risks associated with their consumption. If consumed, the less the better, and always below the low-risk consumption limits: 10g/day (one standard drinking unit) in women and 20g/day (2 standard drinking units) in men,12 leaving a few days a week free without alcohol and avoiding heavy drinking episodes; and in <18 years of age, during pregnancy and breastfeeding, consumption should be completely avoided.
- -
Abandon tobacco use in any form, including heated tobacco and related products such as electronic cigarettes, and avoid environmental exposure to tobacco smoke.
- -
Lipids: a stepwise approach of treatment intensification is advised in apparently healthy individuals with high or very high VR and in patients with vascular disease or diabetes, taking into account VR, treatment benefit, risk modifiers, comorbidities, and personal preferences. In patients who have had vascular disease, in order to reach therapeutic c-LDL targets as soon as possible, it is recommended to go directly to stage 2 (see section on VR). High-intensity statins are recommended in very high-risk individuals or those with vascular disease, and if c-LDL targets are not achieved, ezetimibe should be added, and if targets are still not achieved, a PCSK9 inhibitor should be added. Although this recommendation is in line with achieving 2-stage targets, it is difficult to achieve reductions ≥50% in c-LDL, except with maximal doses of atorvastatin and rosuvastatin. The available evidences allows changing the terminology of high-potency statins to high-intensity lipid-lowering therapies.13 Thus, the first option in patients with high or very high VR could be the use of non-maximal doses of statins (atorvastatin 40mg or rosuvastatin 10mg) associated with ezetimibe, which facilitate the achievement of therapeutic targets with better tolerance and adherence. Adding n-3 fatty acids (ethyl icosapentate 2×2g/day) to statin therapy could be considered in high or very high risk patients with mild/moderate hypertriglyceridemia (with triglyceride levels above 150mg/dl).
- -
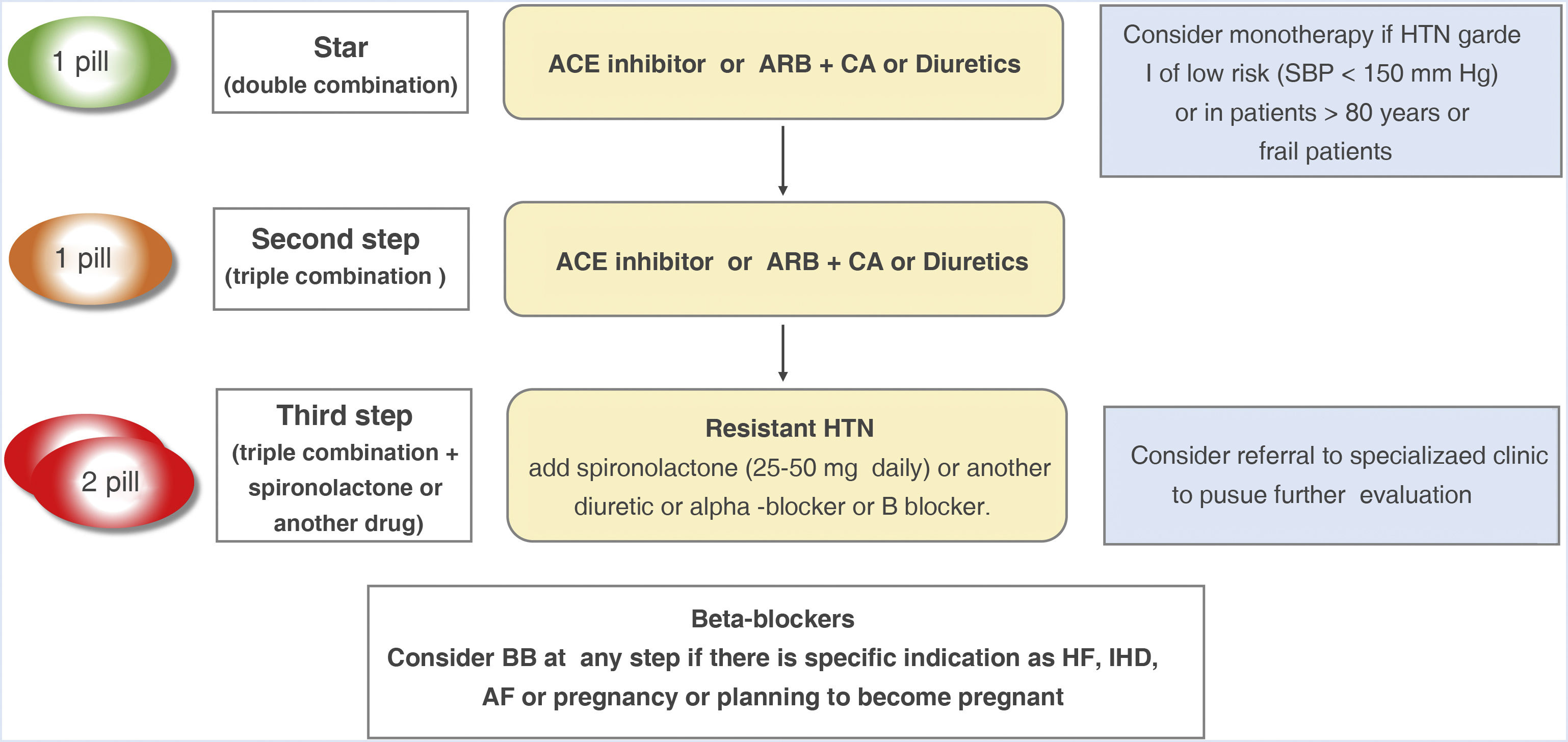
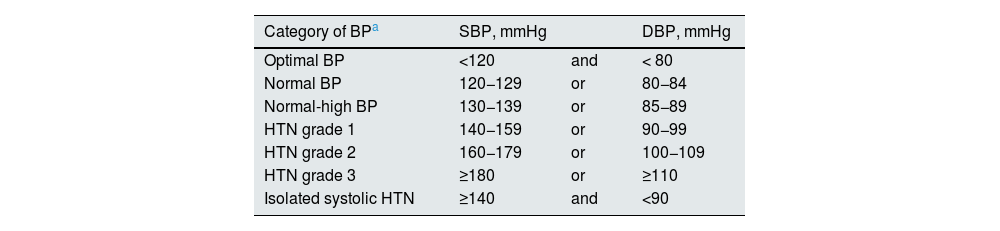
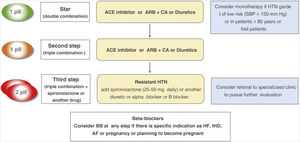
Arterial hypertension (HTN): in contrast to the American guidelines (ACC/AHA 2017), the same classic threshold is still recommended for the definition of HTN and for classification into optimal BP, normal BP, normal-high BP and HTN grades 1–3 (Table 3). The Spanish Society of Hypertension-Spanish League for the Fight against Arterial Hypertension published a position paper justifying the convenience of maintaining the same cut-off point for the definition of HTN.14 It is recommended that treatment be initiated in persons with grade 1 HTN taking into account the VR, the lifetime benefit, and the presence of target organ involvement. Nevertheless, despite the evidence on the benefit of BP lowering in reducing vascular morbidity and mortality, BP control in Europe and other parts of the world is suboptimal, especially in countries with a medium or low level of income,15 and it has worsened in recent years.16 Although the cause is multifactorial, poor adherence plays a relevant role. The recommended strategy for initial treatment continues to be the use of pharmacological combinations, with an angiotensin-converting enzyme inhibitor or an angiotensin II receptor antagonist associated with a thiazide diuretic or a long half-life calcium antagonist (Fig. 4). A recent meta-analysis has shown that this strategy improves adherence and the rate of control in patients with hypertension.17
Table 3.Clinical blood pressure classification (obtained at the out patient clinic) and degrees of hypertension.
Category of BPa SBP, mmHg DBP, mmHg Optimal BP <120 and < 80 Normal BP 120−129 or 80−84 Normal-high BP 130−139 or 85−89 HTN grade 1 140−159 or 90−99 HTN grade 2 160−179 or 100−109 HTN grade 3 ≥180 or ≥110 Isolated systolic HTN ≥140 and <90 Current guidelines on the diagnosis and treatment of arterial hypertension (HTN) indicate the need to know ambulatory blood pressure (BP) levels by ambulatory blood pressure monitoring (ABPM) or self-measurement of blood pressure (ABPM), given the high prevalence of white coat HTN and masked HTN.
DBP, diastolic blood pressure; SBP, systolic blood pressure.
aDefinitions are based on BP measured seated in the office. BP for classification will be based on the mean of 2 or more readings, in 2 or more occasions, following standardized recommendations for quality measures. Subjects with SBP and DBP in different categories will be classified in the highest category.
Fig. 4.Strategy for the treatment of arterial hypertension (HTN) without associated clinical complication.
This basic strategy is also valid for most patients with subclinical target organ damage, diabetes, cerebrovascular disease and peripheral arterial disease. There are specific algorithms for patients with ischemic heart disease (IHD), chronic kidney disease, heart failure (HF) and atrial fibrillation (AF).
ARB, angiotensin II receptor antagonist; BB, betablockers; CA, calcium antagonist; ACEI, angiotensin-converting enzyme inhibitor; ACE, angiotensin receptor blocker; Comp: tablet; SBP, systolic blood pressure.
- -
Diabetes mellitus: metformin is recommended as first-line treatment of diabetes mellitus (DM) with monitoring of renal function, for use especially in patients without vascular disease, chronic renal or cardiac failure. In these cases, in addition to the use or not of metformin, it isrecommended the treatment with glucagon-like peptide type 1 receptor agonists or sodium-glucose cotransporter (iSGLT2) inhibitors that have demonstrated a reduction in vascular and renal episodes. In patients with DM and CKD, iSGLT2 is recommended for vascular and renal benefits. In patients with DM and reduced ejection fraction, iSGLT2 is recommended to reduce hospitalizations for heart failure and vascular deaths.
- -
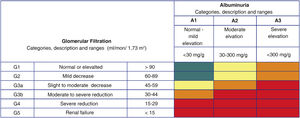
CKD: In CKD, the estimated glomerular filtration rate (eGFR) and urine ACR, determines prognosis (Fig. 5). In patients without DM, having a GFR<30ml/min/1.73m2 or a GFR<30−44ml/min/1.73m2 with ACR>30mg/g carries a very high risk of vascular events, as if the patient have had a previous vascular event. In addition, having GFR 30−44ml/min/1,73m2 and ACR <30mg/g or GFR 45−59ml/min/1,73m2 and ACR 30−300mg/g or FGe≥60ml/min/1,73m2 and ACR>300mg/g conditions an elevated risk of vascular events.18 In patients with DM, the presence of a GFR<45ml/min/1.73m2 or GFR 45−59ml/min/1.73m2 and ACR 30−300mg/g or ACR>300mg/g is considered as severe target organ injury, as it is the presence of microvascular complications at 3 different sites, which confers a situation of very high VR. In patients with CKD there are recommended, general measures of smoking cessation and lifestyle optimization, SBP control between 130 and 140mmHg and diastolic <80mmHg BP, according to tolerance, and c-LDL targets lower than 70mg/dl or 55mg/dl in patients with high or very highVR. In patients with DM and diabetic renal disease, the use of hypoglycemic drugs with recognized renal protective effects is recommended.
Fig. 5.Risk related to chronic kidney disease according to glomerular filtration rate and albuminuria categories (expressed as albumin/creatinine ratio).
Areas in green, baseline risk (no kidney disease if no other defining markers are present); areas in yellow, moderate risk; areas in orange, high risk; areas in red, very high risk.
Kidney Disease: Improving Global Outcomes (KDIGO) guidelines on chronic kidney disease.
- -
Antithrombotic therapy: the addition of a second antithrombotic drug (platelet P2Y12 receptor inhibitor or low-dose rivaroxaban) to aspirin should be considered in secondary prevention of vascular disease in patients with high ischemic risk and low risk of bleeding. Combined treatment with aspirin and low-dose rivaroxaban could be considered in patients with diabetes and peripheral arterial disease. Treatment with low-dose colchicine (0.5mg day) could be considered in secondary prevention of vascular disease if other RV factors are insufficiently controlled or in the presence of recurrent ischemic episodes despite optimal treatment.
Much more emphasis is placed on health policies as a population-based prevention strategy. The aim is to reduce the attributable risk of risk factors, that is, the burden of vascular disease that we can prevent by eliminating or reducing the prevalence of each factor. These strategies are based on Geoffrey Rose's paradigm, according to which small leftward shifts in the population distribution of risk factors have a large impact on the overall burden of disease.19 The guidelines and other recommendations of international organizations, such as the World Health Organization,20–22,24 propose the most cost-effective interventions at the population level to create environments that promote healthy lifestyles, modifying risk factors such as physical inactivity, unhealthy diet, tobacco and alcohol consumption,23,25 exposure to air and noise pollution24 (especially from road traffic), and acting on climate change. In addition, different methods (governmental, media communication and education, labeling and information of products, economic incentives), settings (schools, workplace, community) and actions are described for each of the methods reinforced by a level of evidence and a class of recommendation. The goal, and also the task for national, regional and local authorities, is to make easy what is healthy, creating environments where the default choices are health-promoting.
Recommendations to promote the practice of physical activity and reduce sedentary lifestyles include urban planning measures to facilitate active and healthy mobility, active transportation and increase the availability of spaces and equipment that facilitate physical activity in schools and the community environment. To promote healthy eating, legislative measures are included to ban or reduce caloric intake, salt, added sugars and saturated fats in prepared foods and beverages, fiscal measures (tax or incentive) on some foods and beverages, and availability of healthy meals in the menus served and in food vending machines in the school and work environment. Recommendations are also included, mainly legislative, to reduce tobacco and alcohol consumption: regulation of consumption in public places, availability and sale, advertising, labeling and packaging, pricing policies and the implementation of educational campaigns.21–25 Finally, it recommended to establish measures to reduce emissions of small particles and gaseous pollutants, the use of solid fuels and road traffic, and to limit carbon dioxide emissions to reduce CV morbidity and mortality.
The population-based approach can bring numerous benefits, such as reducing the gap in health inequalities, preventing other noncommunicable diseases that have common risk factors and determinants with vascular events, such as cancer, lung disease, and type 2 DM, and saving the health and social costs of vascular events that are avoided.
Conflict of interestThe authors declare that they have no conflicts of interest.