Due to the global burden represented by chronic kidney disease (CKD), the World Health Organization encouraged the implementation of renal protection programmes (RPP) to affect its incidence through prevention and control measures.
ObjectivesTo assess the effectiveness of a Colombian RPP in terms of its effect on the stage progression of CKD and the need for renal replacement therapy (RRT).
MethodsAn analytical study that monitored 2 cohorts of patients diagnosed with CKD. The study compares the behaviour of clinical and renal impairment indicators from patients exposed to a RPP with that of patients following conventional treatment (CT). The population of both intervention groups was considered when determining the sample size. The incidence rate was calculated as well as patient survival (Kaplan–Meier). In addition, a multivariate analysis (Cox) was used to calculate the influence that exposure to the RPP had on the outcomes of the patients following the RPP and those following CT.
ResultsThe patients exposed to the RPP took longer to advance to the next CKD stage and require RRT. The incidence rate for progression is higher for the patients following CT (0.050, CI 95%: 0.040–0.064) compared to those in the RPP (0.034, CI 95%: 0.030–0.039). The ratio of incidence rates was 1.480 (CI 95%: 1.21–1.90). The hazard of progression was lower for the RPP (HR: 0.855, CI 95%: 0.74–0.98), as was the hazard of requiring RRT (HR: 0.797, CI 95%: 0.606–1.049).
ConclusionsThe RPP is a secondary prevention strategy against CKD which has an effect on the stage progression of CKD and the need for RRT. Early patient detection has a positive effect on the outcomes studied.
Debido a la carga global de la enfermedad renal crónica (ERC), la Organización Mundial de la Salud fomentó programas de protección renal (PPR) para impactar en su incidencia con medidas de prevención y control.
ObjetivosEvaluar la efectividad de un PPR en Colombia sobre el progreso de estadio en ERC y el requerimiento de terapia de reemplazo renal (TRR).
MétodosEstudio analítico de seguimiento a 2 cohortes de pacientes con diagnóstico de ERC, que compara el comportamiento de indicadores clínicos y de deterioro renal entre pacientes expuestos a un PPR versus el tratamiento convencional (TC). Como tamaño de muestra se tuvo en cuenta el censo de la población de ambas aseguradoras. Se calculó la tasa de incidencia, la supervivencia (Kaplan Meier) y la influencia de la exposición al PPR sobre los desenlaces entre PPR y TC mediante un análisis multivariado (Cox).
ResultadosLos pacientes expuestos al PPR se demoraron más en hacer el primer progreso de estadio y en requerir TRR. La tasa de incidencia para progreso es mayor en TC (0,050; IC 95%: 0,040-0,064) que en PPR (0,034: IC 95%: 0,030-0,039). Razón de tasas de incidencia: 1,480 (IC 95%: 1,21-1,90). El riesgo instantáneo de progreso fue menor en PPR (HR: 0,855; IC 95%: 0,74-0,98), al igual que el riesgo de requerir TRR (HR: 0,797; IC 95%: 0,606–1,049).
ConclusionesEl PPR representa una estrategia de prevención secundaria en ERC que impacta en el progreso de estadio y requerimiento de TRR. La captación temprana de pacientes mejora dichos desenlaces.
Chronic kidney disease (CKD) is considered a global public health problem. One out of ten people suffers some degree of renal dysfunction that progresses silently, increasing the clinical manifestations in advanced stages that are usually irreversible and significantly affect the quality of life.1 Back in 2010, the global prevalence of this disease was 10.4% in males and 11.8% in females; also the total number of people with CKD around the world for that same year was over 400 millions, most of them from developing countries.2
Progression of the disease leads to end-stage renal disease (ESRD), requiring renal replacement therapy (RRT); at this stage, patients have major cardiovascular, metabolic, an cognitive disorders and mortality is high.3
The increased incidence of diabetes mellitus (DM) and high blood pressure (HBP), and poor lipid control and habits like smoking is associated with more new cases of renal disease,4,5 that are identified at initial stages meaning that in such patients strategies aimed at preventing progression to end-stages can be implemented even in individuals who are not sick but are at risk and responder to preventive measures.6 In Latin America, the prevalence of ESRD in RRT has increased significantly, in 2010 there were 660 per million; and renal transplants were 19.1 cases per million.7
The World Health Organization (WHO) proposed the implementation of renal protection programmes (RPP) aimed at impacting the global burden of CKD, improving its indicators and implementing prevention and control measures.8 As a consequence, large studies like KEEP and NHANES III, aiming at the early detection of the disease with an emphasis on more sensitive populations have be able to identify risk and prognostic factors that could help to minimize the impact on the patients’ health.9 In Latin America similar strategies have been implemented: in Mexico they have created a version of the KEEP,10 while countries like Uruguay and Chile, among others, have created national programmes to promote early diagnosis, adequate management, disease worsening prevention, and quality of life.11–14
In Colombia, the CKD is considered a disease that consume large amount of resources since 1993. According to Colombian legislation, health-promoting entities (HPE) affiliate patients to the Social Security System and in general promote secondary prevention and RRT.15 This study tried to evaluate the effectiveness of a RPP in Colombia by measuring progression to ESRD and requierement of RRT.
MethodsStudy designAnalytical study with follow-up of two dynamic cohorts of CKD patients to compare the development of clinical indicators, laboratory values, and indicators of renal impairment in patients exposed to a RPP versus patients on conventional therapy (CT).
Background and participantsThe population studied was the census of users of two Colombian HPEs. Retrospective information obtained from the electronic history records (HER) of both insurance companies was collected from the year the RPP started until the moment the study started. Then the information was obtained prospectively until completion of a five year follow-up. The inclusion criteria were: being affiliated to the HPE during follow-up and meeting the KDOQI clinical practice guidelines for CKD.16,17 Children under fifteen years of age and those registered in both institutions at the same time or in another during the period of study were excluded. The beginning of the follow-up was set at the moment of diagnosis of CKD or at the moment of inclusion in the RPP. Ethical support from the IRB/IEC of the institutions involved was granted.
Renal Protection Programme versus conventional treatmentThe RPP is a secondary prevention strategy that includes a protocol of educational and clinical appointments, with clinical and periodic lab exams focused on the active search for patients at risk. The RPP has a first level of healthcare for the follow-up of patients in the early stages of CKD with general practitioners (GP) and nurses and two annual appointments with the Internal Medicine and Nutrition units. The RPP has a second level of healthcare from CKD stage 3 or more of with appointments with the Internal Medicine, Nephrology, and Nutrition units every three or two months based on the stage of CKD. The lab exams are conducted one month prior to the appointment following the RPP technical guide.
The other group is on CT which provides first level healthcare both for patients at risk and for those with a diagnosis of CKD; referral to a specialist occurs based on the medical criterion from the treating GP and as requested by the patients. No guidelines or protocols of care are applied, and there is no active search for patients at risk.
VariablesVariables based on exposure (based on being exposed to the RPP or CT). The variables considered as criteria for the diagnosis of CKD were: creatinine clearance <60ml/min (estimated using the Cockroft–Gault formula), alterations in renal ultrasound, proteinuria >150ml/day, abnormal urinary sediment and, in diabetic patients microalbuminuria >30mg.16,17
Dependent variables: time from diagnosis to first stage progression, and time from diagnosis to need for RRT.
Independent variables: the clinical and lab characteristics.
Source of the data and measurementsInformation was gathered from databases provided by every HPE and data obtained from the active and progressive search from clinical charts of patients during the period of study.
Study sizeAn analysis of the population census of both insurance companies meeting the diagnostic criteria based on the KDOQI clinical practice guidelines was conducted.
Quantitative variables: the clinical markers such as of systolic blood pressure, diastolic blood pressure, fasting glycemia, glycosylated haemoglobin (HbA1c), total cholesterol, triglycerides, low and high density lipoproteins (LDL, HDL) and creatinine were dichotomically recodified as controlled/non-controlled variables based on what it is recognized by the scientific literature for each clinical parameter in CKD patients. The reference values to define a variable as controlled were: systolic blood pressure <130mmHg, diastolic blood pressure <80mmHg, glycemia <140mg/dL, HbA1c <7 per cent, total cholesterol <200mg/dL, triglycerides <150mg/dL, LDL <100mg/dL, HDL >40mg/dL and creatinine <1.2mg/dL.16,17 The glomerular filtration rate (GFR) was considered a progression variable based on each CKD stage. In some of the analyses it was preferred to group variables such as age, marital status, stage of the disease, total number of appointments, and clinical markers.
Statistical methodsPopulation was characterized for the diagnosis of CKD through frequency distributions and proportions for qualitative variable; for the quantitative variables, we used descriptive statistics and dispersion statistics; in addition, the type of distribution was assessed using the Kolmogorov–Smirnov or Shapiro–Wilk normality tests. In order to establish the differences between the RPP and CT, the Student's t test or the Mann–Whitney U test were used based on the distribution of the variables.
The rate of the different outcomes in RPP and CT was estimated. To this end, in the numerator was the number of new cases of first progression and requiring RRT, and in the denominator, the years of exposure from the moment of diagnosis of CKD. Also the ratio of the incidence rate with its corresponding confidence intervals (CI) at 95 per cent was estimated.
The Kaplan–Meier survival curves were used to assess stage progression and need for RRT per insurance company. Both models were adjusted for the different covariables and also for two subgroups based on stage: 1 and 2 as early entry, and 3 and 4 as late entry. Stage of disease, age, and gender were all analyzed comparatively (log rank test) in an effort to compare the progression in each stage. Cox proportional hazards analysis was used to analyze the influence of the exposure to RPP on each dependent variable adjusted for the other variables of interest. To compare progression, the late stages 3 and 4 were considered reference points since progression is lees, and stage 5 was not taken into account because it does not progress any further. On the contrary, to compare the need for RRT, the early stages 1 and 2 were considered reference points since late stages represented a too high risk of RRT. Covariables were included in the models based on clinical and statistical criteria (Hosmer–Lemeshow: p<0.25). Compliance with the proportional hazards assumption was tested graphically using Scaledsch and Schoenfeld scaled residuals in Stata Version 11.
ResultsParticipants and descriptive dataThere were 9887 clinical histories consulted; 56.5% corresponded to patients within the RPP and 43.5% to patients on CT. Overall, 5663 patients meet the inclusion criteria, 74.2% had been exposed to the RPP and 25.8% had been on CT. During follow-up there were 509 withdrawals (8.9%), 1010 losses to follow-up (17.8%), and 312 deaths (5%). The age of patients within the RPP was significantly lower than the age of patients on CT, with an average age of 66 (16–100) and 70 (20–97) years old, respectively. There were more male patients in the group on CT (64.5%; p<0.001).
The most frequent co morbidities in both groups were the following: high blood pressure (HBP) (94.67% for the RPP and 85.01%for CT; p<0.001); dyslipidemia (60.42% for the RPP and 63.8% for CT; p=0.023) and diabetes mellitus (DM) (36.2% for the RPP and 32.65% for CT; p=0.014). More than 30% of patients from the RPP were stage 1 and 2 patients while only 16.7% of patients on CT were stage 1 and 2 patients.
Main resultsAs compared to patients on CT, patients on RPP took longer to progress from one stage of the disease to the next, they expend more time until their first hospitalization, and also it took more time to require RTT. All these differences were clinically relevant and statistically significant (Table 1).
Months from the moment of diagnosis until different outcomes in patients with CKD from two Colombian HPEs.
| Event | RPP | CT | p* | ||
|---|---|---|---|---|---|
| Average (SD) | Median (Min-Max) | Average (SD) | Median (Min–Max) | ||
| 1st progression | 14 (10.1) | 12 (1–47) | 9.5 (7.2) | 8 (1–31) | <0.001 |
| 1st hospital stay | 14.7 (10.6) | 12 (1–47) | 11.5 (9.3) | 10 (1–47) | 0.002 |
| Need for RTT | 16.4 (9.9) | 16 (1–46) | 12.7 (7.2) | 11.5 (1–29) | 0.008 |
| Death | 20 (10.6) | 20 (1–46) | 13.2 (8.5) | 13 (1–41) | <0.001 |
| Follow-up | 24 (13.0) | 25 (1–49) | 19 (10.2) | 18 (1–46) | <0.001 |
SD, standard deviation; Max, maximum; Min, minimum.
In patients on RTT, a 24% progressed to next stage and in CT only 17% showed progression of disease stage (p<0.001). On the other hand, the percent of patients requiring RTT after follow-up was higher in patients on CT (5.1%) than in RPP (4.8 per cent) but p=0.802.
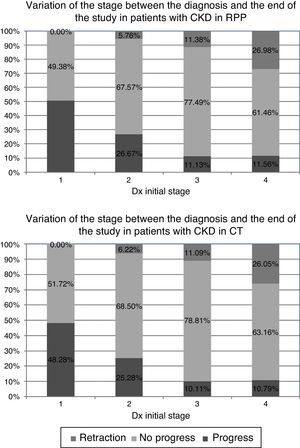
Stage progression and glomerular filtration ratePatients on the RPP showed more progression in the early stages of the disease. However, in later stages of CKD, both cohorts showed a tendency to stay in a given stage; but, patients within the RPP have a better control of renal function since a high percentage of these patients had a regression of the stage (Fig. 1).
The impairment of GFR was less in RPP than CT at the moment of diagnosis, and with the first and last changes of stage (Table 2). Among patients that progressed during follow-up, we found that patients on RPP showed more favourable GFR at the moment of diagnosis and during the first and last changes of stage than patients on CT. Such differences are clinically relevant and statistically significant (Mann–Whitney U test p<0.001 for the three instances).
Evolution of GFR in patients with CKD from two Colombian HPEs.
| TFG | RPP | CT | p* | ||||
|---|---|---|---|---|---|---|---|
| n | Average (SD) | Median (Min–Max) | n | Average (SD) | Median (Min–Max) | ||
| At the moment of diagnosis | 4.034 | 52 (23) | 48.9 (5.7–217.2) | 1.336 | 43.1 (19) | 41.1 (4.7–163.7) | <0.001 |
| 1st change of stage | 1.779 | 49.8 (24) | 53 (4.7–233.5) | 485 | 44.7 (25) | 34 (7.3–255) | <0.001 |
| Last change of stage | 1.778 | 49.2 (23) | 50.7 (4.6–233.5) | 485 | 44.5 (25) | 37.6 (7.3–255) | <0.001 |
SD, standard deviation; Max, maximum; Min, minimum.
In the group of patients who needed RRT during follow-up, we saw that patients within the RPP showed better glomerular filtration rates both at the moment of diagnosis and during the first and last changes of stage than patients on CT, though only the first of such differences was statistically significant (Mann–Whitney U test with p=0.022; 0.191; 0.051, respectively).
Incidence of progression renal disease and need for renal replacement therapyAt the end of the study the incidence rate (IR) of stage progression and need for RRT was recorded in both groups. RRT was needed in 204 patients on RPP, and in 74 patients on CT. Thus the IR for progression was greater for CT patients (0.050; 95% CI: 0.040–0.064) than RPP patients (0.034; 95% CI: 0.030–0.039). The IR ratio for such outcome was 1.48 (95% CI: 1.21–1.90). The IR for stage progression was not significantly different between the groups.
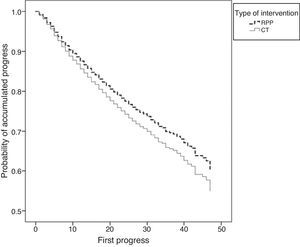
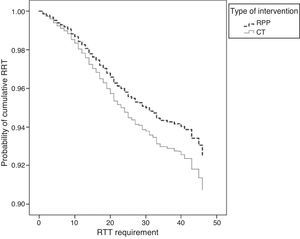
SurvivalKaplan–Meier curves adjusted for subgroups and other covariables showed that in both models the patients on RPP had less stage progression and less need for RTT than patients on CT (Figs. 2 and 3).
Cox proportional hazards analysisAnalysis of stage progression: hazards model adjusted for stage subgroups and different covariables showed that patients on RPP were significantly protected from stage progression (HR: 0.855; 95% CI 0.740–0.988). It was confirmed the influence on stage progression of age (HR: 1.623; 95% CI: 1.429–1.843), HBP (HR: 1.55; 95% CI: 1.209–1.988) and DM (HR: 1.216; 95% CI: 1.085–1.362). Also, patients in early stages of the disease had higher hazard ratios of stage progression (HR: 4.039; 95% CI: 3.554–4.590) while dyslipidemia turned out to be protective (Table 3).
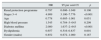
Hazards ratio for first stage progression adjusted for covariables in patients with CKD.
| HR | 95 per cent CI | p | |
|---|---|---|---|
| Renal protection programme | 0.855 | 0.740–0.988 | 0.034 |
| Stage 1–2 | 4.039 | 3.554–4.590 | <0.001 |
| Age | 1.623 | 1.429–1.843 | <0.001 |
| High blood pressure | 1.550 | 1.209–1.988 | 0.001 |
| Diabetes mellitus | 1.216 | 1.085–1.362 | 0.001 |
| Dyslipidemia | 0.891 | 0.794–0.999 | 0.048 |
| Gender (males) | 0.896 | 0.803–1.000 | 0.051 |
The hazard ratio for RRT was lower in the RPP (HR: 0.797; 95% CI: 0.606–1.049) although it was not statistically significant. However patients in the late stages of the disease showed a statistically significant increased hazard ratio for RRT (HR: 4.909; 95% CI: 3.10–7.776). Comorbidities like DM increased the hazard ratios for RRT (HR: 2.080; 95% CI: 1.637–2.643). Age and gender predisposed to a higher HR for RRT but they were not statistically significant. In addition dyslipidemia reduced the HR for RRT (Table 4Table 4).
Hazard ratio for needing RTT adjusted for covariables in patients with CKD.
| HR | 95 per cent CI | p | |
|---|---|---|---|
| Renal protection programme | 0.797 | 0.606–1.049 | 0.106 |
| Stages 3–4 | 4.909 | 3.100–7.776 | <0.001 |
| Age | 0.778 | 0.605–1.001 | 0.051 |
| High blood pressure | 1.545 | 0.784–3–043 | 0.209 |
| Diabetes mellitus | 2.080 | 1.637–2–643 | <0.001 |
| Dyslipidemia | 0.657 | 0.516–0.837 | 0.001 |
| Gender (males) | 0.852 | 0.672–1.080 | 0.187 |
This study shows that RPP can be a secondary prevention strategy in patients with CKD since it effectively reduces renal impairment that would result in, stage progression, development of ESRD and further need for RTT. Also it shows that the strategy of early recruitment of these patients benefit the outcomes.
The present study conducted in Latin America, had collected a very large number of patients with CKD (5663) that can be compared with reference studies like the KEEP and the NHANES III that recruited 16,689 and 2734 CKD patients respectively.9 In Latin America the reference study KEEP México recruited 3539 participants with CKD10 and the Uruguay study recruited 2219 patients.11 As a common factor for every one of these studies and our study, HBP and DM were among the most common prevalent comorbidities.
Both groups of the present were cohorts similar from the socioeconomic standpoint since each insurance company covered a labour-related population of the same region of the country, and for the purposes of our analysis both cohorts met the diagnostic criteria for CKD and showed similar proportion of comorbidities as evidenced by the results. However, it is important to note the difference in accessibility since in RPP there was an active search for diseased patients while the CT used a method of consultation on demand. The aforementioned should not be seen as different accessibility barriers to services for either one of the two populations: the RPP provided healthcare through structured protocols which was evident in the more favourable outcomes reported, and this is why we tried to show that inasmuch as healthcare providers manage to implement such programmes and conduct early patient recruitments, better outcomes can be achieved.
Patients exposed to the RPP were significantly younger than on CT; also RPP patients were in early stages of the disease; with the strategy of early recruitment of patients with CKD or at risk of developing CKD, it would be expected to have a younger population in earlier stages of the disease. Early identification and recruitment of patients is the initial step for the optimal management of a large number of diseases. Brown et al. acknowledged the importance of early recruitments of patients that are likely to develop CKD with poorly controlled risk factors, including those a reduced glomerular filtration rates, that remain unidentified as renal patients.18
Patients exposed to the RPP took a longer period of time to: progress from one stage of the disease to the next, have their first hospital admission, and need RRT. However, since in RPP the strategy was early recruitment, there were more progressors in early stages. It was expected that since patients had been recruited younger and in the early stages of the disease, the individuals exposed to the RPP would have more chances of progressing from one stage to the next while patients in late stages of the disease, either in one insurance company or the other, had little or no progression since stages 4 and 5 are considered the final stages of the disease whose outcome is usually RRT. Nonetheless, our study confirmed the potential effect of prevention to delay stage progressions.
Reduction of GFR was lower in patients exposed to the RPP since these patients had a lower GFR both at the moment of diagnosis and during the first and last change of stage. Additionally, the incidence ratio for the need for RRT was lower in RPP. Thus, CKD patients exposed to the RPP improves the clinical condition and the prognosis, since these patients have a better GFR among other significant clinical markers, also the percentage of patients needing RRT is lower.
The risk of progression to higher stages of the disease was higher in the RPP. This may be explained by the fact that with early enrolment, most patients on RPP were in CKD stages 1, 2 and 3, and therefore were more likely to progress than patients on CT. However, the risk of needing RTT was higher with CT; the lack of early recruitment contributed to have most patients in advanced stages of the disease, and with a poor access to a multidisciplinary type of healthcare, since none of this was included in CT strategy. This is why more stage progressions were expected.
The HBP and DM were found to be important risk factors for CKD stage progression, and need of RRT. However, dyslipidemia turned out to be protective which in turn matches that phenomenon of reverse epidemiology since even though dyslipidemia is widely known as a state that increases morbimortality in patients with advanced stages of CKD it has been shown to be a protective factor. Iseki et al. found that low levels of lipids were a marker of inflammation and malnutrition in renal patients.19 Also, Kilpatrick et al. said that high levels of total cholesterol, LDL, and triglycerides meant better prognosis in patients on dialysis. The serum levels of lipids, as an indirect estimate of energetic reserve, are favourable if they are in the upper limits since they may counteract both the effects of proinflammatory state and the low levels of albumin caused by poor nutritional conditions of advanced CKD.20 Jurkovitz et al. studied risk factors associated with CKD stage progression in patients from the KEEP study. Just as our study, they found that HBP, DM, and dyslipidemia were the most prevalent comorbidities of patients with CKD. This population did not have an adequate control of such cardiovascular risk factors; only patients presenting with end stages of the disease seemed to have a better control of such comorbidities, since they have more frequent access to healthcare providers such as nephrologists or other specialists. Nephrologists or other specialists did not assess patients in the early stages of the disease, and this is why risk factors were poorly controlled in these patients.21
One of the limitations of the study was the possible bias in measurements since the follow up was not identical in all patients populations; it is expected to have greater number of outcomes in group of patients with close follow up and there will be fewer records of such outcomes in the population followed for the shortest period of time.
This study shows the effectiveness of secondary prevention programmes in patients diagnosed with CKD. Results show the potential of the RPP for protection from renal impairment in this population. It is important the early enrolment of patients at risk, thus all factors and comorbidities associated are taken into account, and strategies can be designed to affect favourably the progression of the disease, reduce the number of patients who progress to more advanced stages of the disease and reduce the risk of developing ESRD and need for RTT. This is a way to achieve a better and timely care resulting in improved survival and quality of life.
Financial supportThis study has been co-financed by Colciencias, the University of Antioquia, and EPS Sura.
Conflicts of interestsWe the authors declare that while conducting this paper there were no conflicts of interests linked whatsoever.
We wish to thank Prof. Rubén Darío Gómez, PhD; Prof. Fabián Jaimes, PhD, and Prof. Hugo Grisales, PhD for their counselling.
Please cite this article as: Yepes Delgado CE, Pérez Dávila S, Montoya Jaramillo M, Orrego Orozco BE. Progreso de estadio y requerimiento de terapia de reemplazo renal en un programa de protección renal en Colombia. Estudio de cohorte. Nefrologia. 2017;37:330–337.