To the Editor,
Peritoneal dialysis (PD) is an increasingly frequent therapeutic option for advanced chronic kidney disease. However, this technique is not exempt from complications, the most common being peritonitis. Although you may also observe infections in the exit site of the peritoneal catheter, infection of the subcutaneous tunnel, hernias, abdominal or lumbar pain, haemoperitoneum, chylothorax, pleuroperitoneal communication or hydrothorax, among others.
The infusion of fluid in the peritoneal cavity increases intraabdominal pressure, which may cause the peritoneal fluid to flow into the chest, leading to pleuroperitoneal communication. Cases of pleuroperitoneal communication secondary to peritonitis have also been described.1.2.
We present the case of a 77-year-old male with chronic kidney disease, probably secondary to nephroangiosclerosis, who was on continuous ambulatory PD for 15 days. On the 8th day, the patient had an episode of peritonitis, caused by Streptococcus (viridansgroup) and was treated according to protocol with ciprofloxacin and vancomycin. The patient went to the emergency department reporting dyspnoea, fever and coughing for 24 hours, along with a deficit of ultrafiltration in recent days.
The examination showed revealed a general poor health status accompanied by tachypnoea and bilateral hypoventilation, more pronounced in the right pulmonary area.
A chest x-ray showed a moderate right pleural effusion, which was mild on the left side.
Treatment was started with empirical antibiotics for respiratory infection, reducing the febrile syndrome while the dyspnoea continued.
Therapeutic and diagnostic thoracentesis was performed, with transudate characteristics. We found greater glucose in pleural fluid than in plasma. Dyspnoea improved and peritoneal fluid was cultured, showing negative results.
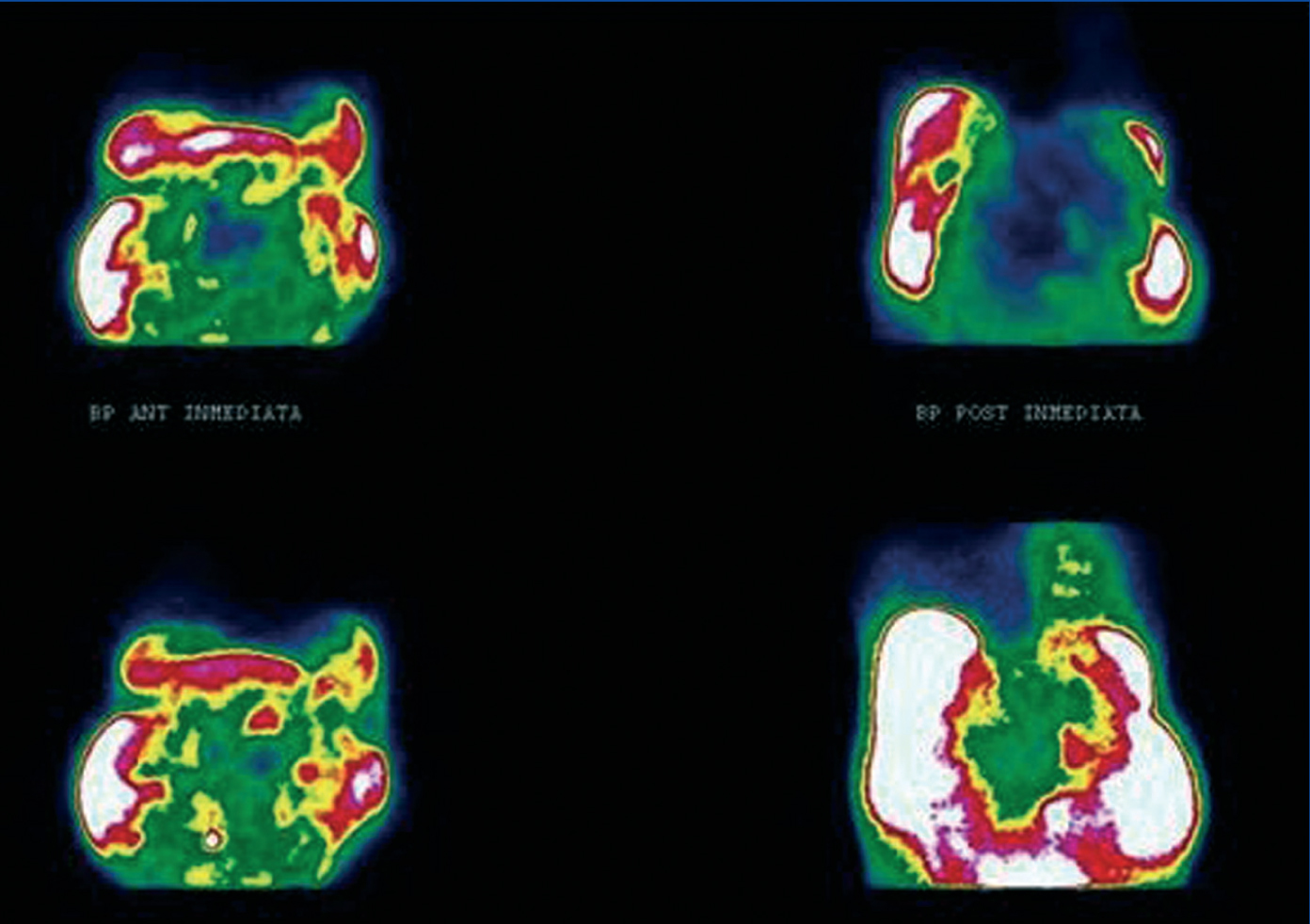
Given the suspicion of pleuroperitoneal communication, an isotopic peritoneogram with 99mTc-MAA was performed. The presence of the radiotracer activity at the right hemithorax suggested the existence of pleuroperitoneal communication in this hemithorax (Figure).
Having confirmed the diagnosis of pleuroperitoneal communication, it was decided to temporarily suspend PD and the patient was transferred to haemodialysis.
DISCUSSION
Patients on PD may present technique-related complications, the most frequent being peritonitis, catheter-related infections, hernias; and among the less frequent ones is pleuroperitoneal communication.2.3 This occurs by congenital or acquired diaphragmatic defects, due to an increase in intra-abdominal pressure when instilling peritoneal fluid. This can also be associated, in some cases, with peritonitis episodes.1 Its incidence rate ranges between 1.6% and 2%, although it is believed to be greater in some cohorts. It is more frequent in women and on the right-hand side. Our patient is a male who presented right pleuroperitoneal communication, and whose diagnosis was reached due to the clinical suspicion in the presence of dyspnoea, hypoventilation, and decreased ultrafiltration.2
Chest x-ray revealed pleural effusion. The thoracentesis showed a liquid with characteristics of fluid transudate, and the concentration of glucose in pleural fluid was greater than in plasma.2.3
The isotopic peritoneogram with 99mTc-MAA, showing pleuroperitoneal communication, was very useful for confirming the diagnosis.4
Before diagnosis other causes of dyspnoea should be ruled out, such as salt retention, heart failure, hypoproteinaemia, infections or neoplasias.3
Treatment consists of the final or temporary cessation of PD, with peritoneal rest and transition to haemodialysis. In some cases where the patient maintains residual diuresis, you may continue automated PD (APD) at low volumes or APD at low volumes with dry day. In some occasions, it is necessary to perform pleurodesis, either chemical (tetracycline), surgical or with the patient's blood.5
In our case, the decision was peritoneal rest with temporary transition to haemodialysis.
In some cases, treatment does not deliver good results, giving rise to the abandonment of the technique (PD) and the final transition to haemodialysis.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the contents of this article.
Figure 1. Peritoneal scintigraphy with 99mTc-MAA