A 38-year-old male, native of Colombia, with a history of noncommunicating hydrocephalus at 2 years of age, secondary to episodes of viral meningitis. He required the implantation of a ventriculoperitoneal shunt, presenting mechanical and infectious complications, so 19 years later he was changed to a ventriculoatrial shunt (VA shunt).
Since then, despite the replacement, he continued with infectious symptoms, characterized by intermittent fever, skin rash and dark urine, which were exacerbated by physical activity and temperature changes; during these episodes he had deterioration of renal function, with proteinuria in the nephrotic range and macroscopic hematuria. A renal biopsy was performed in his country of origin, with the report of membranoproliferative glomerulonephritis (MPGN) type I, (report not available). With the resolution of the infection it was evidenced the recovery of renal function, up to baseline creatinine level, but the proteinuria (1–2 g/day) and microscopic hematuria (1–5/field) persisted.
Presentaba además de forma crónica, anemia, consumo del complemento por la vía clásica, y crioglobulinas positivas.
He also presented chronic anemia, complement consumption by the classical route, and a positive cryoglobulins test.
During his staying in our country, 4 years ago, he was admitted to another center for Cutibacterium acnes bacteremia. CSF cultures were sterile, so it was decided to maintain the VA shuntD. He developed acute renal failure, with Cr of 1.58 mg/dL and proteinuria of 5 g/day. Renal biopsy was performed, with the diagnosis of type I MPGN, possibly postinfectious (the material obtained was insufficient).
Regarding the current episode, he came to our center for febrile syndrome without focus, without isolations of microbiological agent, including in CSF sample (although it was extracted after starting antibiotic therapy). Lab work showed anemia (Hb 8.1 g/dL), deterioration of renal function, Cr 1.26 mg/dL, proteinuria of 5.3 g/day, microhematuria, C3 (40.2 mg/dL) and C4 (5.9 mg/dL) hypocomplementemia, elevated rheumatoid factor (410 UI/mL) and positive cryoglobulins, with cryoglobulins <1%.
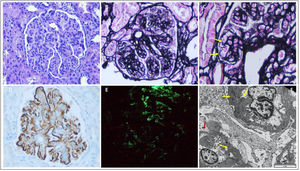
Due to worsening renal function, Cr 2.34 mg/dL and persistence of abnormalities in the urine sediment, a new renal biopsy is performed (Fig. 1). It presents a MPGN pattern, with marked endocapillary proliferation. Capillary lumens focally occupied by monocytes and polymorphonuclear cells. Tumefaction of endothelia, with fenestrations. Focal double contours. Podocytes with hypertrophic appearance and irregularly fused pedicles (30%). Direct immunofluorescence with global and diffuse positivity for IgG, C3, C1q in granular pattern in the capillary loops and occasionally in the subepithelial side. Immunohistochemical staining for intense positive C4d in granular pattern at the level of the capillary loops and mesangium. Electron microscopy showed globally enlarged mesangium at the expense of matrix and cellularity, with non-organized electron-dense deposits. These findings led to the diagnosis of glomerulonephritis associated with infection.
Renal biopsy: Glomerulus with mesangial and endocapillar proliferation and diffuse thickening of capillary loops (A and B), and the presence of double contours (C, black arrows). Immunohistochemical staining for C4d positive granular pattern in mesangial and subendothelium (D) and positivity for IgM in the pattern (E). Electron microscopy (F) shows mesangial and subendothelial electrodense deposits (black arrows) and unfolding of the glomerular basement membrane (G). A) Hematoxylin-eosin 20×, B) methenamine silver 20×, C) methenamine silver 60×, D) immunoperoxidase 20×, E) direct immunofluorescence 20× and F) electron microscopy 2000×.
Given the recurrence of fever after complying with the antibiotic regimen and the isolation of Cutibacterium acnes in CSF, it was indicated urgent withdrawal of the AV shunt, and subsequently it was evidenced the infection of the entire system. Together with Neurosurgery and Microbiology, it was decided the implantation of a ventriculoperitoneal shunt impregnated with antibiotic.
The patient continues to be followed in the outpatient clinic, with improvement of anemia (Hb 11.9 g/dL) and renal function (Cr 0.9 mg/dL), with stable proteinuria of 1 g/day in treatment with angiotensin-converting enzyme inhibitors.
DiscussionShunt nephritis is a rare immunocomplex-mediated glomerulonephritis associated with chronic infections of ventricular shunt systems.1 The incidence of shunt infection is 7.1%, and of shunt nephritis about 4.68% (compared to 0.7%–2.25% in 1970 series).1,2 More than 75% occur in connection with AV shunts.3,4
Signs and symptoms are variable and nonspecific; it has been described hematuria, fever, arterial hypertension and hepatosplenomegaly. Less frequent are skin rash and arthralgias.3
Laboratory findings include anemia, acute renal failure with proteinuria, and hypocomplementemia. The presence of cryoglobulins and positive rheumatoid factor are less frequent.3
Approximately half of CSF cultures and about one third of blood cultures are negative.1,3,5 The most frequent microorganisms involved are coagulase-negative Staphylococcus and Cutibacterium acnes.5,6
In the histology, more than half of the patients present a mesangial proliferative glomerulonephritis pattern, followed by MPGN (45%). The most frequent deposits are mesangial IgM, C1q and C3. Electron microscopy shows subendothelial (64%) and mesangial (39%) deposits.3
The combination of of antibiotic therapy and shunt removal is associated with better results.7,8 Once the infection has been resolved, it can be considered non-derivative options such as ventriculocysternostomy.9 If it is not technically possible, a ventriculoperitoneal shunt is preferred over the rest.
Shunt nephritis is a potentially fatal and reversible disease. Without timely diagnosis, progression can lead to chronic renal disease and even death.1 Therefore, early recognition should be a priority, even in the absence of microbiological isolation.
Conflict of interestNone.