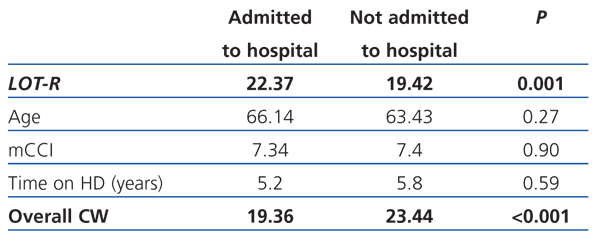
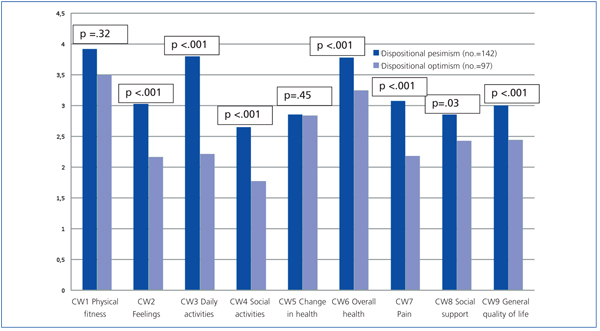
Introduction: Dispositional optimism is a personality trait significantly associated with the use of positive adaptive coping strategies as well as with perceived psychological and physical well-being, and it appears to be an important predictor of illness. Objectives: To analyse if dispositional optimism is significantly associated with the number of hospital admissions of our chronic haemodialysis patients, as well as its relationship with perceived state of health. Methods: We studied 239 patients on chronic haemodialysis. Patients were categorised into two groups according to the variables: hospital admissions/no. of admissions in the last year and dispositional optimism (DO). We used the following variables and questionnaires: 1) Dispositional O/P using the Spanish-validated cross-cultural adaptation of the revised version of the Life Orientation Test (LOT-R) (Scheier, 1994): higher scores mean a higher degree of dispositional optimism. 2) Health-related quality of life (HRQoL) using the different aspects of the COOP/WONCA (CW) charts and its total score. In this case higher scores mean lower HRQoL. 3) Modified Charlson Comorbidity Index (mCCI). 4) Age, gender, and time on dialysis. Results: Mean age was 64.8±14.3 years; median time on dialysis 2.9 years (range: 0-32); and median LOT-R 21 (range 6-30). Patients considered DO had a lower risk of hospital admissions than pessimists (DP) (OR: 0.55; IC 95%: 0.32-0.94; P<.05). PD Patients that were admitted in the last year showed a significantly lower score on LOT-R (they were more pessimistic) than those that had no hospital admissions (19.4±5.7 vs 22.3±4.6; P=.001). We found no significant differences between admitted and not admitted patients in age, gender, time on haemodialysis and comorbidity. Admitted patients showed worse HRQoL (higher scores in total CW) than those that were not (Total CW: 22.37 vs 19.42; P<.001). PD patients had significantly higher scores than OD patients in all COOP-WONCA aspects except in aspect 1 (physical fitness) and 5 (change in health). Conclusions: Pessimistic personality trait is significantly associated with hospital admissions in chronic haemodialysis patients, regardless of age, gender and comorbidity. Optimistic patients perceived a better state of health.
Introducción: El optimismo disposicional es un rasgo de personalidad que se relaciona significativamente con el empleo de estrategias positivas de afrontamiento y con el grado de bienestar psicológico y físico percibidos por el paciente, y que parece ser, también, un importante predictor de enfermedad. Objetivo: Analizar si el optimismo disposicional guarda relación con el número de ingresos hospitalarios que han presentado en el último año los enfermos renales crónicos estadio Vd en nuestros centros. Material y métodos: Se estudiaron 239 pacientes en hemodiálisis que fueron categorizados en dos grupos respecto a las variables ingresos /no ingresos hospitalarios en el último año y optimismo/pesimismo disposicional. Se utilizaron los siguientes cuestionarios y variables: 1) O/P disposicional mediante el LOT-R de Scheier (1994) en su versión española: a mayor puntuación, mayor grado de optimismo disposicional. 2) Calidad de vida relacionada con la salud (CVRS) mediante las láminas COOP/WONCA: a mayor puntuación peor calidad de vida referida. 3) Índice de comorbilidad de Charlson (ICM). 4) Edad, tiempo en HD y sexo. Resultados: La edad media fue de 64,8 ± 14,3 años; la mediana de tiempo en hemodiálisis de 2,9 años (rango: 0-32), y la mediana en el LOT-R 21 (rango: 6-30). Los pacientes optimistas (OD) presentaban un menor riesgo de ser ingresados que los pesimistas (PD) (OR: 0,55; IC 95%: 0,32-0,94; p <0,05) y los pacientes con ingresos hospitalarios mostraron una puntuación en el LOT-R significativamente menor que los que no ingresaron (19,4 ± 5,7 frente a 22,3 ± 4,6; p = 0,001). No se encontraron diferencias significativas en cuanto a edad, tiempo en hemodiálisis, e índice de comorbilidad de Charlson entre los pacientes que ingresaron y los que no ingresaron. Los pacientes que ingresaron mostraban peor calidad de vida relacionada con la salud que los pacientes que no ingresaron (CW total: 22,37 frente a 19,42; p <0,001). Los pacientes PD puntuaban significativamente más alto que los pacientes OD en las láminas COOP/WONCA en todas las dimensiones exploradas, excepto en las dimensiones 1 (estado físico) y 5 (cambios en el estado de salud). Conclusiones: El rasgo de personalidad pesimista se asocia con los ingresos hospitalarios independientemente de la edad, el tiempo en diálisis y el grado de comorbilidad del paciente. Por otra parte los pacientes con un rasgo de personalidad optimista tienen una mejor salud percibida.
INTRODUCTION
Several studies have highlighted that certain personality traits are related with the prognosis of a disease, and it seems that some of them might be predictors of illness.1 Dispositional optimism, one of the traits that is capturing the most interest, refers to general positive expectations. This trait was initially proposed and investigated by Scheier et al in their articles in 1986 and 1992. Dispositional optimism is one of the personal resources to protect well-being and is assessed using the Life Orientation Test (LOT-R).2 There is a Spanish-validated cross-cultural adaptation of this test available. This trait consists in having a general positive outlook and expecting positive results; in other words, the tendency to expect positive outcomes in the future. People with dispositional optimism are less likely to attribute negative events to internal factors (“it is my fault”), stability factors (“I’m this way, it is how I am, and I can’t change”), and global factors. They are, therefore, more likely to see stress as a problem that can be changed, that is specific to that moment and that essentially comes from external sources that can be potentially modified or ignored.
This personality trait has been identified in several studies as a good predictor of prognosis or recovery in cardiac3-5 and cancer6-8 patients. It appears to be related with the use of positive strategies for coping with stress, i.e., more adaptive coping strategies. Patients with this optimistic personality trait tackle stressful situations and adapt to disease and, as a result, consequent treatments better.
Advanced kidney failure requiring kidney replacement therapy affects the patient’s physical and emotional health. Subjects have to make some important changes to their lifestyle when starting haemodialysis (HD) and this has an effect on their quality of life and probably on their later progress on dialysis. The ability of the subject to control their own behaviour by using adaptive coping strategies is essential during the whole process of adapting to dialysis. This model of “behavioural self-control” assumes that when difficulties arise, positive expectations increase people’s efforts to be able to meet their objectives, while negative expectations reduce these efforts, sometimes to the point of completely giving up on the task. In this model, optimism and pessimism would be considered as general expectations (favourable or unfavourable, respectively) on events that happen to you during your life. Furthermore, these expectations are considered as stable dispositions (i.e. individual personality traits). That is why it is called “dispositional optimism”.9
“Positive thinking” or “optimism” seem to play an important role in the use of these adaptive coping strategies,10,11 as well as on psychological and physical well-being.12 They also seem to be significant predictors for psychological and physical diseases.13,14
The main aim of this study was to analyse the association between dispositional optimistic personality traits and the number of hospital admissions in one year in our HD population on kidney replacement therapy. The relationship between dispositional optimism and health-related quality of life (HRQoL) was also studied.
MATERIAL AND METHOD
Patients
This was a cross-sectional, observational and retrospective study on 239 HD patients on kidney replacement therapy belonging to three hospitals.
Inclusion and exclusion criteria
Of a total of 249 patients on HD in our units, 239 accepted to participate after being informed on the nature and objectives of the study and were included in the study. The exclusion criteria were: patients that had been previously diagnosed with a psychotic or neurological disorder or mental retardation; patients that could not answer the questionnaire due to difficulties with comprehension; and those whose state of health had deteriorated leading to hospital admission or had had a stressful event 30 days before the study (death of a family member/friend, personal illness, their own accident or of someone close to them, change in financial situation, change of job/house, divorce/separated, marriage, loss of job). Of the 10 patients excluded from the study, three were foreigners and did not speak Spanish; therefore, they were not able to answer the test properly. The other seven had been admitted to hospital recently.
Data collection procedure
All the patients were informed on the nature and objectives of the study and signed an informed consent form. The Life Orientation Test-Revised (LOT-R) as well as the health-related quality of life charts (COOP-WONCA) were filled in during the HD sessions as the patient was in a stable clinical situation. Both tests were administered by trained nephrologists from the units. The other variables were collected from patients’ medical history. These data were collected cross-sectionally over a period of one month.
The number of hospital admissions was recorded for each patient during the following year.
Measuring instruments
Dispositional optimism: life orientation test-revised
The dispositional optimism variable was obtained using Scheier’s revised version of the life orientation test (LOT-R)2 published in 1994 in the form of Otero-López’s Spanish version (1998).15 This questionnaire is made up of 10 items, 4 of which are filler questions (items 2, 5, 6, 8), i.e. they make the content of the test less obvious and they are not to be used in the analysis. The 6 remaining items measure the level of dispositional optimism: three are positively worded (optimistic direction) and three are negatively worded (pessimistic direction). The subjects are asked to state their level of agreement or disagreement with statements such as “in uncertain times, I usually expect the best” using a 5-point scale where 1 is “disagree a lot” and 5 “agree a lot”. Of the 6 content items, the negatively worded items are inverted and a total score focussed on optimism is obtained. The adaptation of the LOT-R used in this study is included in Table 1. This test measures stable personality traits and the general predisposition of the individual towards positive or negative results for the future. The higher the score obtained in the LOT-R, the higher the level of dispositional optimism is and vice-versa. As there are no standard scores for the questionnaire, we decided to use the median as a cut-off point to differentiate between dispositional optimism and pessimism. The patients that had a score equal to or lower than the median of the distribution were classified as dispositional pessimists (DP) and those with a score above the median as dispositional optimists (DO).
Health-related quality of life (HRQoL): COOP-WONCA (CW) charts
The HRQoL was estimated using the Spanish version of the COOP-WONCA charts (CW)16,17(Figure 1). These charts were chosen instead of other questionnaires such as the NHP (Nottingham Health Profile), SIP (Sickness Impact Profile), Kidney Disease Quality of Life (KDQOLTM) or SF-36 based on the fact that they are all similarly valid,18 but these are easier to answer and have been used previously on dialysis patients.18-20
The COOP-WONCA charts are short, easy to understand and have good criteria for measuring quality. When compared with the SF-36 (widely used in the dialysis population), they show a convergent validity of 0.57, a discriminant validity of 0.22 and Cronbach’s alpha of 0.76.18
There are nine charts and each one explores an aspect of the patient’s quality of life completely. Each aspect has a title and answers the question relating to what has happened in the last two weeks: 1) Physical fitness, 2) Feelings. 3) Daily activities. 4) Social activities. 5) Change in health. 6) Overall health. 7) Pain. 8) Social support. 9) General quality of life. The patients have five possible answers that are accompanied by a drawing or a sign for each answer. The possible answers follow an ordinal scale from 1 to 5, and a higher score means a worse HRQoL. Although it has not been used much in the literature as it does not provide much information if individual scores for each chart are not shown in the results, the possibility of using an index has been accepted (overall COOP-WONCA). This is the total of all the charts, except for number 5 (Change in health), which is read in a different way due to the fact that it has a bipolar structure.
Comorbidity: Charlson’s comorbidity index
Comorbidity was obtained using Charlson’s original comorbidity index21 modified in accordance with the proposal of Beddhu et al.22 It included the patient’s age as another item, the score increasing by one point for every 10 years over the age of 40.
Variables analysed
The results obtained in the LOT-R were analysed in accordance with the following variables:
1. Age
2. Sex
3. Average time on HD
4. Charlson’s comorbidity index (CCI)
5. HRQoL according to the COOP-WONCA charts
6. Hospital admissions per patient in the last year
Statistical analysis
The statistical analysis was carried out using SPSS 12.1 software. Student’s t-test was used to compare independent samples when the data followed a normal distribution and Wilcoxon test when the samples did not follow it. The chi-square test was used to compare qualitative variables and the strength of association was measured by calculating the odds ratio and the 95% confidence interval. The strength of association between the results obtained using the LOT-R and the HRQoL questionnaire (COOP-WONCA) was evaluated using Pearson’s linear correlation coefficient. The results were taken to be statistically significant at P<.05.
RESULTS
Mean age was 64.8±14.3 years and 62.5% of patients were men. The distribution of men and women was similar in both groups of patients (63% men and 37% women vs 60% men and 40% women; P=.45). The median time on HD was 2.9 years (range: 0-32), the mean score on the LOT-R was 21.1±5.3 and the median 21 (range: 6-30).
Of a total of 239 HD patients studied, 65 had been admitted during the previous year. There were no significant differences between the patients considered DP (score equal to/lower than the median of the distribution) and DO (score higher than the median of the distribution) for age (64.1±16.1 compared to 61.1±17.0; P=.42), time on HD (15.3±32.1 compared to 15.5±30.3; P=.97) and comorbidity according to the CCI (6.76±2.4 compared to 7.33±2.88; P=.32). The patients considered DO had a lower risk of being admitted to hospital than pessimists (OR: 0.5; 95% CI, 0.3-0.9; P<.05). The patients admitted to hospital showed a significantly lower score on the LOT-R (pessimist) than those not admitted to hospital (19.4±5.7 compared to 22.3±4.6; P=.001). There were no significant differences with regard to age, time on haemodialysis and CCI between patients admitted and those not admitted to hospital (Table 2).
Patients admitted to hospital had a worse HRQoL (higher scores in the total CW) than patients not admitted (total CW: 22.37 compared to 19.42; P<.001) (Table 2).
Figure 2 shows how the patients considered DP, according to the LOT-R score, had a significantly higher score than DO patients on the COOP-WONCA charts in all the aspects studied, except for aspect 1 (physical fitness) and 5 (change in health). Therefore, “pessimistic” patients perceived their health state to be worse. There was a -0.47 correlation (P<.001) between the LOT-R scores and the HRQoL scores (overall COOP-WONCA).
DISCUSSION
This study evaluated dispositional optimism (DO) in HD patients. This is a personality trait that is currently being studied extensively in other areas of medicine. However, its influence on patients with kidney diseases is still unknown. Our results highlight that HD patients with a pessimistic personality trait have a higher risk of being admitted to hospital than optimistic patients. Furthermore, these admissions do not depend on age, sex, time on HD, or associated pathology. Authors such as Hudetz,23 King and Karensen, among others, have identified DO as a good predictor of prognosis and recovery in patients undergoing cardiovascular surgery as well as cardiac and cancer patients. It has been suggested that this relationship between DO and a more favourable course of the disease lies in the patients’ better ability to cope with the problems. Optimism is strongly linked to self-efficacy (the belief that one is capable of doing what is required in a given situation). There are several studies that associate certain personality traits with different coping strategies for stressful situations. According to the data published by Carver24 in 2001, people with an optimistic personality trait have an active or more adaptive style for coping with stress (planning, positive reinterpretation, personal growth and problem solving) compared with pessimists, who have a passive style (refusal, focus on emotions and behavioural distancing). The fact that DPs have this type of coping strategy means that they avoid solving problems and the problems continue. The studies carried out by Chico in 20029 and Roy in 201025 follow this line of thought as they state that, as well as the ability to cope with stress, another mechanism linking dispositional pessimism with physical symptoms may be that these patients persist with harmful habits to their health.
All dimensions of a patient’ life change significantly during kidney replacement therapy and it is essential that patients prepare themselves correctly to achieve a good response to therapy. We see everyday how patients that adapt better to the treatment are able to follow strict diets low in potassium and phosphates; maintain a perfect weight between dialysis; comply better with drug treatments; come to recommended check-ups, etc. In summary, their behaviour seems to yield better results. One of the limitations of our study was that it was a short, cross-sectional study and it is not possible to assess the relation between DO/DP and morbidity/mortality in the long term. This item could be the objective of another study.
In this study we have observed how patients with an optimistic personality trait had a better HRQoL. This result was global (total CW) and for every aspect of the COOP-WONCA charts (feelings, daily activities, social activities, health, pain, social support and quality of life) except in two: physical fitness and change in health. This finding seems to indicate that the level of DO is related to a greater extent with the more psychological and social dimensions of perceived health and not so much with the physical aspect (physical fitness) and with the observation of changes in health. The studies by Chang26 and Martínez-Correa1 show an association between DO/DP and state of physical health. Optimistic subjects had a lower number of immunological, gastrointestinal, cardiovascular, neurosensory, genitourinary and dermatological symptoms compared with pessimists during the last year assessed. No differences were found in respiratory and musculo-skeletal symptoms.
To conclude, DO is another factor to be taken into account in the evolution of dialysis patients. In fact, pessimism seems to be associated with a higher number of hospital admissions, regardless of age, time on dialysis and comorbidity of the patient. Furthermore, patients with an optimistic personality trait perceive that they have a better HRQoL.
Table 2. Relation of the different variables analysed with hospital admission
Figure 2. Health and optimism-related quality of life
10534_108_14687_en_10534es_tabla_1.doc
Table 1. LOT-Revised (cross-cultural adaptation)
10534_108_14689_en_10534es_figura_1.doc
Figure 1. COOP-WONCA charts (Spanish) for measuring quality of life