Introducción: En un estudio publicado en 2011 se observó que en la Comunidad Canaria la supervivencia de los pacientes incidentes en diálisis peritoneal (DP) es mejor que la de los pacientes incidentes en hemodiálisis (HD). El inicio de HD con catéter venoso central condiciona un peor pronóstico, por lo que el acceso vascular de inicio podría condicionar la comparación de la supervivencia entre ambas modalidades. Objetivo: Realizar un estudio comparativo en nuestra comunidad de la supervivencia a medio plazo de los pacientes incidentes en tratamiento renal sustitutivo según la modalidad, separando a los pacientes incidentes en HD según el acceso vascular de inicio: acceso vascular arteriovenoso desarrollado o catéter venoso central. Material y métodos: Se trata de un estudio de cohortes longitudinal retrospectivo, que incluyó todos los pacientes incidentes en tratamiento renal sustitutivo entre enero de 2005 y diciembre de 2010 seguidos hasta diciembre de 2011 en tres de los grandes hospitales de la Comunidad Canaria y se dividieron, según la modalidad de inicio, en DP, HD con acceso vascular desarrollado (HD-FAV) y HD con catéter venoso central (HD-Cat). Se estimaron las curvas de supervivencia en los distintos grupos mediante Kaplan-Meier y se aplicó un modelo de riesgos proporcionales de Cox de supervivencia para estimar los riesgos relativos de mortalidad de DP, frente a HD-FAV y HD-Cat, ajustando para edad e índice de comorbilidad de Charlson. Posteriormente se realizó el mismo análisis por subgrupos definidos por la edad y presencia de diabetes. Resultados: Se incluyeron 1110 pacientes, mediana de edad 63 años, 56 % diabéticos. El análisis de Kaplan-Meier muestra una mejor supervivencia de DP (66 meses) frente a HD-Cat (41 meses), log-rank p < 0,001, no existiendo diferencia entre DP y HD-FAV (67 meses). En la regresión de Cox el riesgo relativo de mortalidad de la HD-Cat frente a la DP fue de 2,270 (1,573-3,276); p < 0,001. No se observó diferencia entre los pacientes HD-FAV y DP 0,993 (0,646-1,525). El análisis por subgrupos muestra estos mismos resultados en diabéticos y no diabéticos, y en los pacientes más jóvenes y en los más añosos. Conclusiones: La mejor supervivencia en DP frente a HD observada en el registro de enfermos renales de la Comunidad Canaria parece a expensas de los pacientes incidentes en HD-Cat, no observándose diferencia entre DP y HD-FAV. Estos resultados podrían sugerir que, en nuestro medio, aquellos pacientes en los que, optando inicialmente por HD, no se consigue un acceso vascular desarrollado en la etapa prediálisis podrían obtener un beneficio de supervivencia ofreciéndoles la DP como técnica de inicio, al menos hasta disponer de un acceso vascular definitivo.
Introduction: A study published in 2011 showed that patients in the Canary Islands, who were incident in peritoneal dialysis (PD) had better survival than those who were incident in hemodialysis (HD). Since initiating hemodialysis with central venous catheter is associated with worse prognosis, it would be possible that the initial vascular access influences the results of survival comparison between both groups. Objective: To conduct a comparative medium-term survival study of patients incident in renal replacement therapy with different modalities in our community, classifying those incident in hemodialysis according to the initial vascular access: established arteriovenous vascular access or central venous catheter. Material and method: Retrospective longitudinal cohort study including all patients who were incident in renal replacement therapy between January 2005 and December 2010, with follow-up until December 2011, in three large hospitals of the Canary Islands. Patients were classified according to the initial modality: PD, HD with established vascular access (HD-FAV) or HD with central venous catheter (HD-Cat). Kaplan-Meier survival curves were estimated for each group and a Cox proportional hazards survival model was used to estimate relative mortality risk for DP as compared to HD-FAV and HD-Cat, adjusting for age and Charlson comorbidity index. An equivalent analysis was then conducted on subgroups defined by age or by the presence of diabetes. Results: 1110 patients were included, with a median age of 63 years, 56% of them were diabetic. A Kaplan-Meier analysis showed better survival for PD (66 months) as compared to HD-Cat (41 months), Log Rank p<.001, with no difference between DP and HD-FAV (67 months). Cox regression RR of mortality for HD-Cat versus PD was 2.270 (1.573-3.276); p<.001; no differences were found between HD-FAV and PD patients 0.993 (0.646-1.525) n.s. Subgroup analysis showed equivalent results for diabetic and non-diabetic patients as well as for younger or older ones. Conclusions: better survival of PD patients as compared to HD ones, observed in the Canary Islands, seems to be based on incident HD patients with central venous catheter, while no differences were found between PD and HD with established vascular access. These results could suggest that patients in our community, for whom a vascular access cannot be achieved in predialysis, could have better survival if PD is offered as initial technique, at least until a vascular access is available.
INTRODUCTION
Survival in patients with chronic kidney disease who begin renal replacement therapy is a subject of vital importance and comparative studies between patients treated with peritoneal dialysis (PD) and haemodialysis (HD) have frequently shown conflicting results. Since there are no large controlled prospective studies, most discrepancies can be explained by the methodological and design differences and population differences of the observational studies.1-11 In fact, when a critical analysis was carried out on the studies published with the aim of eliminating methodological discrepancies, it seems that the results of both techniques were similar, although, there may be differences between different patient subgroups, and these may vary over time. Specifically, it appears that PD has a slightly higher survival rate in the first 1-2 years and that it is more accentuated for younger, non-diabetic patients; after the first few years, either no differences were observed, or in some studies HD displayed better survival, especially in diabetic and older patients.12,13
In 2011, a study was published that compared survival between PD and HD in recent years in the Community of the Canary Islands. In this community, it was shown that PD patients have a survival advantage over HD patients regardless of age and whether they are diabetics or non-diabetics, and this advantage was maintained beyond the early years of treatment.14 A recent study suggested that initial vascular access in HD may change the association between dialysis modality and survival.15 In the comparative analysis of the Canary Islands Registry study14 initial vascular access and comorbidity were not taken into account and patients were only analysed by age and presence of diabetes. Since the proportion of patients starting dialysis with a central venous catheter was particularly high in the Canary Islands,16 we decided to undertake the present study to assess the medium-term survival of incident PD and HD patients, separating HD patients in accordance with their initial vascular access (central venous catheter or arteriovenous fistula), and adjusting comparisons by the Charlson comorbidity index.
MATERIAL AND METHOD
This is a retrospective longitudinal cohort study that included all incident patients on renal replacement therapy between January 2005 and December 2010 and with follow-up until December 2011 in three of the main hospitals in the Community of the Canary Islands (Hospital Universitario de Gran Canaria Doctor Negrín, Hospital Universitario Insular de Gran Canaria and Hospital Universitario de Canarias de Tenerife). We calculated the modified Charlson comorbidity index17 at the start of renal replacement therapy and the incident patients were divided into three groups: initial PD, initial HD with developed vascular access (HD-FAV) and initial HD with central venous catheter (HD-Cat).
In each group considered, the categorical variables were summarised in frequencies and percentages and the numerical variables in means and medians and the interquartile range according to the distribution of the latter. The percentages were compared using the Χ2 test and the medians using Wilcoxon’s test for independent data. The survival curves were estimated in accordance with the initial dialysis technique using the Kaplan-Meier method and the curves were compared using the log-rank test. Subsequently, a multidimensional analysis was carried out using the Cox regression model. Variables were selected using the likelihood-ratio test. The resulting models were expressed through P-values and relative risk (RR), which were estimated by confidence intervals at 95% (95% CI). A contrast of hypotheses was considered statistically significant when the corresponding P-value was below 0.05.
Analysis was performed from time zero, the study event was patient death from any cause, in case of transfer between PD and HD we censored follow-up time, unless the death occurred within 60 days of the change of technique, in which case it was assigned to the initial modality. The causes of termination of the study were patient death, loss to follow up, change of dialysis technique (except in the aforementioned case in which death occurred within 60 days of the change), transplantation and reaching the study completion date.
Since the profiles of diabetic and non-diabetic patients displayed major differences and differences were reported in survival for each dialysis technique in accordance with diabetes mellitus and age, a survival analysis was also carried out according to the initial technique by age and presence of diabetes subgroups.
RESULTS
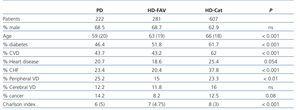
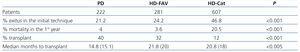
The cohort included a total of 1110 incident patients on renal replacement therapy with a mean age of 61±14 years (median 63 years, interquartile range 20), 65.5% male, 56% diabetic. The aetiology of chronic renal failure was: diabetic nephropathy 43.8%, vascular 10.4%, glomerular 7.9%, polycystic disease 8.1%, unknown 14.4%, other 14%. 20% (222) began with PD, 25.3% (281) began with HD-FAV and 54.7% (607) began with HD-Cat. Table 1 displays the demographic and clinical data of the three groups and it is highlighted that the HD-Cat group had an older age, a higher percentage of diabetics, more history of cardiovascular disease, and therefore, a higher Charlson comorbidity index. The PD and HD-FAV groups were quite similar, with a slightly older age in HD-FAV and a higher history of peripheral vascular disease and cancer in the PD group. Table 2 displays that the gross rate of overall mortality in the first year of treatment was higher in the HD-Cat group, while the transplantation rate was higher and the time until transplantation lower in the PD group.
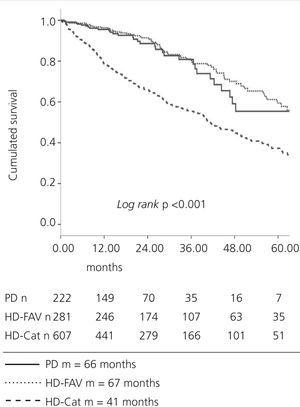
When we compared survival by Kaplan-Meier between HD and PD, similar results were obtained for this cohort to those obtained in the data of the Canary Islands registry,14 with better survival for PD (median of 66 months) compared with HD (median 51 months); P<.001. Using a Cox proportional hazards model, adjusted for the Charlson index and starting age, RR of HD compared with PD was 1.871 (CI 95% 1.299-2.694); P<.001. When we separated HD patients according to initial vascular access, we observed that the difference between HD and PD occurred mainly due to the worse survival of patients who began treatment with HD-Cat, as was observed in the Kaplan-Meier analysis, displayed in Figure 1. Cox’s regression model, adjusted for the Charlson comorbidity index and age shows RR for mortality of HD-Cat patients with respect to PD patients of 2.270 (1.573-3.276); P<.001, while no difference was observed between HD-FAV and PD patients 0.993 (0.646-1.525), as shown in Table 3. No differences were observed in survival between participating hospitals for any of the techniques. When the hospital in which treatment was received was introduced into Cox’s regression as a covariable, it was not significant. Since this covariable hardly changed change the RR resulting from the other covariables it was not introduced in the model.
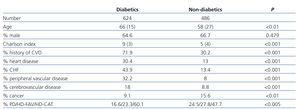
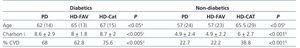
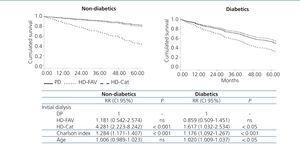
Tables 4 and 5 show the major differences in the baseline characteristics that the diabetic patients presented compared with the non-diabetics of the cohort, as well as the differences in the distribution of the different techniques by groups. In general, patients on HD-Cat presented a poorer comorbidity profile, both in the diabetic group and in the non-diabetic group. It is also notable, that in the diabetic group, patients who start with PD have a higher comorbidity index and a higher prevalence of cardiovascular disease than those on HD-FAV. These differences between diabetics and non-diabetics and the data published that suggest that survival in the different dialysis techniques may vary according to diabetes status justify analysing survival separately in both groups. Figure 2 represents Kaplan-Meier survival analysis by technique in both subgroups. The non-diabetics displayed similar survival between PD and HD-FAV patients, which was significantly higher than that of patients on HD-Cat. In diabetic patients, we did not observe a significant difference between patients on PD and those on HD-FAV and both had a significantly higher survival rate than those in the HD-Cat group. However, we did observe, unlike with the non-diabetics, that the survival curve would appear to be somewhat worse for PD patients than for HD-FAV patients. The higher comorbidity described in Table 5 of diabetic patients who started with PD probably had an influence, as well as the small number of patients who achieved a follow-up of over four years on PD. In fact, Figure 3 represents the graphs and results of the Cox regression model adjusted to the Charlson comorbidity index and age in diabetics and non-diabetics showing in both subgroups a higher RR of mortality in the HD-Cat group compared with PD (RR 4.281 (2.223-8.242); p<.001 in non-diabetics and RR 1.617 (1.032-2.534); p<.05 in diabetics) while no differences were found between HD-FAV and PD in both subgroups (RR 1.181 (0.542-2.574); not significant (ns) in non-diabetics and RR 0.859 (0.509-1.451) in diabetics).
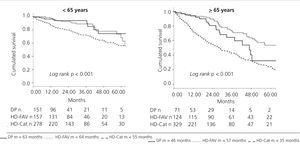
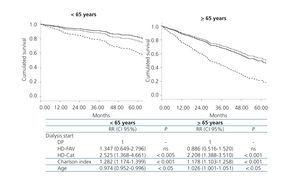
The analysis was also carried out by age subgroups and the cohort was divided into patients under 65 years of age and those who were 65 or older. Figure 4 displays the results of the Kaplan-Meier analysis and we observed in both age subgroups better survival in PD and HD-FAV patients than in HD-Cat patients. In the younger subgroup, survival in PD and HD-FAV was quite similar, while in the older subgroup, although the difference in survival between both techniques was not significant, there was a somewhat worse curve for PD than for HD-FAV. However, Figure 5 shows the results of the Cox regression model adjusted to the Charlson comorbidity index and age separately in both age subgroups showing in both subgroups a higher RR of HD-Cat compared with PD (RR 2.525 (1.368-4.661); P<.005 in <65 year olds and RR 2.208 (1.388-3.510); P<.001 in >65 year old), while no differences were found between HD-FAV and PD in both subgroups (RR 1.347 (0.649-2.796); ns in <65 year olds and RR 0.886 (0.516-1.520); ns in >65 years).
DISCUSSION
The comparative survival studies between HD and PD often displayed heterogeneous and even contradictory results.1-11 To demonstrate evidence of the difference in survival between both techniques, it would be necessary to conduct prospective controlled studies, but the few attempts carried out as in the Netherlands with the study integrated into the initiatives of The Netherlands Cooperative Study on the Adequacy (NECOSAD), have experienced many problems in recruitment, given the impossibility of randomising, since patients wished to choose one or another modality, and although the final result of this specific study favoured the patients included in PD, the final n of only 38 patients makes the results not very easy to extrapolate.18 A controlled study is currently underway in China and is in the recruitment stage with the aim of including more than 1000 patients, but it is expected that the results of this study will not be known until 2016 (clinicaltrials.gov: NCT01413074). Many of the heterogeneous results of the observational studies could be explained by differences in the characteristics of the populations studied, differences in the study designs and the statistical methods employed to analyse the results. When we attempted to carry out a critical analysis of the observational studies published, with the aim of eliminating the methodological differences, it seems that the results of both techniques were similar, although there may be differences between patient subgroups and these may vary over time. Specifically, it appears that PD offers better survival rates in the first 1-2 years of treatment and that this advantage is more accentuated in younger and non-diabetic patients. After the first years, some studies do not display differences between the techniques, while an advantage of HD is observed in others, particularly in diabetic and older patients.12,13,19-21
In 2011, a study was published comparing survival between HD and PD in the medium term in incident patients on dialysis in the Community of the Canary Islands in the last few years using a Cox proportional hazards model with adjustment based on the propensity analysis.14 This study showed better survival in PD compared with HD in this community, which was maintained over time beyond the second year and was observed in diabetics and non-diabetics and in younger and older patients alike. In the aforementioned study, the hypothesis was considered that these results may arise from the improvements experienced in PD in the last few years, such as the use of new, more biocompatible solutions, the increase in the use of automated dialysis or the improvement in continuous care for chronic kidney disease patients with the implementation of the advanced chronic kidney disease (ACKD) clinics. In fact, it has been demonstrated that in the last few years the survival results have been improving in incident PD patients in different cohorts.22-23
Initial vascular access has been shown to be an important determining factor of mortality in incident HD patients.24,25 As such, vascular access used initially in HD may determine the difference in survival between PD and HD patients,15,26 particularly bearing in mind, as has already been communicated in previous studies, that in the Canary Islands, a high percentage of incident patients on HD start with a central venous catheter.16 Our results show that the difference observed between PD and HD in our community was predominantly due to the worse survival rate of incident HD-Cat patients, with practically no difference being observed between PD patients and incident HD-FAV patients. In spite of the patients in the HD-Cat group being older and having greater comorbidity, higher mortality continued to be observed in the Cox regression model after adjusting it for both factors and as such, morbidity associated with the use of catheters is probably having a negative influence on survival in this group. It has been suggested that, analysing the results of the survival studies as a whole, and without the ability to clearly demonstrate the advantages of one or the other in the majority of patients, particularly in the first few years of treatment, survival should not be the main factor in the decision about the choice of technique, but rather, other factors should be predominant such as patient preference, the adaptation of the latter to the lifestyle and the socioeconomic impact on the system.27-30 The advantage of survival on PD in the first few years, which is observed in the studies of the main registries, has often been attributed to the better initial preservation of residual renal function compared with HD. Nevertheless, in our study and in others, it has been shown that, at least in part, it may be due to the negative impact of the HD catheters in the first few years of treatment. Thus, the sequential approach of using PD as a “bridge” modality for patients who had previously chosen HD and who do not have a mature and functioning vascular access in time could be an advantage for survival. In this sense, there is already experience in a centre that uses assisted PD for older patients who were referred late to dialysis, avoiding HD-Cat, which is the standard method for these patients in most centres.31
Undoubtedly, it would also be necessary to improve the percentage of incident patients with developed vascular access in order to comply with the guidelines of the Sociedad Española de Nefrología.32 Nevertheless, the efforts made in each participating hospital to improve the clinical procedures for obtaining vascular access in time did not yield the expected results, although there is surely obvious room for improvement. These data may be due, in part, to the demographic and clinical differences of the incident Canary Islands population, which shows clear differences to that of the mainland, which may in part explain the profile of the incident patient with the catheter. For example, in the ACKD clinics of the Canary Islands, a very high prevalence of diabetes mellitus has been reported: 50-65%; more than 60-70% of patients are overweight and of them, 25-40% are obese (body mass index >30kg/m2), there is a high prevalence of vascular calcifications and over 50% of patients have had a history of some cardiovascular event.33-35 All of the above result in a very poor profile for successfully achieving a functioning arteriovenous fistula. We do not have data for the whole cohort, but to further define the situation in our setting, we can break down the data of the incident patients in one of the participating hospitals in the last four years (data not published): of all the incident patients on renal replacement therapy, 35% were not treated in an ACKD clinic and most of these patients were unknown to the nephrology service or had been lost to follow-up in the last few years; of these, 93% started PD and of those who started HD, 51% did so with a developed vascular access and 49% with a central venous catheter; of the latter, 27% had at least one failed arteriovenous fistula attempt, 29% had been assessed for vascular access but it was not able to be scheduled for various reasons and 43% started treatment without access due to acute deterioration, most in the course of hospital admissions due to heart failure, cardiovascular events, sepsis or surgical complications. Despite these possible explanations, it is unquestionable that the high rate of incident patients with a catheter in our community and the unequal distribution of PD between hospitals requires a detailed analysis of our selection and initial renal replacement therapy processes and the implementation, by the healthcare system, of effective measures. For example, incentives have been suggested for objectives to increase the number of arteriovenous fistulas and achieve a rational use of the different techniques.
The fact that many patients who started with central venous catheter did not benefit from the pre-dialysis care in the CKDA clinics and that many started dialysis from admission to hospital due to associated complications has resulted in the suggestion that part of mortality attributable to the catheter may be due to a bias, since the most critically ill patients start with a venous catheter. This bias may also have an influence when survival is compared between HD and PD, given that patients with an urgent condition and in a more serious situation usually start with HD. In an attempt to eliminate this bias, Quinn et al. carried out a study in which they compared the risk of mortality in incident PD and HD patients, but only in patients who had begun renal replacement therapy and fulfilled two conditions: that they had received more than four months of care in clinics prior to dialysis and began with ambulatory dialysis, excluding patients who started dialysis from admission to hospital. After adjusting for comorbidity, no differences were found in mortality between PD and HD.36 We do not have a registry with the initial form of treatment for the whole cohort of our study, although we can analyse it in the subgroup of the 432 incident patients of the Hospital Insular de Gran Canaria. Of these patients, 232 (53.7%) began with scheduled ambulatory renal replacement therapy with more than four months’ follow-up in CKDA clinics, while the remainder began with non-scheduled treatment, either due to not having follow-up in nephrology CKDA clinics or beginning from an admission at hospital due to an additional medical complication. Of the 232 who had a scheduled start, 22% began with PD, 50% began with HD-FAV and 20% began with HD-Cat. If we compare the RR of mortality in HD with PD in this patient subgroup, adjusted to age and comorbidity, we do not find any significant differences (RR 2.229, CI 95% 0.688-7.224, ns), and if we separate them by starting vascular access, we observe a higher risk in HD-Cat patients compared to PD patients (RR 3.646, CI 95% 1.094-12.143, P<.05 and no difference between HD-FAV and PD (RR 1.450, CI 95%, 0.426-4.932 ns). Although it is necessary to interpret these results with caution due to the small number of patients, they could suggest that although there is a poor prognosis for survival due to the serious condition of the patient starting HD, there also appears to be a deleterious effect per se in using central venous catheters, which is plausible if we take into account the numerous and serious medical complications associated to their use: bacteraemia, sepsis, endocarditis, osteomyelitis, venous thrombosis, underdialysis, etc.
As for analysis by subgroups, our data show that there is a survival advantage in using PD compared with HD-Cat both in diabetics and non-diabetics and both in younger patients (<65 years) and in older patients (>65 years). When we compared PD with HD-FAV, no significant differences were observed in any of the subgroups in terms of survival time, but it is true that in the subgroup of diabetics and in the older subgroup, there appears to be an advantage in survival of HD-FAV patients compared to those on PD, although it is not statistically significant, perhaps due to the number of patients included. This could be in line with the findings of large registry studies that show that the advantage of PD compared with HD is particularly observed in younger, non-diabetic patients, while in older, diabetic patients, particularly from the second year, no difference or even better survival in HD is observed.37-41
Our study has many limitations. Firstly, it is a non-controlled observational study in which, although the groups are adjusted for comorbidity, since the study is not randomised, there will always be biases that escape us. Furthermore, the number of patients and geographical area is limited with specific health care and demographic characteristics and as such, its results cannot be extrapolated to other regions. Nevertheless, this characteristic is also of interest to the study given the progressive increase of obesity and diabetes in the last few years in incident patients on renal replacement therapy in other areas of the country; as such, the interaction between age, diabetes, starting technique and survival are more important. Another limitation is the use of survival analysis without bearing in mind the real time on each modality, by not taking into account the changes in technique carried out or subsequent vascular access changes in dialysis, which surely have an impact on survival in each group. Censoring for kidney transplants may be a negative bias that may be detrimental to the survival result quantified for PD patients, since in our study, a higher proportion of PD patients received transplants and earlier than in the other two groups, and as such, it is assumed that the younger and healthier patients in the PD group were censored early and contributed less survival time to their group. In a study, an attempt has been made, through a marginal structural adjustment model, to compensate for this PD prejudice.42
In conclusion, the advantage of survival in PD compared to that of HD in the Community of the Canary Islands seems to be at the expense of patients who begin treatment with HD-Cat, with differences not being observed with patients who began HD-FAV. These results may suggest that it would be possible to obtain an improvement in survival by proposing PD as a “bridge” modality for patients who had previously chosen HD and who did not have a mature functioning vascular access in time. To achieve this objective and improve the percentage of patients that start scheduled renal replacement therapy with developed vascular access, the development of multidisciplinary and clinical procedures and well-organised strategies in the CKDA clinics is necessary to achieve initial renal replacement therapy with the best guarantees and in respect of the patients’ modality of choice.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Description of the population in accordance with the initial dialysis technique
Table 2. Progression of the different groups
Table 4. Differences between diabetics and non-diabetics
Table 5. Differences in techniques between diabetics and non-diabetics
Figure 1. Analysis of survival by Kaplan-Meier in the three groups: peritoneal dialysis, haemodialysis with developed vascular access and haemodialysis with central venous catheter
Figure 2. Analysis of survival by Kaplan-Meier in the three groups: peritoneal dialysis, haemodialysis with developed vascular access and haemodialysis with central venous catheter, for diabetic and non-diabetic subgroups
Figure 3. The Cox regression model for survival of haemodialysis with developed vascular access and haemodialysis with central venous catheter compared to peritoneal dialysis adjusted to the Charlson index and age for diabetic and non-diabetic subgroups
Figure 4. Survival analysis by Kaplan-Meier in the three groups: peritoneal dialysis, haemodialysis with developed vascular access and haemodialysis with central venous catheter for the younger and older subgroups
Figure 5. Cox regression model for survival on haemodialysis with developed vascular access and haemodialysis with central venous catheter compared with peritoneal dialysis adjusted to the Charlson index and age by subgroups, the younger and older groups
12048_19157_50297_en_tabla_3.doc
Table 3. Cox regression model for survival in haemodialysis with developed vascular access and haemodialysis with a central venous catheter compared with peritoneal dialysis adjusted for the Charlson index and age