Renal infarction is an uncommon event that often goes undetected due to its symptoms and analytical data being non-specific.1 The most frequent causes of renal infarction are embolic events (due to atrial fibrillation, thromboembolism after a myocardial infarction or release of atheromatous plaque),2 although it may also be secondary to thrombosis3 or renal artery dissection.4 Typical clinical manifestations include nausea, vomiting and intractable abdominal pain, although renal infarction may also be asymptomatic.5 Ventricular aneurysms are a complication in 30% of anterior myocardial infarctions and they are accompanied by several additional complications, such as sustained ventricular tachycardia, arterial embolism or heart failure.6,7
We present the case of a patient with a renal infarction secondary to a ventricular aneurysm caused by a prior myocardial infarction.
The 61 year old patient came to the Emergency Department due to intense pain in the right renal fossa lasting 5 hours. Medical history included primary arterial hypertension, dyslipidaemia and an acute myocardial infarction in 1997 that was treated by placing a stent in the right coronary artery. The patient was undergoing treatment with acetylsalicylic acid, nitroglycerin, simvastatin and diltiazem. Physical examination revealed a blood pressure of 143/94mm Hg, heart rate of 84 beats per minute, and lack of a fever. The patient experienced intense pain in right renal fossa, with no other abnormalities.
The Emergency Department laboratory analysis found the following: haemoglobin, 13.5g/dl; leukocytes, 14 300/µl; platelet count, 201 000/µl; creatinine, 1.17mg/dl (baseline 1mg/dl); urea, 42mg/dl; sodium, 136mmol/l; potassium, 3.8mmol/l; alanine transaminase, 66IU/l; aspartate transaminase, 97IU/l; bilirubin, 0.9mg/dl; gamma-glutamyl transferase, 28IU/l; alkaline phosphatase, 43IU/l; lactate-dehydrogenase (LDH), 2124IU/l; creatine-kinase, 1210IU/l; C-reactive protein, 1.1mg/dl. The systematic urine analysis showed only 5-10 leukocytes per field.
Electrocardiography was performed, revealing sinus rhythm with several ventricular and atrial extrasystoles. The Emergency Department performed an abdominal ultrasound which showed no inflammatory changes in the right iliac fossa. It was concluded that the kidneys presented no significant abnormalities.
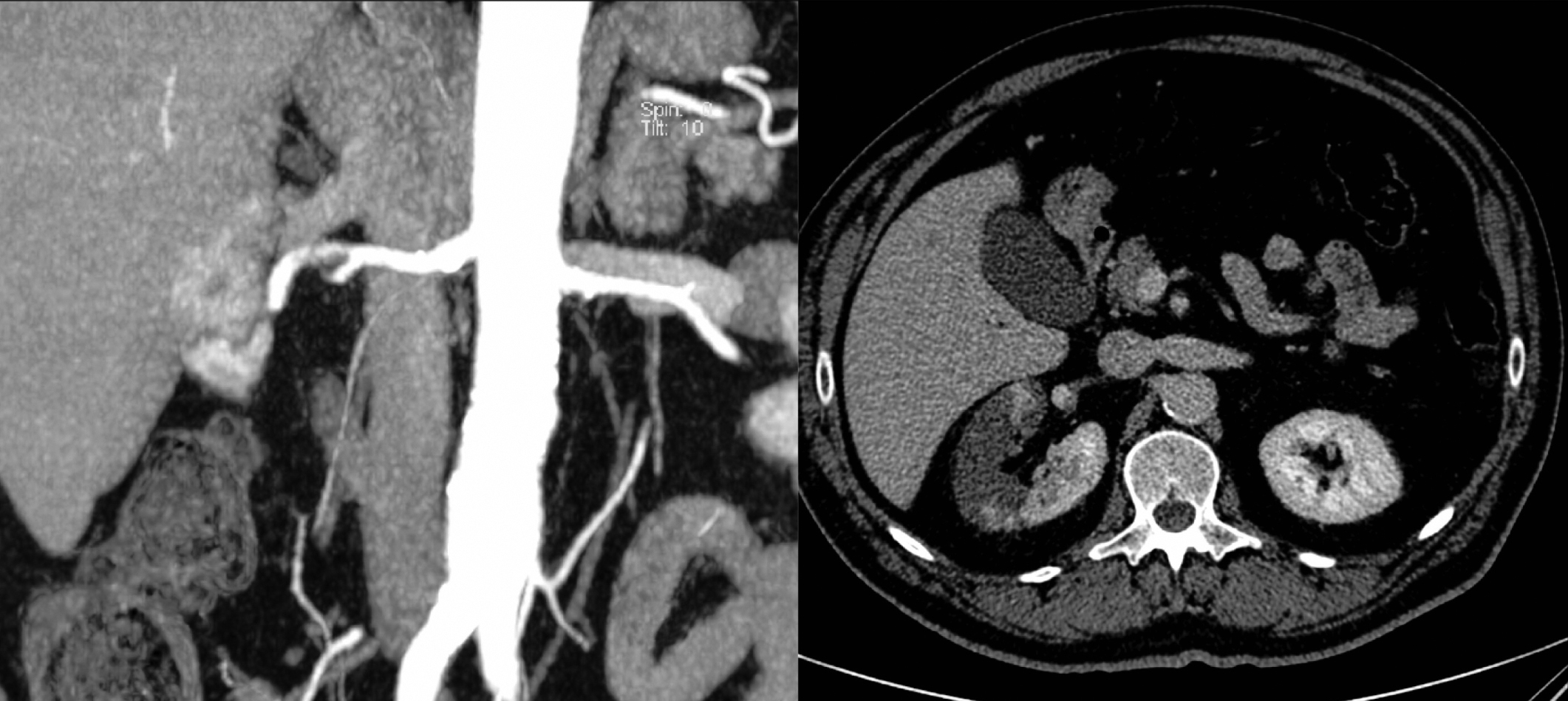
Given the patient’s intense pain and high LDH level, computed tomography was performed. The scan revealed an extensive right renal infarction with a filling defect in the main renal artery, proximal to its trifurcation (Figure 1).
The patient was admitted and began systemic anticoagulation therapy with heparin sodium.
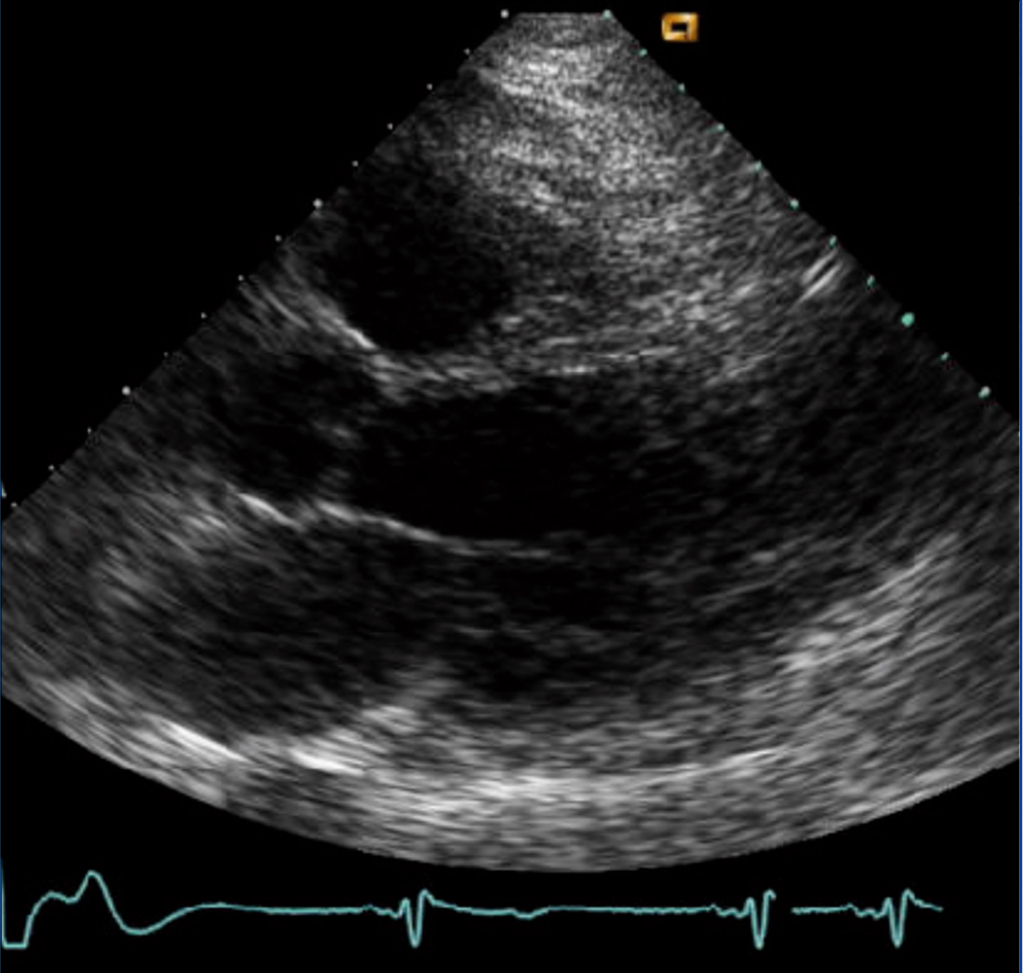
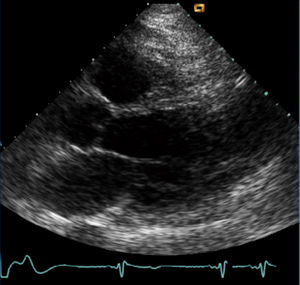
The echocardiogram performed on the day after hospital admission showed akinesis of the inferior septum, inferior wall and distal third of all walls, with an aneurysm of the distal thirds of the anterior and lateral walls; left ventricular ejection fraction 35%; mild to moderate mitral regurgitation; and mild tricuspid regurgitation (Figure 2). A Holter monitor confirmed the presence of multiple ventricular extrasystoles.
During the following days, the patient’s renal function decreased to 1.6mg/dl, at which point it stabilised.
The interesting feature of this case is that thromboembolic events following an infarction due to a left ventricular thrombus usually appear in an early stage (the first 4 months),8 while in our patient, they occurred 15 years later. Likewise, in 80% of all cases, left ventricular aneurysms follow infarction of the anterior descending artery,9 while our patient had an occluded right coronary artery. At the present time, the option of fitting the patient with a defibrillator is being considered.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Figure 1. Different computed tomography views of the right renal infarction
Figure 2. Echocardiogram showing the ventricular aneurysm