Introduction: Pyelectasis can be defined as mild to moderate dilatation of the urinary tract and is diagnosed by means of an ultrasound scan (0.5-2cm transverse diameter in the initial ultrasound performed after birth). There is some disagreement about whether cystography should be indicated as standard practice. The aim of this study was to establish if renal function tests are useful in determining which cases of mild to moderate dilatation of the urinary tract do not require an initial cystography. Patients and Methods: The study was conducted on 79 infants (57 males, 22 females) with pyelectasis. Seventy-three were diagnosed in utero and 6 after birth. All infants underwent at least one cystography and one desmopressin urine concentration test before one year of age. Results: Compared to infants without vesicoureteral reflux (VUR) (n=68), infants with VUR (n=11; two with Grade I, three with Grade II, five with Grade III, two with Grade IV) showed a significantly lower (P=.006) maximum urine osmolality and a significantly higher microalbumin/creatinine ratio (P<.001) and NAG/creatinine ratio (P=.003). The negative predictive value of the first two tests was 93%. Sensitivity of the maximum urine osmolality to detect VUR was 72.7% (specificity 63.2%). Sensitivity of the microalbumin/creatinine ratio to detect VUR was 62.5% (specificity 75%). The positive probability ratio (PR) was 1.29 for the NAG/creatinine ratio, 2.03 for the maximum urine osmolality and 2.5 for the microalbumin/creatinine ratio. The negative PR was 0.95 for the NAG/creatinine ratio, 0.43 for the maximum urine osmolality and 0.5 for the microalbumin/creatinine ratio. Conclusions: Pyelectasis is a benign condition. Only 2 patients required pharmacological intervention (prophylactic treatment for VUR Grade IV patients). Initially at least, cystography should not be indicated in cases of microalbuminuria and/or normal urine concentrations.
Introducción: La ectasia piélica puede definirse como la dilatación leve-moderada de las vías urinarias diagnosticada mediante ecografía (0,5-2 cm de diámetro transversal en la primera ecografía realizada después de nacer). Existe una cierta divergencia sobre si la cistografía se debe indicar de forma universal. El objetivo del estudio fue conocer si las pruebas de función renal son útiles para decidir, en los casos de dilatación leve y moderada de las vías urinarias, aquellos en los que no se debe solicitar la cistografía inicialmente. Pacientes y métodos: Se estudiaron 79 niños (57 niños, 22 niñas) con ectasia piélica (73, diagnosticadas intraútero y seis después de nacer). A todos se les realizaron, al menos, una cistografía y una prueba de concentración con estímulo de desmopresina antes del año de edad. Resultados: En relación con los niños sin reflujo vesicoureteral (RVU) (n = 68), los niños con RVU (n = 11; dos de grado I, tres de grado II, cinco de grado III, dos de grado IV) mostraron una osmolalidad urinaria máxima significativamente inferior (p = 0,006) y un cociente microalbúmina/creatinina (p <0,001) y un cociente NAG/creatinina (p = 0,003) significativamente superiores. El valor predictivo negativo de las dos primeras pruebas fue del 93%. La sensibilidad de la osmolalidad urinaria máxima para detectar RVU fue del 72,7% (especificidad 63,2%). La sensibilidad del cociente microalbúmina/creatinina para detectar RVU fue del 62,5% (especificidad 75%). El cociente de probabilidad (CP) positivo para el cociente NAG/creatinina fue 1,29, para la osmolalidad urinaria máxima 2,03 y para el cociente microalbúmina/creatinina 2,5. El CP negativo para el cociente NAG/creatinina fue 0,95, para la osmolalidad urinaria máxima 0,43 y para el cociente microalbúmina/creatinina 0,5. Conclusiones: La ectasia piélica es una condición benigna. Sólo 2 pacientes requirieron una intervención médica de índole farmacológica (tratamiento profiláctico al ser portadores de RVU grado IV). Al menos, la cistografía no se debe indicar inicialmente en los casos de microalbuminuria y/o concentración urinaria normales.
INTRODUCTION
Dilatation of the urinary tract is diagnosed by ultrasound in 1%-5% of pregnancies.1,2 In some cases, it may be the expression of urinary tract abnormalities, such as those causing obstruction or vesicoureteral reflux (VUR).3,4 In the current literature, two terms are used for dilatation of the urinary tract, leading to some confusion: pyelectasis5,6 (from the Latin ectasis, dilatation) and the more traditional term of hydronephrosis.7,8 Some groups prefer to use the term ectasia for mild to moderate dilatation and hydronephrosis for serious cases, i.e. when the anteroposterior diameter of the renal pelvis is at least 2cm, given that most infants who need surgical treatment comply with this latter requirement.9,10 For the majority of cases, where the dilatation is not secondary to abnormalities, we have coined the term simple renal ectasia (ectasia renal simple11), and have suggested that this could indicate a genetic predisposition to suffer from kidney stones in adulthood.12
The risk of any grade of VUR is 4.4% in mild prenatal hydronephrosis and 14% in moderate.13 Some authors suggest cystography in all patients with dilatation of the urinary tract.14,15 However, given its low frequency of association with severe VUR, we believe that patients who would benefit from its diagnosis in the first months of life should initially be distinguished from those who can wait for a decision on its indication. Thereby preventing, as much as possible, an unnecessary, uncomfortable procedure and an associated risk of secondary urinary tract infection.16-19
This study shows our concept of sensitive renal function tests (maximum urine osmolality, microalbumin/creatinine ratio and NAG/creatinine ratio), which are useful for initially deciding against cystography in cases of mild and moderate dilatation.
PATIENTS AND METHODS
This is a cross-sectional prospective study of 79 breastfeeding infants (57 boys, 22 girls) diagnosed with mild and moderate pyelectasis. The diagnosis was made in utero for 73 of them, and after birth for the other six.
The foetal diagnosis was confirmed when the first ultrasound was performed after birth, with the anteroposterior diameter of the renal pelvis being between 0.5cm14 and 2cm.9,10 The same criterion was applied to infants diagnosed after birth. Patients with an anteroposterior diameter greater than 2cm were excluded. The first ultrasound was carried out at the age of 32.6±56.1 days (range: 1-240).
The ectasia was located on the left side in 32.9% of cases (n=26), and on the right side in 17.7% of cases (n=14), with 49.3% of cases (n=39) being bilateral. The mean and SD of the longitudinal diameter of the pelvis on the left side was 1.01±0.57cm and 0.75±0.64cm on the right side.
Besides the above ultrasound, the inclusion criteria were a cystography and at least one desmopressin urine concentration test within the first year of life. When the VUR was bilateral, the higher grade value was taken.
The microalbumin/creatinine ratio was measured from an isolated urine sample in 64 patients. In addition, the corresponding NAG/creatinine ratio was estimated for 53 infants from an isolated sample. Also, 26 out of the 76 patients (32.9%) were referred for a furosemide renogram during follow-up to rule out urinary tract obstruction. In all cases this was normal.
Desmopressin (DDAVP) concentration test
Every morning, 10µg of intranasal desmopressin were administered.20,21 The 3 following urine samples were then collected. If only two samples were available, the test was discontinued 8 hours later. The highest osmolality value obtained was taken as the test result. Because they were being bottle fed, the babies were restricted to half the bottle contents from the first bottle in the morning until 18.00h to reduce the risk of water intoxication.22
Laboratory techniques
Urine creatinine was measured by the creatininase method, using a Modular Analytics autoanalyser (Roche/Hitachi, Mannheim, Germany). Urine osmolality was measured by determining the freezing point depression with an Osmo Station OM-6050 osmometer (Menarini Diagnostics, Florence, Italy). Microalbumin was measured by a nephelometric technique (Array). N-acetylglucosaminidase (NAG) was determined by an enzymatic colorimetric method based on the hydrolysis of NAG-dichlorophenol sulfonephthalein (Boehringer Mannheim).
Normal values
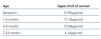
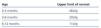
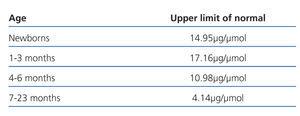
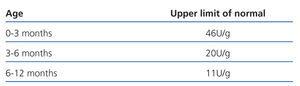
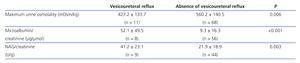
The normal values used with respect to the maximum urine osmolality,23 microalbumin/creatinine ratio24 and the NAG/creatinine25 appear in Table 1, 2 and 3, respectively.
Statistical methods
Quantitative variables were expressed as the median and interquartile ranges. Bivariate techniques were used for the initial evaluation of contrasts. Thus, Fisher's exact test was used to compare the frequencies between the qualitative variables and the Mann-Whitney U test for comparison of the means between two quantitative variables. The sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated for the three functional parameters studied to detect VUR. Furthermore, the positive and negative likelihood ratios (LRs) were calculated for the same parameters. A probability of less than 0.05 was considered statistically significant. These tests were performed using SPSS statistical software (SPSS V 17.0, SPSS Inc., USA).
RESULTS
Sixty-eight out of the 79 cystograms were normal. VUR was observed in 11 of them (13.9%): 1 of grade I, 3 of grade II, 5 of grade III and 2 of grade IV. The longitudinal diameters of the pelvis for the two patients with the highest VUR grade were 1.2cm and 1.34cm, respectively, and both received prophylactic treatment. The VUR was found on the left side in 4 infants, 2 had it on the right side and in 5 it was bilateral.
There was a renal concentrating capacity defect in 33/79 cases (41.7%). Urinary excretion of microalbumin was high in 19/64 cases (29.7%) and the NAG/creatinine ratio was high in 10/53 (18.8%).
Patients were distributed according to the presence or absence of VUR, the values of the three functional parameters were significantly different in both groups (Table 4).
The maximum urine osmolality of the 3 infants with VUR and the normal concentration test was 529mOsm/kg (grade I), 599mOsm/kg (grade II) and 665mOsm/kg (grade III). The two infants with VUR grade IV had both a concentrating capacity defect and increased urinary excretion of microalbumin (254mOsm/kg, microalbumin/creatinine 21.9µg/mol and 382mOsm/kg, microalbumin/creatinine 8.7µg/mol, respectively).
No differences were found in renal function after dividing the sample into two subgroups according to the longitudinal diameter of the pelvis (greater and smaller than 1cm).
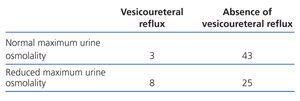
Table 5 shows the comparison of the frequencies between the absence and presence of VUR in the urine concentration test. 36.7% of infants with simple renal ectasia (without VUR) had a concentrating capacity defect.
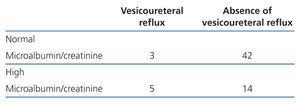
Table 6 shows the comparison of the frequencies between the absence and presence of VUR in the urinary excretion of microalbumin. 25% of infants with simple renal ectasia had increased urinary excretion of microalbumin.
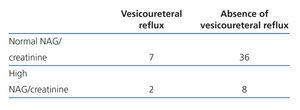
Table 7 shows the comparison of the frequencies between the absence and presence of VUR in the urinary excretion of NAG. 18.2% of infants with simple renal ectasia had increased urinary excretion of NAG.
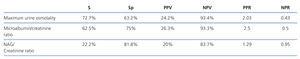
Table 8 shows values for sensitivity, specificity, positive and negative predictive values and positive and negative likelihood ratios for the three functional parameters studied to detect VUR.
DISCUSSION
Most pyelectasis study protocols recommend an initial cystography14,15,26 or renogram27 in addition to an ultrasound scan. It is surprising that none of the existing protocols mention a renal function study, including those recommended by paediatric nephrologists.
In the initial protocol used in our hospital, we performed both a morphological (ultrasound) and renal function study.28 This study is therefore an attempt to confirm that renal function should be examined when selecting which infants diagnosed with mild-moderate urinary tract dilatation should undergo a cystography. In the initial functional study, we did not include parameters for measuring glomerular renal function such as creatinine or cystatin C levels. They are very specific for kidney damage but not sensitive, as renal parenchymal damage is already considerable when changes are detected.
Continuously high microalbumin is an early sign of glomerular damage in hyperfiltration processes, such as diabetic nephropathy. It is also a suitable marker for hyperfiltration in the healthy renal parenchyma, as it increases in cases with a significant absence of the rest of the parenchyma. In addition, microalbuminuria is recognised as a marker of endothelial damage, as occurs in hypertension, for example.29-31 One interesting but not well accepted issue is whether it can also increase in response to situations where there is excess pressure in the urinary tract, as in cases of VUR.32,33 Our results seem to confirm this third utility for determining microalbuminuria. Moreover, we confirmed that once VUR is cured, urinary excretion of microalbumin is reduced, compared to initial values.34
NAG is a characteristic enzyme of the renal proximal tubule cells that travels through the tubular lumen, and therefore into urine, in high quantities when there is a cellular aggression. Its levels may be elevated in cases of urinary tract obstruction and in VUR, especially when there is scarring from nephropathy.32,35
The renal concentration test is based on the maximum urine osmolality reached by the effect of arginine-vasopressin in the renal collecting tubules, stimulating the activity of aquaporins. When any of the various components of this mechanism is disturbed, there is a defect in the concentrating capacity, which is accompanied by polyuria. However, minor defects may go unnoticed.
Many kidney disorders that occur with normal glomerular filtration rate, especially many tubulopathies, obstructive uropathies36-38 and VUR,34,39-41 are related to a reduced maximum urine osmolality and, therefore, to a concentrating capacity defect.
Table 3 shows how infants with VUR, compared to those with simple renal ectasia, showed significantly reduced maximum urine osmolality values and significantly high NAG/creatinine and microalbumin/creatinine ratios. This is due to functional damage produced by overpressure on the urinary tract to renal parenchyma.
In our results, the NAG/creatinine ratio can be seen as the least sensitive, but most specific of the three parameters studied, similar to that mentioned for the plasma creatinine levels.27 Conversely, the maximum urine osmolality is the most sensitive parameter for detecting VUR (72.7%), but the least specific. The microalbumin/creatinine ratio had a sensitivity and specificity between the above two parameters. The three parameters studied performed very well in calculating the likelihood ratios (LR). They summarise information on the sensitivity and specificity and indicate the test's ability to increase or decrease the likelihood of a particular diagnosis. The higher the LR is above 1, the more likely the diagnosis is to be correct. Thus, the LR for each of these parameters is on the rise, 1.29 for the NAG/creatinine ratio, 2.03 for the maximum urine osmolality and 2.5 for the microalbumin/creatinine ratio.
The reported results show the validity of functional tests when considering a cystography. At least two of the functional tests are useful in deciding who should not undergo this procedure. It seems that no functional parameter has a 100% guarantee for the absence of VUR. However, our results suggest that if the patient has a normal concentrating capacity and/or the microalbumin/creatinine ratio is not high, there is a high probability (93%) that it is a simple pyelectasis. Only 3 infants with VUR had a normal renal concentrating capacity and, according to current criteria, their degree of VUR did not require antibiotic prophylaxis42,43 or surgery. In addition, only 1 out of the 3 infants with VUR and a normal microalbumin/creatinine ratio was a grade IV patient, and he or she would have been diagnosed due to clearly impaired urinary concentrating capacity.
Furthermore, our study has detected a hitherto unrecognised fact. Some infants with simple renal ectasia had a defect in renal concentrating capacity and/or increased microalbuminuria. Thus, 25% of infants showed a slight increase in urinary excretion of microalbumin and 36.7% had a slight defect in the concentrating capacity. This finding was unknown as it is a minor defect. Nevertheless, in a longitudinal study, our group has demonstrated that both functional defects progressively normalise with age.44
To summarise, because there is a high probability of a mild abnormality, we believe that in cases of urinary tract dilatation, morphological (ultrasound) and functional studies need not always be performed immediately after birth. In particular, when the longitudinal diameter of the renal pelvis is less than 1cm, it could even be done between the third and sixth month of life, as there is a very low risk of detecting severe reflux. A cystography can then be requested, depending on the function test results. We believe that it is acceptable to request this initial radiological test only if both parameters, maximum osmolality and microalbumin, are abnormal. This initial recommendation may be reversed if the pyelic diameter gradually increases, or if children have acute pyelonephritis or if subsequent renal function tests are abnormal, and they would be re-assessed for new morphological studies (cystography and/or furosemide renogram).
In short, we believe that the most important issue is to adequately monitor these infants so that no potentially serious clinical condition goes unnoticed, while ensuring a medical approach leading to less discomfort and lower side effects at all times.
Table 1. Normal values of the maximum urine osmolality in the first year of life obtained after desmopressin stimulation (Reference 23)
Table 2. Normal values of the microalbumin/creatinine ratio in the first year of life (Reference 24)
Table 3. Normal values of the NAG/creatinine ratio in the first year of life (Reference 25)
Table 4. Values of maximum urine osmolality, microalbumin/creatinine ratio and NAG/creatinine ratio after separating the sample between those with and without vesicoureteral reflux
Table 5. Comparison between the results for the concentration test and cystography (Fisher¿ exact test P=.02)
Table 6. Comparison between the results for urinary microalbumin excretion and cystography (Fisher¿ exact test P=.001)
Table 7. Comparison between the urinary NAG excretion results and cystography (Fisher¿ exact test P=.32)
Table 8. Results for the quality and diagnostic efficiency indices of the three parameters studied to detect VUR