Thrombotic microangiopathy (TMA) may be the initial form of multiple diseases (atypical uraemic haemolytic syndrome, antiphospholipid syndrome [APS]), with its differential diagnosis expanding in kidney transplant patients (acute humoral rejection [AHR], calcineurin inhibitor toxicity). It is usually associated with poor kidney graft function, so it is important to start specific treatment early.1 In patients who present TMA associated with APS, the treatment is anticoagulation, although in cases with no response eculizumab has been used with good results.2
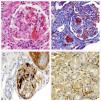
We present the case of a 60-year-old woman with a personal history of hypertension, ischaemic heart disease, paroxysmal atrial fibrillation, with mechanical mitral and aortic prostheses, two miscarriages, and end-stage chronic kidney disease of unrelated aetiology. As a result of having received multiple transfusions and pregnancies, the patient was hyperimmunised. She received her first deceased-donor kidney transplant, and immunosuppression was done with steroids, tacrolimus, mycophenolate, and induction with 7 doses of thymoglobulin. Because of the prosthetic valves, anticoagulation with sodium heparin was started within the first 48h after the transplant. Starting at day 2 post-transplant (PTD), the patient experienced a progressive increase in the urine output rate, but with no decrease in serum creatinine (sCr). However, from the 7 PTD, she presented with a decrease in urine output, and it was decided to perform a kidney biopsy on the 12 PTD. The biopsy showed 14 glomeruli, 6 of which presented capillary thrombi, exudative lesions, and endothelial swelling; the radial arteries presented thrombi and fibrinoid necrosis; C4d staining was positive in the peritubular capillaries (Fig. 1). In addition, the patient began to experience thrombocytopoenia (86,000/μl), anaemia (10.5g/dL), with low haptoglobin and one schistocyte per field on the peripheral blood smear.
Kidney biopsy. (A) Thrombi in the glomerular capillaries and afferent arteriole, fibrinoid necrosis, collapse of the glomerular capillaries (H&E). (B) Thrombi in the glomerular capillaries and arterioles (Masson). (C) CD61+ stain in the glomerular capillaries. (D) C4d+ stain in the peritubular capillaries.
Given these symptoms, the first suspected diagnosis was TMA associated with AHR in a hyperimmunised patient, and treatment was started with steroid boluses, plasmapheresis, and intravenous human non-specific immunoglobulin. The Luminex® technique did not show any evidence of donor-specific antibodies (DSA), therefore the testing was broadened to rule out other secondary TMAs. The existence of anti-cardiolipin IgG and anti-beta-2-glycoprotein IgG antibodies was observed. When her reference hospital was contacted, a prior determination of positive antiphospholipid antibodies was found. Taking into account that the patient had two late miscarriages and two positive antiphospholipid antibody determinations, a diagnosis of primary APS was reached. With the diagnosis and given the negative DSA result, the biopsy findings were reinterpreted as TMA secondary to relapsed APS. Given the relapsed APS and the poor clinical evolution despite being correctly anticoagulated, treatment was started with eculizumab on the 17 PTD. Four days later the urine output increased, and by the 28 PTD kidney function improved (Fig. 2), achieving a sCr level of 1.9mg/dL. After three months of treatment, the treatment with eculizumab was suspended, with no evidence of subsequent APS relapse, and the patient continued to have stable kidney function with sCr 2mg/dL.
Given the finding of TMA on a kidney biopsy from a recent transplant, the first diagnosis to be considered is AHR, especially in hyperimmunised patients, although other causes of TMA should be ruled out to confirm the diagnosis. In our case, despite the absence of DSA, the presence of TMA and positive results for C4d in the peritubular capillaries were sufficient to establish the diagnosis of AHR according to the latest Banff classification.3 However, testing revealed positive antiphospholipid antibodies which, together with the previous determination and the patient“s history, enabled relapsed APS to be diagnosed.4–6 Regarding the presence of a C4d deposit on the kidney biopsy, the activation of the complement“s classical pathway in APS with secondary TMA justifies it.
Treatment for APS consists of permanent anticoagulation, but some aggressive cases may not respond. In the literature, a good response to eculizumab has been reported, with recovery of kidney function, resolution of the TMA lesions, and disappearance of the C4d and C5b9 deposits.2,7 Other authors have used eculizumab to prevent APS relapses in kidney transplant patients with good results.8,9 Our patient presented a good response to treatment with eculizumab, with no signs of relapse after it was suspended.
Our case illustrates the importance of a broad differential diagnosis in transplant patients who present with TMA on the kidney biopsy. Moreover, it makes clear that eculizumab is a therapeutic option for treating APS relapses, and it may not be necessary to maintain the treatment indefinitely, as occurs in other causes of secondary TMA.10
Please cite this article as: Bada-Bosch T, et al. Microangiopatía trombótica como recidiva de síndrome antifosfolípido en trasplante renal. Nefrologia. 2020;40:108–110.