To the Editor,
Anti-neutrophil cytoplasmic antibodies (ANCA) are antibodies directed against neutrophil granulocytes and monocytes.1 These ANCA are essential markers and help to classify small-vessel vasculitides, such as Wegener’s granulomatosis (WG), microscopic polyangiitis (MP) and renal-limited vasculitides, which are classified as ANCA-associated systemic vasculitides.2
The diagnosis can be confirmed when ANCA are detected. This means that treatment with steroids and immunosuppressants can be started without delay.3 In contrast to anti-glomerular basement membrane antibody (anti-GBM) disease, these vasculitides are chronic diseases with a high relapse rate which leads to increased morbidity/mortality.4 Thus, a diagnosis of relapse in a patient with ANCA-associated small-vessel vasculitis with persistently negative ANCA titre at the moment of a possible relapse should be questioned, requiring either histological proof of disease activity or exclusion of other diagnoses.5 On the other hand, whether persistently positive levels of ANCA or an increase in their levels can predict vasculitis disease activity is more controversial.4,5
We describe here the case of a patient diagnosed with MP with positive ANCA at the time of diagnosis. The patient did not have any relapses for 7 years while the ANCA were negative and then had 2 relapses in the following 4 years with persistently positive ANCA and while under immunosuppressive maintenance therapy.
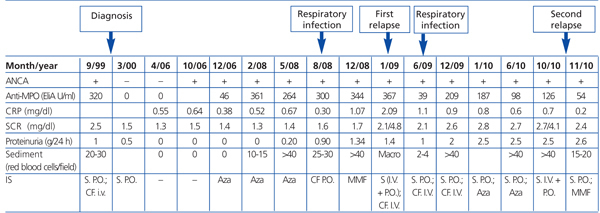
The patient was a 74-year-old male diagnosed with ANCA-positive MP (anti-myeloperoxidase [anti-MPO] antibodies at a titre of 320U/ml, negative anti-PR3 antibodies) in September 1999. He was treated with oral prednisone at 1mg/kg and monthly pulses of 750mg of cyclophosphamide for 6 months. He also had a medical history of tuberculosis in his youth; spondyloarthrosis and osteoporosis; collapse at D10 vertebra as a complication of steroid treatment; chronic hepatitis with positive HBs-Ag, and positive anti-HBe coinciding with the diagnosis of vasculitis. The patient had been asymptomatic for 7 years with stable kidney function (oscillations of serum creatinine with a range of 1.3-1.8mg/dl), persistently negative ANCA and without immunosuppressive maintenance therapy. From the seventh year following diagnosis of MP, we started to detect positive ANCA (positive anti-MPO). The follow-up of the evolution of the ANCA, kidney function parameters and the immunosuppressive treatment established is shown in Table 1.
A year and an half after detecting the positive ANCA, the patient was admitted for a respiratory infection without pulmonary consolidation which was treated with levofloxacin. During this hospitalisation, plasma creatinine was 1.4mg/dl, proteinuria 0.28g/24h, C-reactive protein 13mg/dl and an ANCA titre that oscillated between 410 and 429U/ml was found.
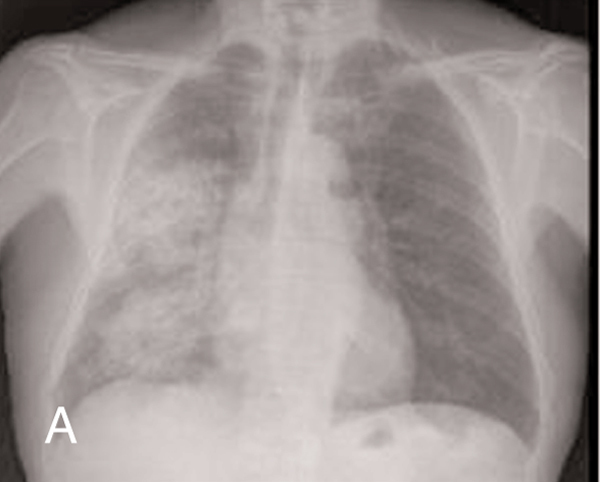
The first relapse of the disease was found two years and 3 months after the ANCA had become positive and while the patient was undergoing immunosuppressive treatment with oral cyclophosphamide at 50mg/day. The patient had anti-MPO at a titre of 367U/ml and the relapse appeared as acute non-oliguric renal failure (creatinine peak at a maximum of 6.6mg/dl), microscopic haematuria and pulmonary haemorrhage in the right lung (Figure 1) that responded to treatment with 500mg pulses of 6-methylprednisone i.v. (three doses) followed by oral prednisone at 1mg/kg/day and 500g pulses of cyclophosphamide. Two months after this first relapse, the patient was admitted to hospital for another respiratory infection without pulmonary consolidation that responded well to levofloxacin.
The second relapse of the disease was detected four years after the reappearance of the ANCA. This was also seen in the deterioration of kidney function (serum creatinine peak at 4.1mg/dl) and microscopic haematuria and with anti-MPO titres of 126U/ml. The patient responded well to treatment with 500mg pulses of 6-methylprednisolone followed by a descending dosage of oral prednisone starting at 1mg/kg/day and treatment with mycophenolate mofetil at a dose of 500mg/day. The patient was asymptomatic three months after this second relapse with a serum creatinine level of 2.7mg/dl, persistent microhaematuria (20-25 red blood cells/field), a C-reactive protein of 0.7mg/dl and an anti-MPO titre of 13U/ml.
Relapses are the main problem of vasculitides given that they cause mortality and morbidity to increase: chronic organ damage (renal failure) and increased cumulative immunosuppressive therapy toxicity.4,6 Although the value of ANCA is well established in the diagnosis of these diseases, the usefulness of measuring ANCA titres in assessing disease activity is more controversial.7 Increased anti-PR3 is associated with a relapse in patients with WG, whereas, persistently high anti-MPO in MP is more contentious. Lurati and Spertini analysed the predictive value of ANCA as a relapse marker in a retrospective study that included 36 patients (23 with WG and 13 with MP). They studied the prognostic potential of an acute increase in the ANCA titre compared to a persistently positive level of ANCA: persistently high ANCA (over 6 months) were not found to be significantly associated with disease relapse in their study, and the predictive value of an acute increase in the ANCA titre was related to the size of the increase.8
In our case, the patient had two relapses over a period of 4 years, during which the anti-MPO titres remained persistently high and, furthermore, the patient was undergoing immunosuppressive maintenance therapy. Also, the relapses occurred regardless of the level of anti-MPO detected: although the first relapse occurred with anti-MPO levels above 350U/ml, the anti-MPO levels had been above 400U/ml a few months before at the time of a respiratory infection, and at this point no relapse had been noted. In the second relapse, the anti-MPO level had been similar to the previous month’s levels (<150U/ml). Ayada et al also described a similar case to ours with anti-MPO titres that had been persistently positive for 6 years. The anti-MPO levels were not valuable for predicting relapse early.9
While monitoring ANCA in patients with vasculitis may be helpful for the clinician and may be useful to make a decision on whether to start immunosuppressive treatment, the final decision must be based on clinical and histological parameters in addition to other analytical parameters.9 In our case, considering that the patient had only received induction therapy when the disease was diagnosed, and still did not have symptoms to consider disease activity (stable kidney function without proteinuria), preventative immunosuppressive therapy was started when the ANCA reappeared 7 years after the diagnosis and the patient had the first relapse 2 years after starting this treatment.
Activation of T-cells, genetic and exogenous causes and infections have been included among the factors associated with relapse. In our case, the patient had been admitted to hospital for a respiratory infection with a maximum peak of anti-MPO within normal levels, although the vasculitis activity was seen seven months later.
Furthermore, the reason for preventing relapses is to avoid chronic organ damage. In our case, it can be seen that after the relapse, a progressive worsening of kidney function along with an increased proteinuria was noted.
To conclude, persistently positive anti-MPO in patients with MP may not be very useful for predicting relapse, even more so if the patients are undergoing immunosuppressive maintenance therapy, although clinical monitoring must be even stricter in patients with persistently positive anti-MPO titres.
Table 1. Evolution of ANCA titre, kidney function parameters, immunosuppressive treatment and relapses
Figure 1a. Pulmonary haemorrhage in the right hemithorax (A) before treatment and (B) after receiving immunosuppressive treatment.
Figure 1b. Pulmonary haemorrhage in the right hemithorax (A) before treatment and (B) after receiving immunosuppressive treatment.