Objetivo: El objetivo principal del estudio es el análisis de la evolución de la función renal residual según la técnica de diálisis (diálisis peritoneal o hemodiálisis) y la frecuencia del tratamiento (dos o tres sesiones de hemodiálisis a la semana). Como objetivos secundarios hemos estudiado la evolución de la concentración sérica de β2-microglobulina y la respuesta de la anemia a los agentes eritropoyéticos. Material y métodos: Se incluyeron 193 enfermos no anúricos, que comenzaron tratamiento renal sustitutivo con diálisis en nuestro hospital entre el 1 de enero de 2006 y el 31 de diciembre de 2011, y tuvieron un seguimiento superior a tres meses. De ellos, 61 enfermos (32 %) iniciaron tratamiento con dos sesiones de hemodiálisis a la semana, 49 enfermos (25 %) con tres sesiones de hemodiálisis a la semana y 83 enfermos (43 %) con diálisis peritoneal. Se midió el filtrado glomerular como la media de los aclaramientos renales de urea y creatinina. Resultados: El ritmo de descenso del filtrado glomerular fue igual en los enfermos que comenzaron tratamiento con la pauta de dos sesiones de hemodiálisis a la semana y con diálisis peritoneal (mediana 0,18 ml/min/mes) y fue superior en los enfermos que iniciaron tratamiento con tres sesiones de hemodiálisis a la semana (mediana 0,33 ml/min/mes, p < 0,05). A lo largo de toda la evolución, la tasa de filtrado glomerular no mostró diferencias entre el grupo que comenzó con dos sesiones semanales de hemodiálisis y el grupo de diálisis peritoneal, y fue inferior en el grupo que comenzó tratamiento con tres sesiones de hemodiálisis a la semana con significación estadística durante los primeros 24 meses de seguimiento. En los tres grupos de enfermos la concentración de β2-microglobulina fue aumentando conforme disminuía el filtrado glomerular y fue más elevada en el grupo de tres sesiones de hemodiálisis a la semana durante los primeros 12 meses de seguimiento. En todos los controles realizados hubo una correlación negativa entre la concentración de β2-microglobulina y el filtrado glomerular (p < 0,001). La dosis de eritropoyetina se relacionó negativamente con el filtrado glomerular. Los enfermos que comenzaron con dos sesiones de hemodiálisis a la semana necesitaron una dosis menor de eritropoyetina que los enfermos que iniciaron tratamiento renal sustitutivo con tres sesiones a la semana. La dosis de eritropoyetina en el grupo de diálisis peritoneal fue inferior a la del grupo de dos hemodiálisis a la semana, a pesar de mantener un filtrado glomerular similar. Conclusiones: Los enfermos que comienzan tratamiento con dos sesiones de hemodiálisis a la semana experimentan el mismo ritmo de descenso de la función renal residual que los enfermos tratados con diálisis peritoneal. La evolución de la concentración de β2-microglobulina es paralela a la del filtrado glomerular. Los enfermos tratados con dos sesiones de hemodiálisis necesitan una dosis de eritropoyetina menor que los que reciben tres sesiones a la semana, pero significativamente superior a la de los enfermos tratados con diálisis peritoneal, lo cual indica que la respuesta de la anemia a los agentes eritropoyéticos no solo está relacionada con la función renal residual, sino también con otros factores inherentes a la técnica de diálisis.
Objective: The main objective of the study was to analyse the progression of residual renal function according to the dialysis technique (peritoneal dialysis or haemodialysis) and the frequency of treatment (two or three sessions of haemodialysis per week). As secondary objectives, we studied the progression of the serum concentration levels of β2 microglobulin and the response of anaemia to erythropoietic agents. Material and method: 193 non-anuric patients were included and began renal replacement therapy with dialysis in our hospital between 1 January 2006 and 31 December 2011, with a follow-up period of over three months. 61 patients (32%) began treatment with two haemodialysis sessions per week, 49 patients (25%) with three haemodialysis sessions per week and 83 patients (43%) with peritoneal dialysis. The glomerular filtration rate was measured as the mean of the renal clearances of urea and creatinine. Results: The rate of decrease in glomerular filtration was the same in patients who began treatment with two haemodialysis sessions per week and with peritoneal dialysis (median 0.18ml/min/month) and it was higher in patients who began treatment with three sessions of haemodialysis per week (median 0.33 ml/min/month, P<.05). Throughout progression, the glomerular filtration rate did not display differences between the group that began with two weekly sessions of haemodialysis and the group on peritoneal dialysis, and it was lower in the group that began treatment with three sessions of haemodialysis per week with statistical significance during the first 24 months of follow up. In the three patient groups, β2- microglobulin concentration increased as the glomerular filtration rate decreased and it was higher in the group on three weekly haemodialysis sessions for the first 12 months of follow up. In all the controls carried out, there was a negative correlation between the beta-2 microglobulin concentration and the glomerular filtration rate (P<.001). The erythropoietin dose was negatively related to glomerular filtration. Patients who began with two sessions of haemodialysis per week required a lower dose of erythropoietin than patients that began renal replacement therapy with three weekly sessions. The erythropoietin dose in the peritoneal dialysis group was below that of the group of two weekly haemodialysis sessions despite maintaining a similar glomerular filtration rate. Conclusions: Patients who begin treatment with two sessions of haemodialysis per week experience the same rate of decrease in residual renal function as patients treated with peritoneal dialysis. The progression of the concentration of β2-microglobulin is parallel to that of the glomerular filtration rate. Patients treated with two haemodialysis sessions require a lower dose of erythropoietin than those who receive three sessions per week, but a significantly higher dose than those treated with peritoneal dialysis, which suggests that the response of anaemia to erythropoietic agents is not only related to residual renal function, but also to other factors that are inherent to the dialysis technique.
Residual renal function is important for prognosis in patients treated with peritoneal dialysis and those treated with haemodialysis and its preservation should be one of the goals of renal replacement therapy.1-6 The regular measuring of residual renal function is part of the treatment protocol for patients treated with peritoneal dialysis, since it is used to calculate the total dose of dialysis received. However, it is not normally analysed in patients undergoing regular haemodialysis and it is assumed that the dialysis dose is provided exclusively by the dialyser. For reasons that are not fully known, the decrease in residual renal function is quicker after treatment with haemodialysis, and perhaps this is one of the reasons for there being less interest in it being measured.
It is common practice in peritoneal dialysis units to begin renal replacement therapy with a low dose of peritoneal clearance that will increase as residual renal function decreases.7,8 On the contrary, it is common in periodic haemodialysis units to start treatment with the standard regimen of three weekly sessions of haemodialysis (3HD/week). However, Gotch established in 1985 that if the renal clearance of urea is equal to or higher than 2.5ml/min, an adequate dose of dialysis can be achieved by the urea kinetic model with two weekly haemodialysis sessions (2HD/week).9
From 2006, we decided to establish a progressively increasing dialysis regimen for patients beginning haemodialysis treatment, in which we consider the possibility of starting with 2HD/week if the renal clearance of urea is equal to or higher than 2.5ml/min. In a previous study, we observed that patients on this regimen had better preservation of residual renal function.10
In this study, we tried to test whether the progression of residual renal function in patients starting treatment with 2HD/week is similar to that of patients on peritoneal dialysis. We also analysed the progression of anaemia and serum β2-microglobulin concentration, as a clear influence of residual renal function has been observed on the response to erythropoietic agents11-15 and the level of β2-microglobulin11,16-19 both in patients treated with haemodialysis and with peritoneal dialysis.
MATERIAL AND METHOD
In this study, we have included all patients starting renal replacement therapy with dialysis in our hospital between 1 January 2006 and 31 December 2011 and who remained on dialysis for more than three months. Patients who were anuric at the time of starting dialysis were excluded, as well as those who were carriers of a kidney transplant and had resumed dialysis due to graft dysfunction.
In accordance with our clinical protocol, residual renal function was measured routinely in all patients treated with dialysis by determining the glomerular filtration rate as the arithmetic mean of the urinary clearances of urea and creatinine. In patients treated with haemodialysis, clearance was calculated from urea and creatinine concentrations in urine collected during the 24 hours before the first haemodialysis session of the week and in the blood sample obtained immediately before starting the session.20,21
The first measurement was usually carried out in the first week of renal replacement therapy and was considered as the baseline glomerular filtration rate. It was subsequently repeated every 2-3 months until diuresis was less than 100ml/day; from this time, it was considered that the patient was anuric and that residual renal function was zero.
Patients treated with peritoneal dialysis started treatment with two daily exchanges of 1.5-2 litres of glucose solution with lactate, which is our normal starting regimen when patients have residual renal function. As the glomerular filtration rate decreased, the number of exchanges was increased or the patient changed to nocturnal automated peritoneal dialysis.
In patients on haemodialysis, when urea clearance in the first glomerular filtration rate measurement was equal to or higher than 2.5ml/min/1.73m2, we attempted to begin treatment with the regimen of 2HD/week (Monday and Friday or Tuesday and Saturday) if the clinical situation allowed it, in accordance with the criteria of the doctor in charge. This regimen was maintained until renal clearance of urea decreased below 2.5ml/min/1.73m2 or clinical symptoms and/or laboratory changes appeared, in which case, an increase in frequency was advised. The time on haemodialysis was initially set at 3.5 or 4 hours per session, according to whether the dry weight was below or above 60kg. All patients were dialysed with a high patency biocompatible membrane (polyamide with an ultrafiltration coefficient of 71ml/mmHg/h or polysulfone with an ultrafiltration coefficient of 55ml/mmHg/h) and ultrapure dialysate. In our treatment protocol, the post-dilution online haemodiafiltration technique is reserved for patients with low or zero residual renal function. The start of haemodialysis treatment was considered scheduled when the patient had a functioning arteriovenous fistula.
As a general rule, patients on peritoneal dialysis receive a daily oral dose of 80mg of furosemide; patients on haemodialysis with a regimen of 2HD/week also receive this dose of furosemide on the days on which they do not undergo dialysis.
The end date of the study was 30 June 2012. The rate of the glomerular filtration decrease (ml/min/month) and 24 hour diuresis (ml/month) was established as follows: in patients who began with the regimen of 2HD/week, the difference was calculated between the baseline glomerular filtration rate and the glomerular filtration rate in the last measurement carried out before treatment on the aforementioned regimen was ended due to transplantation, death, recovery of renal function, transfer to peritoneal dialysis or to a regimen of 3HD/week or the patient’s glomerular filtration rate on the end date of the study if the 2HD/week regimen was continued; the difference was divided by the months elapsed between both measurements. In patients who began with 3HD/week or on peritoneal dialysis, the difference was calculated between the baseline glomerular filtration rate value and the last glomerular filtration rate value obtained before it was considered that the glomerular filtrate had disappeared (diuresis below 100ml/day), or the glomerular filtration rate before ending treatment with dialysis (due to transplantation, death or recovery of renal function), or the value of the glomerular filtration rate before the change of technique (transfer from haemodialysis to peritoneal dialysis or vice-versa), or the glomerular filtration rate value at the time of the end of the study in the event that the patient had preserved residual renal function at that time and remained with their original dialysis technique. This difference was divided by the number of months in the period analysed. The same procedure was carried out to calculate the decrease in diuresis.
In each of the groups studied we collected glomerular filtration rate value on the dates closest to 6, 12, 18, 24, 30 and 36 months on dialysis. In patients without residual renal function on the dates analysed, the glomerular filtration rate value was considered equal to 0. On the same dates on which the glomerular filtration rate was determined, the following parameters were collected: serum haemoglobin and β2-microglobulin concentrations and the weekly dose of erythropoietin (IU week/kg).
Statistical analysis
To test the goodness of fit of the data to a normal distribution, we used the Kolmogorov-Smirnov test. The results are expressed as mean ± standard deviation for normally distributed data. The decreases in the glomerular filtration rate and diuresis are not normally distributed, and the results are expressed as median and the 25th and 75th percentiles (interquartile range). Quantitative variables were compared with the Student's t test, Mann-Whitney test or ANOVA, as appropriate. Qualitative variables were compared with Χ2 test. The relationship between variables was assessed using Spearman's test and Pearson’s test, as appropriate. We used the log-rank test to compare Kaplan-Meier survival curves. The data analysis was carried out with the intention to treat: each patient was assigned to their initial group of treatment regardless of subsequent changes. The progression time corresponds to the time of dialysis treatment, and it was censored at the time of death, kidney transplantation, recovery of renal function or loss of progression due to transfer to another hospital. P values <.05 were considered to be statistically significant.
RESULTS
From 1 January 2006 to 31 December 2011, 224 patients with preserved diuresis were incorporated into the chronic dialysis schedule of our hospital and remained on dialysis for over three months. 31 patients with kidney transplants who recommenced dialysis treatment due to chronic graft dysfunction (24 treated with haemodialysis and 7 with peritoneal dialysis) were excluded. One hundred and ninety-three patients began treatment with renal replacement therapy for the first time and they are those included in the study group. One hundred and ten patients began treatment with haemodialysis: 61 (32%) with the regimen of 2HD/week, because they had baseline renal urea clearance equal to or higher than 2.5ml/min/1.73m2, whenever their clinical situation allowed it, in accordance with the criteria of the doctor in charge (2HD/week group), and 49 (25%) with the regimen of 3HD/week (3HD/week group). Eighty-three patients (43%) began treatment with peritoneal dialysis (PD group). Of the 49 patients who began treatment with haemodialysis with the regimen of 3HD/week, 25 had baseline urea clearance higher than 2.5ml/min/1.73m2, but the doctor responsible decided to begin with the aforementioned regimen due to clinical complications such as heart failure, high blood pressure or volume overload. Of the 110 patients who began treatment with haemodialysis, 55 (50%) did so as scheduled haemodialysis, with an arteriovenous fistula as vascular access. It was more common to start scheduled haemodialysis in the group which began treatment with 2HD/week (35 patients, 64%) than in the 3HD/week group (20 patients, 36%), but the difference was not statistically significant (Χ2 2.98, P=.124).
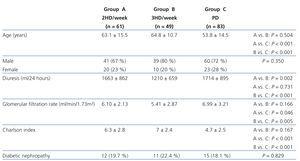
The characteristics of patients at the start of treatment are displayed in Table 1. Patients who began treatment with peritoneal dialysis were younger and had lower Charlson index (age-comorbidity) values and a higher baseline glomerular filtration rate than patients treated with haemodialysis, while these variables were not significantly different between the groups on 2HD/week and those on 3HD/week. Patients in the 3HD/week group had lower baseline diuresis than those in the other two groups. The prevalence of diabetic nephropathy was similar in the three groups.
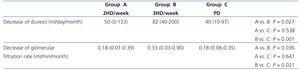
Table 2 displays the decrease in diuresis and the glomerular filtration rate in the three groups of patients. The glomerular filtration rate and diuresis decreased more rapidly in the 3HD/week group, with no differences being observed between the 2HD/week and PD groups. There was no statistically significant correlation between the decrease in the glomerular filtration rate and the baseline glomerular filtration rate (r=.118, P=.098) or age (r=.0757, P=.293), but there was a positive correlation with the Charlson index (r=.157, p=.027). The decrease in the glomerular filtration rate was not influenced by the presence of diabetes mellitus as the cause of renal failure: diabetic 0.22 (0.01-0.53), non-diabetic 0.20 (0.04-0.42) ml/min/month (median and interquartile range, p=.884), or by patient sex: male 0.18 (0.03-0.44), female 0.24 (0.05-0.46) ml/min/month (median and interquartile range, p=.194) or in the subgroup of patients treated with haemodialysis due to beginning scheduled or non-scheduled haemodialysis: scheduled start 0.23 (0.05-0.67), non-scheduled start 0.19 (0.02-0.55) ml/min/month (median and interquartile range, p=.470).
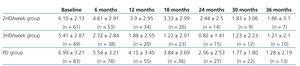
The progression of the glomerular filtration rate in the three groups of patients is displayed in Table 3. From the control in month six onwards, there were no statistically significant differences between the 2HD/week and PD groups. In the 3HD/week group, the glomerular filtration rate continued to display statistically significant differences with respect to the other two groups until the control at month 24.
In Table 4 we display the progression of serum β2-microglobulin concentration. Between the 2HD/week and PD groups, there are only statistically significant differences at baseline. In the 3HD/week group, serum β2-microglobulin concentration is higher until the control at month 18 with respect to the 2HD/week group and until the control at month 12 with respect to the PD group. In all the controls carried out, including baseline, there was a negative correlation between the level of β2-microglobulin and the glomerular filtration rate (P<.001 in all controls). The concentration of β2-microglobulin increased throughout progression as the glomerular filtration rate decreased (P<.001).
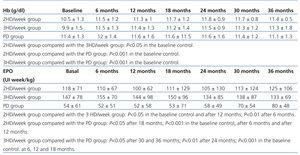
Parameters associated with anaemia are expressed in Table 5. In the baseline control, there were statistically significant differences between the three groups with regard to haemoglobin concentration and erythropoietin dose. The Charlson index was negatively related to baseline haemoglobin (r=-0.33, p<.001) and positively to the weekly dose of erythropoietin (r=0.33, p<.001). In the group of patients treated with haemodialysis, the scheduled start was associated with higher baseline haemoglobin (10.8±1.5 vs. 9.6±1.6g/dl, p=.004), at a lower dose of baseline erythropoietin (104±61 vs. 168±78IU weekly/kg, p<.001). Throughout the remainder of progression, there were no longer differences in haemoglobin concentration in the three groups. The weekly erythropoietin dose was lower in the PD group throughout progression, but the differences were statistically significant until the control at month 18 with respect to the 2HD/week group and until the control at month 36 with respect to the 3HD/week group. The erythropoietin dose was lower in the 2HD/week group with respect to the 3HD/week group until the control at month 12. In all the controls carried out, except for the control at month 36, there was a statistically significant negative correlation between the erythropoietin dose and the glomerular filtration rate.
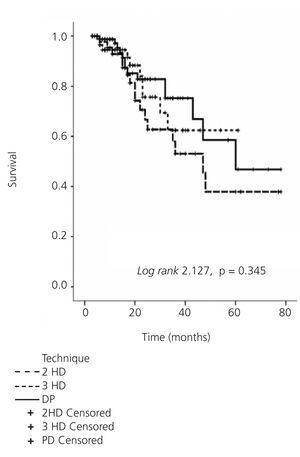
Follow-up time on dialysis was 18.6±13.4 months (94.8 patients-year) in the 2HD/week group, 24.7±19.6 months (101.1 patients-year) in the 3HD/week group and 22.4±16.8 (154.8 patients-year) in the PD group, without there being statistically significant differences between the three groups. During the follow-up time on dialysis, 15 patients were anuric in the group that started with the regimen of 2HD/week (25%), 25 patients in the group that started with the regimen of 3HD/week (51%) and 17 patients in the PD group (20%) (p=.007 between the 2HD/week and 3HD/week groups, p<.001 between the 3HD/week and PD groups, p=.701 between 2HD/week and PD groups). Of the 61 who started renal replacement therapy with 2HD/week, 25 changed to the 3HD/week regimen due to a decrease in residual renal function after a period of time ranging from 3 to 25 months (9±6 months). 23 patients received a kidney transplant in the 2HD/week group (15 while they were being treated with two weekly sessions of haemodialysis), as well as 16 patients in the 3HD/week group and 42 patients in the PD group. Of the 83 patients who started peritoneal dialysis treatment, 10 were transferred to the haemodialysis technique after a period of 21±16 months (range 3-48 months) on the initial technique. Ten patients in the 2HD/week group (mortality 10.5/100 patients-year), 16 patients in the 3HD/week group (mortality 15.8/100 patients-year) and 14 patients in the PD group (mortality 9/100 patients-year) died. The Kaplan-Meier analysis did not display statistically significant differences in survival between the three groups of patients (log-rank 2.127, p=.345) (Figure 1).
Of the 83 patients who started treatment with peritoneal dialysis, 19 changed to automated peritoneal dialysis with a cycler during the study period; of the total 110 patients who started on haemodialysis, 13 received treatment with the convective technique throughout progression. All patients experienced a significant reduction in or complete loss of residual renal function.
DISCUSSION
The main objective of our study was to study the influence of different dialysis techniques and regimens on the decrease in residual renal function. We have compared the progression of residual renal function as measured by the glomerular filtration rate in patients treated with peritoneal dialysis and two haemodialysis regimens: two and three sessions a week. We excluded from the study patients who recommenced dialysis after kidney transplant dysfunction, since their residual renal function decreased faster22 and their prevalence was higher in the group of patients treated with haemodialysis.
The decrease in residual renal function and diuresis was the same in patients treated with peritoneal dialysis and those who started with the 2HD/week regimen; both groups had a similar glomerular filtration rate throughout their progression. Patients who started renal replacement therapy with the 3HD/week regimen had a quicker decline in residual renal function and maintained a glomerular filtration rate below that of the two previous groups during the first two years of progression. The baseline glomerular filtration rate was higher in the group of patients treated with peritoneal dialysis, but we did not observe a correlation between the decrease of the latter and its baseline level.
The reasons why the loss of residual renal function is faster in patients treated with haemodialysis than in peritoneal dialysis patients remain unclear. The induction of inflammatory reactions by the dialyser membrane or dialysate is one of the reasons considered. Isolated studies have observed a similar decrease in the rate of residual renal function in both techniques when patients undergoing haemodialysis are treated with ultrapure dialysate and high-flux membrane.23,24 All patients in our study used this type of dialysate and membrane, however, the decline in residual renal function was greater in the group that started haemodialysis with the normal regimen of 3HD/week. The higher preservation of residual renal function in patients treated with 2HD/week had already been observed by Lin et al.25 in a prevalent, selected population followed up for 6 months (23 patients treated with two weekly sessions and 51 with three weekly sessions). The reason is unclear and cannot be attributed to differences in hydration status or blood pressure control, because in a cross-sectional study in our unit we found that both parameters were similar in patients treated with two or three weekly sessions of dialysis.10
Unlike other studies, we did not observe a relationship between the rate of decrease in residual renal function and age, the baseline glomerular filtration rate or the existence of diabetes mellitus.26,27 As with other authors,28 we did observe a correlation between the decrease in residual renal function and the comorbidity index. Patients who started renal replacement therapy with peritoneal dialysis or with a 2HD/week regimen received a low dose of oral furosemide. We do not believe that this treatment had a bearing on the preservation of residual renal function, since there is no evidence that furosemide preserves the glomerular filtration rate in patients on dialysis;29 its administration may even accelerate the rate of decrease.27 In patients treated with peritoneal dialysis, the repercussions of using icodextrine, biocompatible solutions or the automated technique on the preservation of residual renal function is a controversial subject.29-33 It is not clear if the convective techniques of haemodialysis have a protective effect.34 In our dialysis unit, automated peritoneal dialysis and on-line haemodiafiltration are usually reserved for patients with low or no residual renal function and we cannot analyse its potential influence therein.
Several studies attribute a prognosis value to the level of β2-microglobulin in patients treated with haemodialysis.35,36 Residual renal function is one of the factors that determine its serum concentration in patients treated with haemodialysis or peritoneal dialysis.11,16-19 In our study, baseline concentration of β2-microglobulin was different in the three patient groups. We attribute this to the differences observed in the glomerular filtration rate at the beginning of dialysis, since, although the difference did not reach statistical significance between the two haemodialysis groups, there was a highly significant correlation between the baseline values of β2-microglobulin concentration and the glomerular filtration rate. The subsequent progression of β2-microglobulin concentration was parallel to that of the glomerular filtration rate: there were no differences between patients treated with peritoneal dialysis and those who began haemodialysis with a 2HD/week regimen and the levels were higher in patients who began renal replacement therapy with a 3HD/week regimen. In the three groups, β2-microglobulin concentration increased as residual renal function decreased and in all the controls carried out there was an excellent correlation between both.
Patients treated with peritoneal dialysis require a lower dose of erythropoietin than patients treated with haemodialysis.37-39 One reason that may explain this phenomenon is the difference in preservation of residual renal function, since the latter influences the response of anaemia to erythropoietic agents in both types of dialysis.12-15 In a cross-sectional study, we found that patients treated with the 2HD/week regimen, and therefore, with better residual renal function, required a lower dose of erythropoietin to maintain identical levels of haemoglobin as patients treated with a 3HD/week regimen.10 The current study confirms these findings: the difference in erythropoietin dose between the two haemodialysis regimens was maintained throughout progression while differences in residual renal function persisted. Until the month 36 control, the dose of erythropoietin had a statistically significant negative correlation with the glomerular filtration rate. However, patients treated with peritoneal dialysis required a lower dose of erythropoietin than patients in the 2HD/week group, despite maintaining similar residual renal function throughout progression. The better response of anaemia to erythropoietic agents in peritoneal dialysis cannot be exclusively attributed to better preservation of residual renal function, but rather, it must be influenced by other factors. It should be highlighted that haemoglobin concentration and erythropoietin dose were different in the three patient groups at the beginning of dialysis treatment. These data may be explained in part by the negative influence of the age-comorbidity index and the non-scheduled start in the haemodialysis group on anaemia.
In conclusion, patients who began treatment with dialysis with the 2HD/week regimen had a rate of decrease in residual renal function that was equal to that observed in the group of patients treated with peritoneal dialysis. Both patient groups maintained a similar glomerular filtration rate throughout progression, which was significantly higher than the GFR of the 3HD/week group. The progression of β2-microglobulin was similar, which confirms the importance of residual renal function on the serum concentration of the latter. Patients who began treatment with the 3HD/week regimen required a higher erythropoietin dose than the other two groups, but the erythropoietin dose with peritoneal dialysis was significantly lower than the 2HD/week regimen, which indicates that, as well as the glomerular filtration rate, other factors inherent in the dialysis technique influence the response of anaemia to erythropoietic agents.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Data at the start of dialysis
Table 2. Decrease in diuresis and the glomerular filtration rate
Table 3. Progression of the glomerular filtration rate (ml/min/1.73 m²) in the three patient groups
Table 4. Progression of serum levels of beta-2 microglobulin (mg/l) in the three patient groups
Table 5. Progression of the parameters related to anaemia in the three patient groups
Figure 1. Actuarial survival graph