Asymptomatic hyperuricaemia is common in kidney transplant recipients and traditional treatment with allopurinol or benzbromarone is associated with complications and interactions that could be potentially serious, and they have demonstrated lower efficacy if used in normal doses. In this study, we aim to assess the short-term efficacy and safety of treatment with febuxostat in stable kidney transplant recipients.
Fifteen kidney transplant recipients being treated with febuxostat who had completed a minimum of 6 months of treatment were enrolled. Uric acid levels, renal function and proteinuria, as well as levels of immunosuppressants at baseline, after three months and after six months were analysed retrospectively. The presence of adverse effects or lab test abnormalities requiring the suspension of the drug were also assessed.
All patients were clinically stable, with creatinine levels of 1.81±0.57mg/dl. All had previously received treatment with allopurinol except one, due to a history of bone marrow failure caused by this drug. Both the starting dose and changes to it were determined by the clinic at its own discretion: the most common was 40mg/day (Table 1).
Demographic characteristics of the subjects included in the study.
| Variable | |
|---|---|
| Number of subjects, n | 15 |
| Age (years) | 55.6±15.31 |
| Males, n (%) | 14 (93.3) |
| Time from TX to start of FBX (months) | 5; mean: 67.13±70.31; median: 36.4; range: (7.1–242.7) |
| Treatment with TAC, n (%) | 11 (73.3) |
| Treatment with CsA, n (%) | 2 (13.3) |
| Treatment with EVER, n (%) | 1 (6.6) |
| Starting dose FBX 40mg/day, n (%) | 12 (80) |
| Final dose FBX < or =40mg/day, n (%) | 12 (80) |
| Previous treatment with allopurinol, n (%) | 14 (93.3) |
CsA: cyclosporin A; EVER: everolimus; FBX: febuxostat; TAC: tacrolimus; TX: kidney transplant.
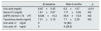
Levels of uric acid decreased significantly after six months of treatment with febuxostat (from 8.45±0.45 to. 6.20±1.07mg/dl). No patient presented gout. No significant differences were found in renal function or in proteinuria levels. We did not detect a homogeneous change in dosage of immunosuppressive drugs. Despite the variations in the dose of febuxostat, there were no significant differences in the serum levels of calcineurin inhibitors or m-TOR inhibitors. No serious adverse events were reported. Overall and graft survival was 100% (Table 2).
Levels of uric acid and other parameters at baseline and six months after starting treatment with febuxostat.
| At baseline | After 6 months | p | |
|---|---|---|---|
| Uric acid (mg/dl) | 8.45±0.45 | 6.2±1.07 | <0.01 |
| Serum Cr (mg/dl) | 1.81±0.57 | 1.71±0.55 | NS |
| eGFR (ml/min/1.73m2) | 53.86±15.3 | 56.9±15.8 | NS |
| Tacrolimus levels (ng/ml) | 7.01±2.18 | 7.7±2.39 | NS |
| Uric acid <7mg/dl | 0 | 12 (80) | |
| Uric acid <6mg/dl | 0 | 4 (26.6) |
Cr: creatinine; eGFR: estimated glomerular filtration rate.
Hyperuricaemia is common in kidney transplant recipients, mainly in those treated with calcineurin inhibitors (cyclosporin and tacrolimus) or diuretics.1 Now, several studies show that this disorder causes graft dysfunction through the activation of proinflammatory mediators, which eventually elicit endothelial and renal microvasculature damage.2,3
Very few studies have shown that reducing uric acid levels has real benefits in the progression of chronic kidney disease.4 In 2010, Goicoechea led a randomised controlled study and, later, in 2015, he published his post hoc analysis, in which he stated that the beneficial effect of treatment with allopurinol in the progression of kidney disease and cardiovascular risk was maintained after an average of seven years of follow-up.5,6
In kidney transplant recipients, several studies show that hyperuricaemia plays a relevant role in the long-term prognosis and graft survival.7 However, there are no randomised clinical trials showing a real benefit in reducing uric acid in these patients.
Febuxostat, a new selective xanthine oxidase inhibitor, offers an alternative for those subjects for whom uric acid targets are not achieved, or who have an intolerance or a contraindication for the use of the traditional drugs.
To date, there are insufficient studies to guarantee the efficacy and safety of this drug in stable kidney transplant recipients. In 2014, two retrospective studies were published that analysed kidney transplant recipients in treatment with febuxostat at low doses (between 10 and 20mg/day). In both, after an average follow-up of 12 months, a significant reduction in uric acid was seen, with no serious adverse events occurring.8,9 The patients in treatment with febuxostat achieved bigger reductions than those who received allopurinol or benzbromarone, with no significant differences in the glomerular filtrate rate.9
In our study, febuxostat is shown to be an effective drug which achieves a significant reduction in uric acid within the first six months, even with doses lower than those recommended by the company, in patients for whom the desired targets were not achieved previously with allopurinol. It has also been shown to be a safe drug, with no serious adverse event being recorded and no apparent impact on renal function, proteinuria or levels of immunosuppressants.
It is worth highlighting the almost complete lack of serious adverse events with low doses of the drug. In a multicentre clinical trial comparing febuxostat (doses of 80 and 120mg/day) with allopurinol (dose of 300mg/day), the number of patients who stopped taking the drug was significantly higher in the group which received 120mg/day of febuxostat, particularly due to adverse events and gout.10
Our study has certain limitations. It is an observational, retrospective, single-centre study with a small patient sample. However, the results are in line with those obtained by recent studies with a similar design, which is encouraging for the continued progress towards an effective hyperuricaemia treatment in kidney transplant recipients.
In conclusion, Febuxostat seems to offer short-term efficacy and safety for stable kidney transplant recipients who are resistant to treatment with allopurinol. Prospective, randomised studies demonstrating not just its long-term efficacy and safety but also the effects of reducing uric acid on graft survival and cardiovascular events in these patients are required.
Please cite this article as: Ferreira M, Jiménez C, Lopez MO, González E, Santana MJ, Selgas R. Eficacia y seguridad a corto plazo del tratamiento con febuxostat en el paciente trasplantado renal. Estudio observacional unicéntrico. Nefrologia. 2018;38:331–332.