Kidney transplantation from living donor is an established treatment in Spain since the 60s but has maintained a low level of activity until 2000, when the number of procedures and hospitals that perform this therapy experienced a gradual increase, reaching the highest figure in our history in 2009, with 235 living donor kidney transplants (which represents 10% of renal transplant activity). The reasons why living donor kidney transplantation is emerging in our country are diverse and can be focused in four main areas. 1) Better outcomes obtained when using living donors for kidney transplantation than those obtained with kidneys from deceased donors. Younger recipients with better HLA matching, the good health of the donor, the absence of any damages that occur in the kidney secondary to brain death, the small ischemic time and the possibility of preemptive transplantation can explain the best graft and patient survival. 2) The scarcity of sources: the relaxation of entry criteria on the waiting list implies an increasing challenge of the demand for transplant without the contribution of living donor kidney transplantation, especially in young recipients where the chances of obtaining an age-appropriate deceased donor are lower, due to the change in the profile of the deceased donor (increasingly older). 3) Improvement in the safety of the donor: the excellent evaluation and monitoring of donors (based on international standards) plus the use of less invasive surgical techniques are related to a low complication rate and to survival expectancies of living donors being similar to those of the general population. 4) Barriers overcome: The training effort by the transplant teams, hospital and regional coordinations, and the National Transplant Organization is giving excellent results, visible in the gradual increase in the number of hospitals with a program of living donor kidney transplantation and its activity. In addition, desensitization programs and the national cross-over kidney transplantation program have removed barriers to transplantation in cases of ABO incompatibility or positive crossmatch.
El trasplante renal de donante vivo es un tratamiento establecido en España desde los años sesenta, pero ha mantenido unos escasos niveles de actividad hasta el año 2000, fecha en que comienza un incremento progresivo en el número de procedimientos y de hospitales que realizan esta terapia, alcanzando en el año 2009 la cifra más alta de nuestra historia, con 235 trasplantes renales de donante vivo (que suponen un 10% de la actividad de trasplante renal). Los motivos por los que el trasplante renal de donante vivo está emergiendo en nuestro país son diversos y pueden englobarse en cuatro grandes apartados: 1) Mejores resultados que el trasplante renal de donante fallecido. Receptores más jóvenes con una mejor compatibilidad HLA, el buen estado de salud del donante, la ausencia de los posibles daños que se producen en el riñón secundariamente a la muerte encefálica, el menor tiempo de isquemia y la posibilidad de realizar el trasplante anticipado explican la mejor supervivencia de injerto y de paciente. 2) Necesidad de trasplante de vivo: la flexibilización de criterios de entrada en lista de espera conlleva una mayor dificultad de atender a la demanda de trasplante sin ayuda del trasplante renal de donante vivo, sobre todo en receptores jóvenes en los que las posibilidades de obtener un órgano adecuado a su edad son menores, debido al cambio en el perfil de los donantes fallecidos (cada vez de mayor edad). 3) Mejora en la seguridad del donante: la excelente evaluación y seguimiento de los donantes (basada en estándares internacionales), además de la utilización de técnicas quirúrgicas menos invasivas, conlleva un bajo índice de complicaciones y una esperanza de vida de los donantes similar a la de la población general. 4) Obstáculos superados: el esfuerzo en formación realizado por los equipos de trasplante, coordinaciones hospitalarias, autonómicas y la Organización Nacional de Trasplantes (ONT) está dando excelentes resultados, visibles en el progresivo aumento en el número de hospitales con programa de trasplante renal de donante vivo y en su actividad. Por otra parte, los programas de desensibilización y el programa nacional de donación renal cruzada han eliminado las barreras al trasplante en los casos de incompatibilidad ABO o prueba cruzada positiva.
INTRODUCTION
The first successful kidney transplant took place in 1954 and was performed in Boston’s Peter Bent Brigham Hospital by Merril and Murray’s medical team.1 This was a living-donor kidney transplantation carried out between identical twins. This, therefore, removed the main obstacle that had hindered previous attempts at kidney transplantation: the activation of the immune system and immediate graft failure due to alloantigen-dependent factors. This first transplant was the start of a new stage in the history of organ transplantation in which the donor was a living being, initially with a genetic relationship with the recipient. The advances in immunosuppression over time meant that transplants could be carried out between people who were not genetically related. At the same time, the discovery and general acceptance of the concept of brain death gave rise to a second stage when deceased-donor kidney transplantation predominated, although there were clear differences depending on the geographical area.
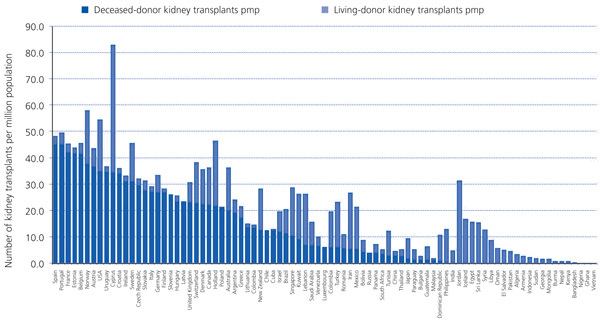
In countries that have developed a deceased-donor system, living-donor kidney transplantation has reappeared in the last few years as a complementary procedure when trying to increase the number of kidneys available for transplantation. In contrast, in countries where a deceased-donor system has not been developed, whether for cultural, religious, health and/or even socioeconomic reasons, kidney transplantation has been mainly or exclusively based on living donations. Figure 1 shows the differences in living-donor and deceased-donor kidney transplantation in 85 countries in terms of procedures per million population (pmp).23
LIVING-DONOR KIDNEY TRANSPLANTATION IN SPAIN
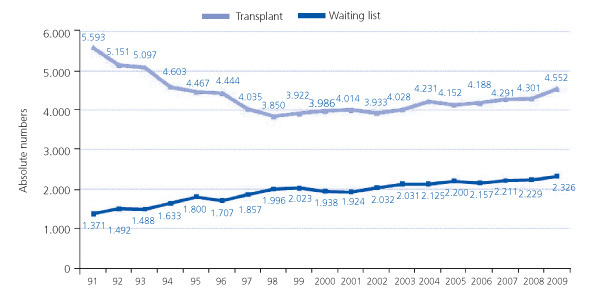
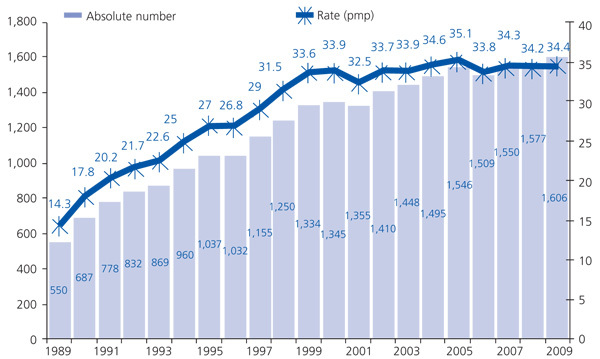
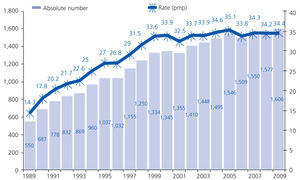
The evolution of living-donor kidney transplantation can only be understood by looking at the evolution of deceased-donor kidney transplantation. In 1989, the Spanish National Transplant Organisation (ONT) was created and organisational measures were implemented. These included creating a network of coordinators which turned out to be indispensable in identifying potential donors and converting them into actual donors.4,5 This led to a substantial increase in donations from deceased patients in Spain that reached unprecedented levels in the world. This has remained above 30 donor pmp in the last few years (Figure 2).6 At the same time, transplantation in general and kidney transplantation in particular have also increased. These have reached levels of more than 45 transplant procedures pmp in the last decade (Figure 3).6
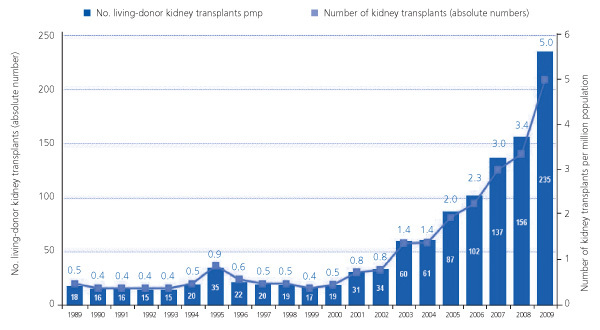
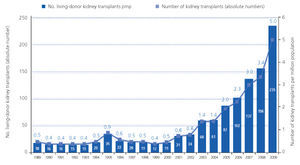
The progressive increase in deceased-donor transplants, along with the reluctance to submit a healthy person to a surgical procedure7 and the lack of understanding of the need for transplant organs, has limited living-donor kidney transplants to a small number of procedures, performed mainly in specialised hospitals with extensive experience. As a result, 1-2 living-donor transplants pmp were carried out in Spain during the 1990s. This constituted about 1% of all kidney transplants in Spain (Figure 4).6
However, the situation changed since the year 2000, when living-donor kidney transplantations started to increase progressively (Figure 4). In 2009 it reached record levels, with 235 procedures performed (5 pmp), i.e., 10.1% of all kidney transplantations in Spain.6 This significant increase in the number of transplants is based on a series of events that helped bring about a progressive change in the attitude of the Spanish system towards living-donor kidney donation: the excellent results achieved with this type of transplantation, the difficulty of meeting the needs of the Spanish population for kidney transplantations, demographic changes and changes in the comorbidity of deceased donors, and a substantial improvement in the safety of the procedure for the donor.
Excellent living-donor kidney transplantation results
Living-donor kidney transplantation is linked to better results than deceased-donor kidney transplantation, whatever the genetic relationship is between the donor and the recipient. Progress includes improvements not only in terms of graft survival, but also in patient survival. Data from the Organ Procurement Transplant Network shows that there is a 79.7% kidney graft survival rate at 5 years for living-donor recipients, compared to 66.5% for deceased-donor recipients, and a 90.1% patient survival rate vs 81.9%.8 The Collaborative Transplant Study data show very similar results to those of the American register.9
There are various reasons that explain the improved results of this treatment. The recipients are usually younger and are closely HLA-matched with the donor, as they are often genetically related. The donor has to undergo a series of extensive medical tests before being accepted and they are usually in perfect health, with obviously less associated pathologies than in the case of deceased donors. The absence of brain death and its pathophysiological factors mean that the graft has improved morphofunctional characteristics. Furthermore, the recipient can undergo immunosuppressive treatment in advance as it is a scheduled operation and the organ is submitted to a shorter cold ischaemia time than in the case of deceased donations. Lastly, another factor that has been proven to have a bearing on the improved results of living-donor transplantation is that it can be performed early, before the patient starts dialysis, according to a study carried out with data from the Catalonian Renal Patient Register.16 It is important to mention that the amount of time spent on dialysis has been identified repeatedly as a negative factor associated with graft and patient survival, regardless of the aetiology of chronic renal failure. This negative impact can start to be seen after 6 months on replacement treatment.11
The need for kidney transplantation
Although more kidney transplantations are being performed in Spain, the number of patients on the transplant waiting list has not dropped proportionally. There is a delicate balance between supply and demand of organs for transplantation. Thus, when there are more donations and transplantations, the criteria for including patients on the waiting list are more flexible and the demand for transplantations increases.
According to data from the Spanish Registry of Renal Patients the prevalence of end-stage kidney disease in dialysis treatment (haemodialysis or peritoneal dialysis) is 415 pmp.12 If we take into account that 22% of these patients are candidates for kidney transplantation, we discover that we need around 100 kidney transplants pmp to cover these needs, i.e., more than twice the number of transplant operations performed per year.
There are ways to increase the number of deceased donations as can be seen from the results of our Quality Control Programme. This detects the number of potential donors lost in ICU due to the patients not being identified, problems preserving the organ, refusal to donate, and, above all, because of medical contraindications.13 Furthermore, the early detection of patients outside the ICU that may progress to brain death can be improved. We must work in close collaboration with the units, departments, and specialities involved in treating the neurocritical patient.14 The number of organ transplants and kidney transplants in particular can be increased by creating new non-heart-beating donation programmes and the widespread use of organs from expanded criteria donors.15
Nevertheless, in spite of all the above mentioned measures, it is difficult to achieve the estimated necessary amount of kidney transplants without complementing it with living-donor kidney transplants.
Change in the profile of organ donors
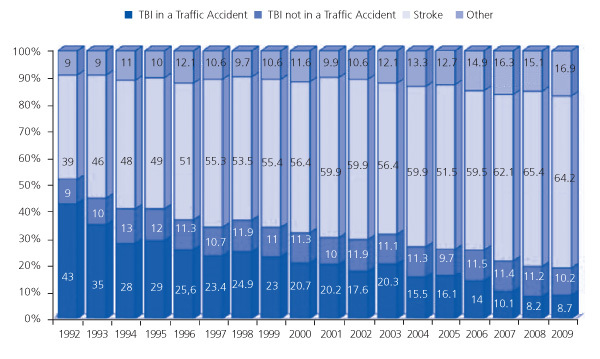
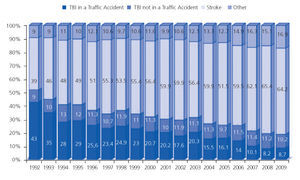
In Spain, the shortage of organs for transplantation continues due to epidemics and health care crises that have an effect both on our potential to donate (at least in terms of brain death), and the profile of organ donors. More aggressive treatments are being used to treat neurocritical patients (for example, decompressive craniectomy), which seems to decrease the mortality associated with this pathology. Furthermore, over the years there has luckily been a massive drop in traffic accidents as new legislative measures have been implemented to improve road safety.14 Faced with this prospect, if our donation and transplant system had kept the same criteria when accepting a deceased person as an organ donor, donation and transplantation would have dropped dramatically in Spain. In contrast, both the coordination network and surgical teams have progressively increased the number of organs accepted from elderly donors and their subsequent use to try and adapt to this situation and maintain our level of transplantation (and even increase it). These donors have normally died of strokes and not in road accidents (Figure 5). Compared to many European countries, our system stands out for the very high number of transplants using organs from elderly donors, through an unofficial, but existent, policy of “old for old”. The top priority of this policy is the suitability of age between the donor and recipient and not their immunological compatibility.17 This situation makes it easier to carry out transplantations on elderly recipients. In contrast, the large drop in young donors in Spain means that it is harder to carry out transplants on young recipients with advanced kidney disease and/or on dialysis. This is the population group that would most obviously benefit from living-donor kidney transplantation.
It is also important to mention that the drop in young donors has an effect on the availability of other types of organs as well, including pancreas. Simultaneous pancreas-kidney transplantation has now become a very sensitive procedure for various reasons. In short, it is not only diabetic patients that are competing for the pancreas-kidney transplant but also young recipients with the aforementioned problems to find an appropriate donor in terms of age, and especially in hyperimmunised patients. Living-donor kidney transplantation could help solve this situation, with the possibility of implanting the pancreas on its own.
Improvement in living donor safety
Performing a nephrectomy on healthy patients is not a harmless procedure, although it is seen as relatively low risk surgery these days. As a result, the risk of immediate death linked to living-donor kidney donation is estimated at 0.03%.18,19 The probability of complications in the short term, such as haemorrhage or infection, is also low. However, this does vary depending on the type of procedure used to perform the nephrectomy on the donor (between 0.6% and 14%). The use of laparoscopic nephrectomy has improved considerably the immediate postoperative recovery, with donors recovering and returning to work faster.20 In the long term, living-donor-related death does not seem to be higher than that of the general population when adjusted for age and associated comorbidity.18 The living donors’ health condition is also similar and the repercussions of donation seem to have minimal effects on kidney function, albuminuria and blood pressure levels.21 Furthermore, studies show that the long-term quality of life of living donors is similar to that of the general population and in some cases they have a higher quality of life. This is due to the fact that the satisfaction they have for helping someone is added to their general situation.22-24
Although current knowledge has meant that living-donor kidney transplantation has been reconsidered in Spain and in other countries and has been welcomed and accepted by doctors, it must be acknowledged that living donors need to be systematically monitored over time. Therefore, one of the main challenges linked to this therapeutic procedure is the need to create tools to be able to monitor living donors. This has even been included as one of the obligations of the Directive of the European Parliament and of the Council on standards of quality and safety of human organs intended for transplantation.25
LIVING DONOR KIDNEY TRANSPLANTATION AND INTERNATIONAL STANDARDS
Due to the fact that not enough organs are available for transplantation and that wealth is not shared equally throughout the world, ethical questions must be addressed with regard to selecting the donor, assessing the reasons for donating, the possibility of marketing organs and other aspects regarding the medical, psychological and social evaluation and perioperative and postoperative care of the living donor. This has meant that living donation has been standardised in the different legal instruments available internationally, such as the Council of Europe’s Convention on Human Rights and Biomedicine26 and its Additional Protocol concerning donation and organ transplantation27 and the WHO Guiding Principles on Human Organ Transplantation. These instruments are crucial when developing national laws. It cannot be denied that these legal documents all agree on a series of basic principles regarding organ donation. These include the need to obtain free, explicit and informed consent for donation, banning human organ trade, the need to carry out appropriate donor selection and investigations to assess the medical, psychological and social risks to the donor and the need to care for and monitor the donor after the procedure. On this subject, it is worth mentioning the criteria set out in international consensus documents such as those in the Amsterdam Forum,17,29 in the case of living kidney donation and the Vancouver Forum30,31 for living lung, liver, pancreas, and intestine donor.
Although these basic principles have not changed over time, these institutions have changed their stance on the role of living donation, as has occurred in Spain.
BARRIERS AND SOLUTIONS TO INCREASING LIVING-DONOR KIDNEY TRANSPLANTATION IN SPAIN
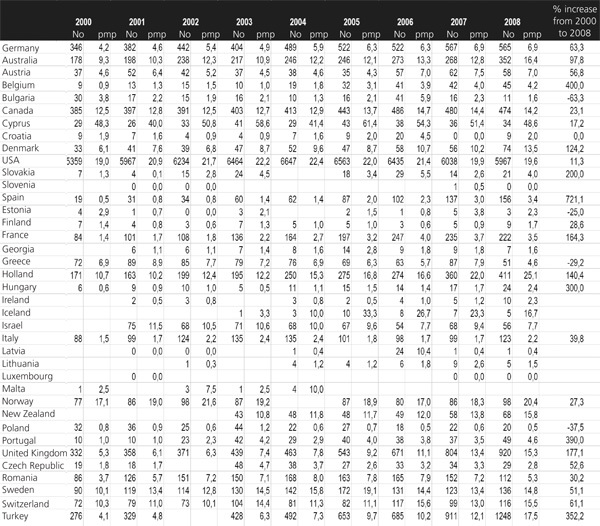
Despite a progressive increase in living-donor kidney transplantation in Spain, barriers are still identified that prevent it from increasing even further or it may be more apt to say that they hamper greater equality between hospitals and the Autonomous Regional Governments. In any case, and including Spanish outcomes, Table 1 highlights how far living-donor kidney transplantation has evolved over the last few years in countries surrounding Spain or with similar socio-demographic and economic characteristics. Evolution is certainly irregular, but in general terms, countries that do not perform many transplants have increasingly been performing more. The activity of Northern European countries stands out and it is interesting to note that in the USA a small drop in activity in the last few years has made the Americans analyse their systems.32
Lack of experience of some kidney transplant teams
Laparoscopic nephrectomy or minimally-invasive procedures have become increasingly recognised as the international reference and this has held back the development of living-donor transplantation in some hospitals that do not have enough experience in this type of surgical approach. It is true that we have to promote the development of these new types of surgical approaches, but not having developed them must not be a barrier to living-donor transplantation, as may be happening at the moment. These new approaches should be seen as an improvement to traditional approaches and doctors should always be suitably informed on the existing options offered to potential donors and recipients. They may not only lack experience in the surgical aspects of donating, but also in informing the recipients and their family members on this therapeutic alternative, assessing the donor and setting safe donation limits, evaluating the psychological and social aspects, the post-donation follow-up, etc. This type of training is essential.
One of the actions that has been established in Spain recently is the development of training courses. The most important events are the Reunión Internacional de Donante Vivo Hepático y Renal (International Conference on living liver and kidney donations) which has been annually organised by the Clinic i Provincial Hospital of Barcelona since 2002, and the course organised by the Spanish National Transplant Organisation (ONT) and by one of the most active centres in living-donor kidney transplantation in Spain, the Puigvert Foundation team from Barcelona. This course has been running for four years now, and this year it is aimed at hospitals that have recently implemented or plan to introduce a living-kidney transplantation programme, nephrologists who work in advanced kidney disease and dialysis units. Attendance from these hospitals has been envisaged in such a way that doctors from different units take part, including nephrologists, urologists, and transplant coordinators who may participate in this process (and in fact participate at some hospitals) from an informative, evaluative and logistical point of view.
The need to get through to doctors efficiently is one of the reasons why the Spanish Society of Nephrology (SEN) and the ONT have decided to develop these Guidelines on living-donor kidney transplantation.
Living-donor transplantation is not indicated enough
Living-donor transplantation is also limited by the fact that doctors do not indicate it or do not offer it as an additional therapeutic option to patients with advanced kidney disease, preferably before starting dialysis.33 As a result, there were five living-donor kidney transplants pmp in Spain in 2009. However, the activity varied greatly depending on which Autonomous Community the recipient was from, from 0 pmp in some Autonomous Communities to almost 14 pmp in Catalonia.
The fact that living-donor transplantation is not routinely offered as a therapeutic option was confirmed in a survey carried out on dialysis patients in 2004: 59% stated that they had not received any information on this type of transplantation and 83.4% claimed that their medical team did not inform them about this therapeutic option.34 The current situation may be entirely different, but the variability described above highlights the need to encourage nephrologists to offer this as another option so that patients and their relatives can make an informed decision.
Various activities have recently been developed to improve the communication between doctors and patients, such as information documents that may be useful to doctors that look after advanced kidney disease patients. Transplant doctors, patient associations, hospital and autonomous transplant coordinators and the ONT have actively participated in drawing up these documents. In the last year, ALCER, ONT and other regional organisations have organised meetings between patients and doctors aimed at informing the patients and promoting dialogue and communication with the health professionals that look after them.
ABO incompatibility and positive crossmatch between potential donors and recipients
The barriers are completely different when we look at the units that perform a high number of living-donor kidney transplants. According to the data provided by one of the most active teams in Spain, up to 30% of people assessed as potential living donors are rejected during the process due to ABO incompatibility or a positive crossmatch. The estimated situation in the USA is similar, where 36% people have an ABO incompatibility with another from their population35 and 30% of patients on the waiting list for kidney transplantation are sensitised to HLA antigens.36 There are two ways to solve this situation: one is drug-based and the other is organisational. The first is based on a desensitisation therapy, which is already being used by some medical teams in Spain. Twelve ABO-incompatible living-donor kidney transplants could be performed in the last two years thanks to this therapy.
The organisational option is based on what has been called cross-over donation or kidney paired exchange, conceived by Rapaport in 1986. His idea consists in that if a potential donor of a pair X is incompatible with his/her potential recipient, but compatible with the recipient of a second pair Y, who is incompatible with his/her donor, and vice versa, the situation may be solved by swapping the donors (or kidneys).37 This cross-over kidney transplantation procedure was not put into practice until 1991, in South Korea.38 As the years passed, national and regional programmes have been developed in other countries such as the USA, Holland and the UK. These programmes, which have become more sophisticated over the years, have contributed to increase living organ donations in these countries.39-41 This sophistication goes from developing IT software for an optimised selection of pairs for exchanging organs/donors to combining the programme with altruistic donation. This programme has been able to benefit more people and have had a knock-on effect on waiting lists for deceased donors. Cross-over kidney transplantation has its advantages and disadvantages compared to using desensitisation protocols: it is cheaper and less aggressive for the recipient, but it is logistically more complex. The emotional aspect linked to direct kidney donation is also lost.
After a discussion process and approval by the transplant committee of the interterritorial council, the idea to set up a programme of this type on a national level became a reality in Spain and was developed by an ad hoc committee of experts chosen by the ONT. The programme, which has already been developed, consists of three main elements: a network of hospitals that take part in the programme (hospitals have to join it formally and it is verified beforehand that they comply with a series of previously agreed criteria), a national register of donor-recipient pairs that might participate in the programme, and an action protocol subject to continuous evaluation. The protocol sets out the selection criteria for pairs, how the assessment of the exchange possibilities works, the selection and prioritisation criteria for pairs, the procedure, and the post-donation and post-transplant follow-up. The first two crossover kidney transplants took place in Spain in June 2009. The two hospitals that took part were the Clinic i Provincial Hospital of Barcelona and the Virgen de las Nieves Hospital of Granada. The problem for both pairs was a positive crossmatch due to sensitisation to donor antigens. The operations were a success and they opened the door for a new stage in living-donor kidney transplantation in Spain, where new actions, such as ‘Good Samaritan’ donation, have already started. These are expected to report good results in the short term.
Figure 1. 2008 deceased-donor and living-donor kidney transplants (procedures pmp)
Figure 2. Number of deceased-donor organ donations (absolute number and pmp) in Spain, 1989-2009
Figure 3. Number of kidney transplants and patients on the waiting list on 31 December in Spain (absolute numbers), 1991-2009
Figure 4. Number of living-donor kidney transplants in Spain (absolute numbers and pmp), 1989-2009.
Figure 5. Causes of organ donor death in Spain, 1992-2009
Table 1. Evolution of the number of living-donor kidney transplants (absolute numbers and procedures pmp) in different countries, 2000-2008.