Introduction: The high prevalence of chronic kidney disease (CKD) in the general population has created a need to coordinate specialised nephrology care and primary care. Although several systems have been developed to coordinate this process, published results are scarce and contradictory. Objective: To present the results of the application of a coordinated programme between nephrology care and primary care through consultations and a system of shared clinical information to facilitate communication and improve the criteria for referring patients. Methods: Elaboration of a coordinated care programme by the primary care management team and the nephrology department, based on the SEN-SEMFYC consensus document and a protocol for the study and management of arterial hypertension (AHT). Explanation and implementation in primary health care units. A directory of specialists’ consultations was created, both in-person and via e-mail. A continuous training programme in kidney disease and arterial hypertension was implemented in the in-person consultation sessions. The programme was progressively implemented over a three-year period (2007-2010) in an area of 426,000 inhabitants with 230 general practitioners. Use of a clinical information system named “Salut en Xarxa” that allows access to clinical reports, diagnoses, prescriptions, test results and clinical progression. Results: Improved referral criteria between primary care and specialised nephrology service. Improved prioritisation of visits. Progressive increase in referrals denied by specialists (28.5% in 2009), accompanied by an explanatory report including suggestions for patient management. Decrease in first nephrology outpatient visits that have been referred from primary care (15% in 2009). Family doctors were generally satisfied with the improvement in communication and the continuous training programme. The main causes for denying referral requests were: patients >70 years with stage 3 CKD (44.15%); patients <70 years with stage 3a CKD (19.15%); albumin/creatinine ratio <500 mg/g (12.23%); non-secondary, non-refractory, essential AHT (11.17%). The general practitioners included in the programme showed great interest and no complaints were registered. Conclusions: The consultations improve adequacy and prioritisation of nephrology visits, allow for better communication between different levels of the health system, and offer systematic training for general practitioners to improve the management of nephrology patients. This process allows for referring nephrology patients with the most complex profiles to nephrology outpatient clinics.
Introducción: La elevada prevalencia de la enfermedad renal crónica (ERC) en la población general ha creado la necesidad de desarrollar una coordinación entre la atención especializada nefrológica y la atención primaria. Aunque diversos sistemas se han desarrollado para coordinar este proceso, la presentación de resultados es escasa y a veces contradictoria. Objetivo: Presentar los resultados de un programa de coordinación entre atención primaria y atención especializada nefrológica mediante consultorías y un sistema de información clínica compartida para facilitar la comunicación y mejorar los criterios de derivación de los pacientes. Métodos: Elaboración de un programa consensuado entre la dirección médica de atención primaria y nefrología basado en los criterios del «Documento de consenso entre la S.E.N. y la semFYC» y en un protocolo de estudio y tratamiento de la hipertensión arterial (HTA). Explicación e implantación en los equipos de atención primaria. Creación de un programa de agendas de consultorías en atención primaria tanto presenciales como vía correo electrónico de nefrólogos. Implantación de un programa de formación continuada en enfermedades renales y en HTA durante las consultorias presenciales. Progresivo desarrollo en un período de 3 años (2007-2010) en un área de 426.000 habitantes con 230 médicos de familia. Utilización de un sistema de información clínica compartida llamado «Salut en Xarxa» que permite el acceso a informes clínicos, diagnósticos, prescripciones, analíticas y curso clínico. Resultados: Mejora en los criterios de derivación entre atención primaria y nefrología. Mejoría en la priorización de las visitas. Progresivo incremento en el retorno de solicitudes de visitas a nefrología (28,5% en 2009), acompañados de un informe explicativo que incluye sugerencias sobre el tratamiento del paciente de la solicitud devuelta. Disminución de las primeras visitas procedentes de atención primaria en consultas externa de nefrología (15% en 2009). Satisfacción general de los médicos de familia por la mejora en la comunicación y en el programa de formación continuada. Las principales causas de retorno de solicitudes de visita fueron: enfermedad renal crónica (ERC) 3 en >70 años en el 44,15%, ERC 3 a en <70 años en el 19,15%, albuminuria <500 mg/g de creatinina en el 12,23%, HTA esencial no resistente ni secundaria en el 11,17%. En la aplicación de este programa hubo un gran interés de los médicos de familia y no se registraron situaciones conflictivas. Conclusiones: El desarrollo de las consultorías mejora la adecuación y la priorización de las visitas a nefrología, permite mejorar la comunicación entre los niveles de los sistemas de salud y ofrece un sistema de formación continuada para mejorar el tratamiento de los pacientes nefrológicos. Este proceso conduce a una selección de los pacientes con un incremento de la complejidad de las visitas en las consultas externas de los servicios de nefrología.
INTRODUCTION
The success of the proposed classification system of kidney diseases into five different stages1 and the use of glomerular filtration rate estimated by formulas2 has led the way for epidemiological studies that have demonstrated a high prevalence of chronic kidney disease (CKD). Systematic reviews on the prevalence of this disease have observed rates of 7.2% in people older than 30 years3; in the USA, this rate is 13.1% in the general population,4 and it is 9.09% in the general population in Spain (EPIRCE study5). Elderly patients deserve special attention, as this is the age range of people that most frequently access the health care system. According to systematic reviews in patients 64 years old or older, CKD (especially 3 CKD3) has yielded a prevalence of 23.4%-35.8%, depending on the method used for estimating glomerular filtration. Another medical condition frequently observed in patients referred to nephrology units is arterial hypertension (AHT). The prevalence of AHT is also extraordinarily high, especially in patients older than 60 years, reaching 56.4%.6
An elevated prevalence of CKD and AHT necessitates coordination with the primary care services of the public health system in order to provide the required response to this health care issue. The Spanish Society of Nephrology (S.E.N.) has supported this coordination and created awareness.7 Several collaborative protocols between primary health care and nephrology centres have produced a significant increase in nephrology visits and in the number of patients older than 80 years that are referred to a nephrologist.8
Through shared clinical history systems, the unstoppable progress of information and communication technologies can allow primary and specialised health care professionals to have access to the same information regarding the patients they treat. In addition, these systems can facilitate rapid and personalised communication through e-mail and videoconferences.
Within the reference patient population at our hospital, we have observed an increase in the number of patients being referred from primary care to the nephrology units since 2005, and many of these cases did not really need specialised care. Furthermore, we believed that specialised nephrology centres could not provide any advantage to patients referred for the wrong reasons, that nephrology clinics would be saturated with patients and the waiting list would grow in length, and that nephrologists should not take up the slack of family doctors. Towards the end of 2006, the nephrology department, along with the primary care management team for our reference population, started to develop an integrated clinical management programme for the population with kidney diseases and difficult-to-control arterial hypertension through coordination between primary caregivers and the nephrology department of the Parc Tauli Health and University Corporation, Sabadell (Barcelona). We have followed up this programme for 3 years, which was consolidated with the publication of the Spanish Society of Nephrology (SEN) and Spanish Society of Family and Community Medicine (SEMFYC) consensus document on chronic kidney disease.9 The objective of our study is to present the results from applying a coordinated care programme between primary and nephrology care based on consultations and the use of a shared clinical information system in order to facilitate communication and improve the criteria for adapting and prioritising referrals.
MATERIAL AND METHOD
The Parc Taulí Health and University Corporation is responsible for a reference population of 426,000 people, and is located in the Vallès Occidental Este, Barcelona health region. This region is served by 42 primary care centres, compiled into 14 primary health care units, and 230 family doctors. In 2006, the nephrology department and the primary care management team elaborated and agreed upon a programme for coordinating the care given to patients with kidney diseases and difficult-to-control AHT. The previous experience from the Valencian Autonomous Community was heavily considered in the elaboration of this programme. Primary care consultation agendas were created in the nephrology department, with a reference nephrologist; a reference family doctor was also appointed. In-person and electronic clinical consultations with the reference nephrologist have been progressively implemented in the majority of primary care units. Furthermore, the requests that did not fulfil the criteria for a referral were denied and returned with a report explaining the clinical criteria established by the consensus. The primary care laboratory used the MDRD-4 IDMS formula for estimating glomerular filtration rates. The in-person clinical consultation sessions were also combined with a practical and jointly agreed upon training programme to inform family doctors as to the ways in which nephrological clinical problems were understood and managed in the nephrology department. The periodic consultation/training sessions were initially held once every month, and then once consolidated, every 2-3 months. However, the electronic consultations were held on a permanently open basis, with a response time of 2-4 days.
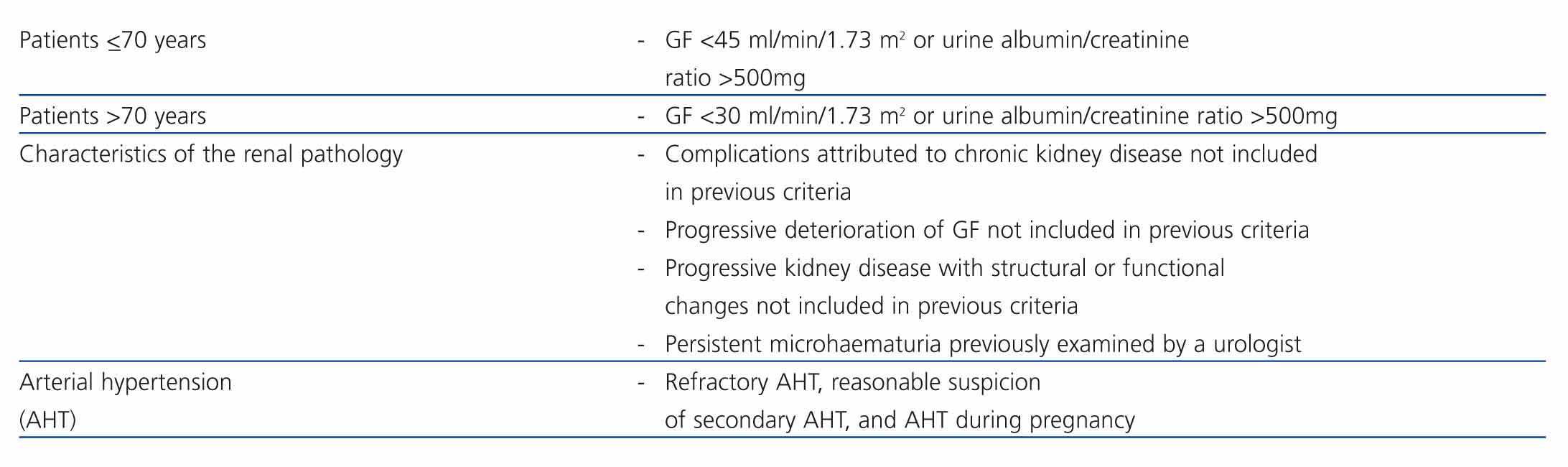
Starting in the year 2008, the criteria for referring patients to the nephrology department due to CKD were adapted, taking into account the SEN-SEMFYC consensus document on chronic kidney disease.9 A summary of the general criteria for referring patients to the nephrology department is displayed in Table 1. We would like to point out the importance given to the age of the patient, greater than or less than/equal to 70 years, which was used to set the cut-off level of deterioration for glomerular filtration rate at less than 30 or 40 ml/min/1.73m2 respectively. Patients with filtration rates below this threshold should be referred to a nephrologist. Furthermore, if it was established that the patient’s glomerular filtration rate was progressively deteriorating, regardless of the levels previously mentioned, the patient must also be referred to a nephrologist. Complications caused by CKD that were not included in the previously mentioned criteria, such as nephrogenic anaemia susceptible to treatment with erythropoietic agents, and proteinuria detected by an albumin/creatinine ratio greater than 500mg/g were also causes for referral. Progressive kidney failure with structural or functional changes, such as polycystic kidney disease, glomerulopathies, and tubulopathies, regardless of the values observed in glomerular filtration rate and proteinuria was also a reason for referral. Cases of haematuria were examined by the urology department before being referred to a nephrology unit. With regard to arterial hypertension, those cases of refractory AHT, reasonable suspicion of secondary AHT, and AHT during pregnancy were referred.
For the last two years, we have used a shared clinical information system called “Salut en Xarxa” (Health in Xarxa) in the evaluation of information on referrals from primary health providers and for the corresponding elaboration of reports when the consensus criteria were not upheld. This shared clinical information system has allowed us to gain access to the laboratory results, prescriptions, referrals to specialists, and clinical comments made by family doctors. These doctors had also access to all types of reports, laboratory results, and pathology/radiology reports originating in the hospital. The nephrology department assessed the adequacy of the referrals, and in the case of inadequate referral, a report was written with the pertinent explanations and recommendations for the case. This system has allowed us to prioritise the response time for requests from primary health care providers; thus, in the case of requests that have been confirmed as high-priority, such as in cases of asymptomatic patients with serum creatinine levels greater than 3mg/dl detected in primary health care, a specific programme ensured a visit within the week. Symptomatic cases have been referred directly to hospital emergency services for nephrological examination and possible hospitalisation.
The data regarding the denial of requests has been compiled from medical reports. The statistical analysis was performed with ANOVA descriptive statistics, using SPSS statistical software for Windows, version 15.
RESULTS
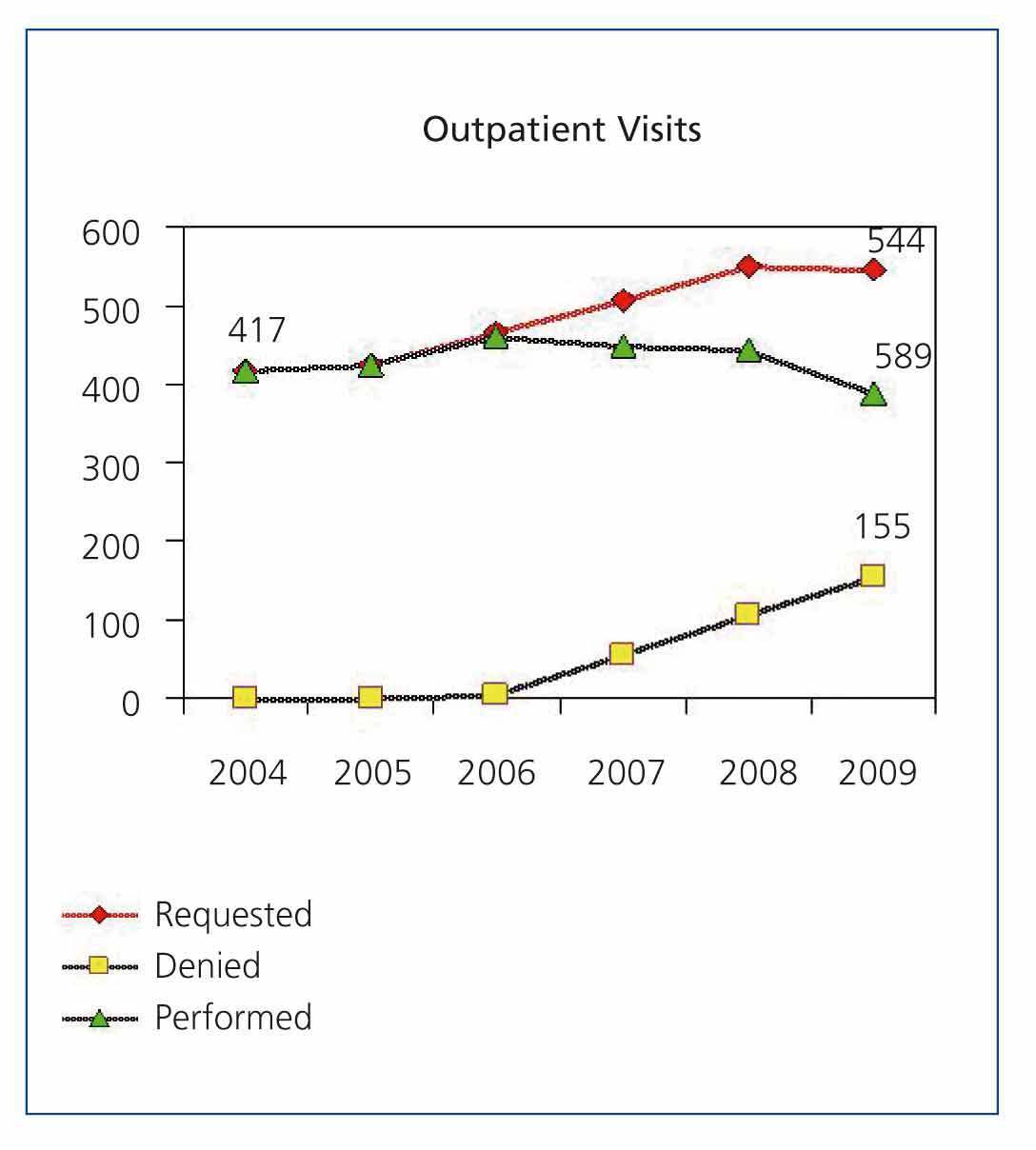
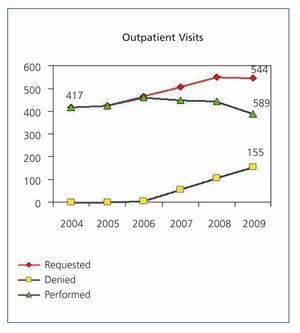
For the last 3 years, nephrological consultations have been progressively implemented in our reference population area. As the number of primary care units with access to the consultations increased, it was easier to apply and explain the consensus criteria agreed upon with the primary care management team to the rest of the department. These consultations provided a personalised relationship, rapid access to a nephrologist, and continuous training. Figure 1 shows the progression since 2004 of the first nephrology visits requested by primary health care providers, those cases denied and returned with an explanatory report, and the visits performed. The number of nephrology visits requested from primary health care providers increased from 417 in 2004 to 544 in 2009 (30.46%), but in 2009 the number of requested visits stabilised. However, we have observed a reduction in the number of first nephrology visits made that originated in primary care, and a clear change in tendency occurred since the coordinated care programme was initially implemented. Denied requests made up 28.49% of the total number of requested visits in 2009. Ninety-six e-mails with their respective clinical cases were exchanged between primary health care providers and the nephrology department in 2009, and the number of successive visits continued to increase, with patients more and more highly selected. Thus, whereas 5263 successive visits were held in outpatient clinics during 2006, 6616 were held in 2009, an increase of 5.53%.
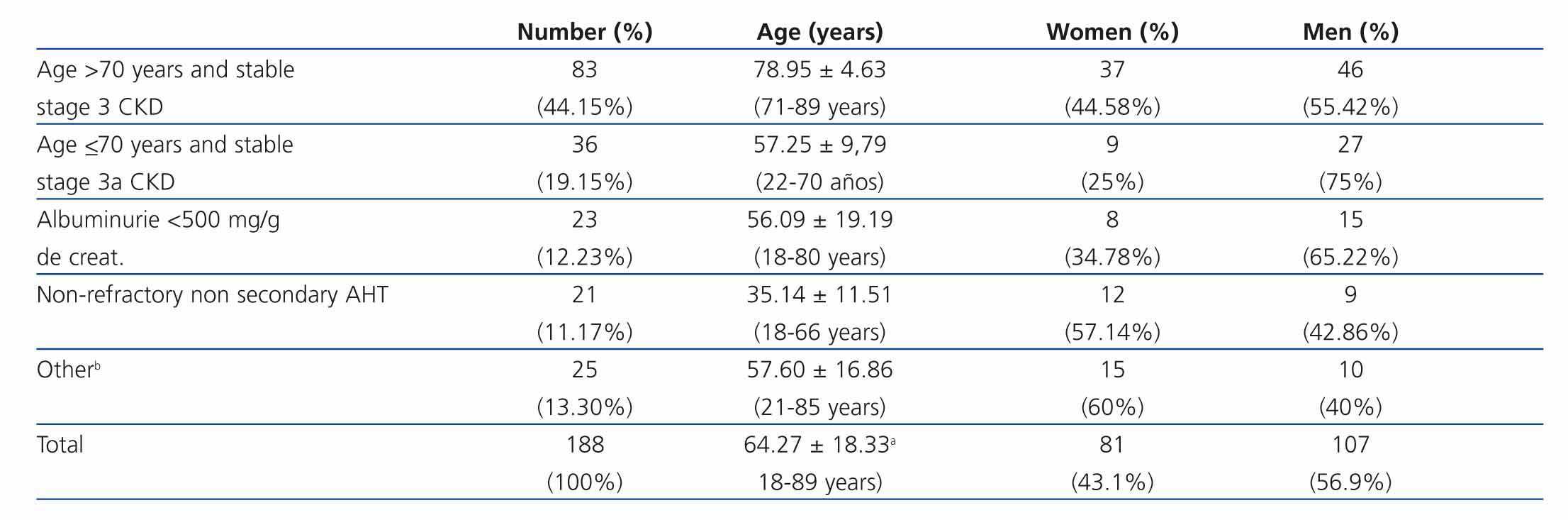
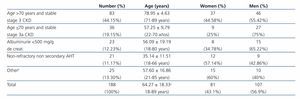
We analysed the reasons for rejection of first visit requests sent to the nephrology department from primary health care providers during a one-year period between 30 June 2009 and 1 July 2010, using the reports filed for each request. During this period, of a total of 559 first visit requests sent from primary health care providers to the nephrology department, 188 were denied (33.63%). Table 2 displays the reasons for denial. Here we must point out that the main cause was the presence of stage 3 CKD (MDRD-estimated glomerular filtration rate >30ml/min/1.73 m2) in patients older than 70 years (44.15%), followed by stage 3a CKD (MDRD-estimated glomerular filtration rate 45-59ml/min/1.73 m2) in patients <70 years old (19.15%). Isolated proteinuria expressed as an albumin/creatinine ratio <500mg/g was the cause in 12.23% of cases. In the ANOVA analysis, the criteria related to the glomerular filtration rate compared with those related to proteinuria corresponded significantly to a population 12 years older (P=.007). Another significant cause for denying requests was non-secondary, non-refractory essential AHT (11.17%). In the “Other” group, several different causes are included, such as: simple renal cysts, renal agenesis, solitary kidney, isolated haematuria not yet assessed by an urologist, mild hyperkalaemia, residual lesions in renal ultrasounds, etc. The mean time elapsed between the request for the visit from primary care and the actual visit was 61 days, but priority cases were preferentially handled within one month, and cases of the high priority (rapidly progressing renal failure) were seen within one week. Emergency cases, such as acute renal failure and hypertensive crisis, required patient admission in emergency services.
The following topics were focused on in the continuous training of family doctors: presentation and discussion of the coordinated care programme, epidemiology of chronic kidney disease, AHT and pregnancy, refractory AHT, recommended medications for AHT (Interlevel consensus document: primary-nephrology care), assessment of proteinuria, renal cysts, conservative treatment of advanced kidney failure, therapeutic compliance, assessment of hyperkalaemia, diabetic nephropathies, renal failure and drugs, secondary effects of anti-AHT drugs, use of diuretics, and kidney failure in elderly patients.
No instances of conflict were produced, and family doctors expressed their satisfaction with the methodology used.
DISCUSSION
The Spanish public health system is organised into the realms of primary health care and specialised care. The primary health care has attempted to follow the recommendations of the World Health Organisation (WHO) International Conference held in Alma-Ata in 1978, with Spain’s participation, which produced a tangible innovation in the conceptualisation of primary health care.10 In this model, primary health care is placed at the nucleus of the health system, and is charged with health care, promotion, and prevention activities. The three critical points for the development of primary health care have been the integration of family doctors into full-time employment, the establishment of clinical histories, and the capacity to train residents in family and community medicine.11 Within this framework, specialised health care takes its place as the leader in knowledge and procedures for the specific aspects of health problems. Coordination and communication with primary health care providers is essential in order to offer an adequate health care service to the population at large, and professional confidence to family doctors. The lack of communication between the realms of primary and specialised health care providers is a real and tangible issue in the Spanish health system.11
The high prevalence of CKD, especially in elderly patients, requires a work system coordinated with primary health care providers. The prevalence of CKD of 23.62% in people older than 64 years in Spain, as indicated by the EPIRCE study,5 cannot be tackled by nephrology alone, and coordination with primary health care providers is necessary. The most common form of CKD is stage 3, which affects elderly patients most of all. Its progression only requires kidney replacement therapy within 5 years in 1.3% of cases, but it has an elevated mortality (24.3%), mostly due to cardiovascular problems.12 In addition, follow-up of patients with stage 4 CKD and estimated glomerular filtration rate from >15 to <30ml/min/1.73m2 indicates that the majority of elderly patients with mild proteinuria and slow deterioration of kidney function does not need kidney replacement therapy, but tight collaboration with primary care providers.13 As the patient’s age increases, glomerular filtration rate progressively decreases,14 although not all cases involve a decrease, since this condition is not observed in a third of the elderly population without hypertension.15 Kidney disease in elderly patients is generally characterised by hypertension-related nephroangiosclerosis, which is frequently accompanied by diabetic nephropathies and other pathological processes.16 The clinical progression of this condition can be slow,17,18 and the rate of renal deterioration can be lower than in young patients.19
The methodology for coordination is a challenge for current nephrological clinical practice. Coordination and shared treatment are key factors for responding to this important health care need. Some shared treatment programmes for patients with kidney disease have revealed that up to 30% of kidney patients do not require direct visits with nephrologists when maintaining consistent treatment through primary health care providers.20 Coordination must be based on agreed upon protocols with criteria for referrals and shared treatment. Cardiovascular risk prevention is a general function of primary care that must be shared with specialised care providers for the different typical pathologies, such as diabetes mellitus, kidney failure, cardiopathies, AHT, peripheral arteriopathy, and cerebral ischaemia. The primary health care management boards are key pieces in the effort to come to a consensus on the criteria for patient referral and shared treatment. After the criteria are agreed upon, in situ consensus must be reached with the family doctors at each health centre in order to put these criteria into practice. In our experience, continuous training of primary care providers regarding common referral aspects and shared nephrological treatment is very enriching and a valuable tool. The reports on referrals that were considered inadequate for specialised care have also been a useful tool for this continuous training. The absence of conflicts with primary health care providers with such a high rate of denied requests for first nephrology visits has confirmed that our methodology is appropriate. Another source of referrals for first visits to outpatient nephrology units are those internally generated at the hospital, but these have not been analysed in this study. The selection process for first visits with a nephrologist has not led to a decrease in outpatient nephrological activity, on the contrary, we have observed a continuous increase in successive visits (25.71% increase in the last 4 years) as a consequence of the increase in patients cared for. We also must take into account that this increase in successive visits has occurred even in spite of the higher rate of patients discharged from outpatient nephrology units and left to the care of family doctors as the criteria for referrals from the coordination protocol have been implemented. All of these processes have resulted in an increased number of successive visits of more complex nephrology patients requiring greater attention. One of the areas of growth in our outpatient non-transplant nephrology services has been the increasing number of kidney transplant patients in the postoperative stabilisation phase, following clinical guidelines for non-transplant nephrology departments.21
Shared clinical information in the public health system is necessary for efficient and high-quality health care. Redundancy in the examinations between primary and specialised health care would be pointless, and there would be no reason not to share clinical information between different levels of the health system. Information and communications technologies have allowed us to establish shared clinical histories between health care providers. The advantages of this instrument are evident in the improved efficiency of the system and daily clinical practice. An area of medicine such as nephrology, in which it is easy to establish criteria for the severity of pathologies through complementary examinations and drug prescriptions, the application of objective criteria for referral must be easy when necessary information is available, as in our case. This all allows us to speak of a continuum health care without the need for the physical presence of a patient in the nephrology unit that is suffering a non-life threatening kidney disorder. According to our experience, this shared clinical information tool, called “Salut en Xarxa” in our region, is extraordinarily useful. In the case of a preferential referral of a patient suffering severe renal failure, we can know the current glomerular filtration rate and the evolution from previous laboratory results, and the same can be said of requests for referral due to proteinuria. Furthermore, in the case of AHT, the progression of medication prescribed can be taken into account, and strategies for clinical treatment can be suggested according to the clinical protocols from the consensus, without the need to perform a visit.
In conclusion, our coordinated care programme with primary health care providers has yielded a clear improvement in the adequacy of patient prioritisation and referrals to the nephrology department. The fundamental elements of this process have been: a programme agreed upon with the primary care management team, the SEN-SEMFYC consensus document on CKD, a shared clinical information system, in-person and electronic consultations, explanatory reports and recommendations in the cases of denied referrals, and a programme for continuous training of primary health care providers.
Table 1. General criteria established in the consensus for referring patients from primary care to nephrology specialists
Table 2. Reasons for rejecting requests for first visits sent by primary health care providers
Figure 1. Progression of the first nephrology visits requested by primary health care providers