Desde que se implementó por primera vez, la peritonitis ha sido la complicación más común de la diálisis peritoneal ambulatoria continua (DPAC) y sigue siendo la causa principal del fracaso del tratamiento y del cambio a otros tratamientos renales sustitutivos. En este estudio se presenta una serie colombiana de un total de 2469 episodios de peritonitis en 914 pacientes de una cohorte de 1497 pacientes en diálisis peritoneal (DP), que fueron sometidos a seguimiento durante casi tres décadas en un único centro. Se trata de la mayor serie de Latinoamérica de pacientes con peritonitis asociada con DP. Objetivo: Describir la peritonitis asociada con la DPAC en una cohorte de pacientes sometidos a seguimiento durante 27 años en un único centro y comparar los resultados con los observados en otras partes del mundo. Diseño del estudio: Estudio prospectivo de pacientes incidentes de DPAC desde marzo de 1981 hasta diciembre de 2008. Resultados: En nuestro centro, la tasa de peritonitis ha permanecido estable entre 0,8 y 0,9 desde 1981 y no se han observado cambios significativos en los 27 años de seguimiento. La tasa es similar a la descrita actualmente por otros grandes centros de diálisis del mundo, que han registrado importantes mejoras en las últimas décadas. No se detectaron diferencias significativas en las muestras aisladas de microorganismos gram positivos o gram negativos u hongos en lo que respecta a los registrados en otras grandes series ni en la frecuencia de peritonitis con cultivo negativo. Conclusión: En este estudio se presenta la mayor serie de Latinoamérica de pacientes con peritonitis asociada con DPAC con un total de 2469 pacientes. La tasa de peritonitis asociada con DPAC permaneció prácticamente inalterable durante las tres décadas de observación, a pesar de haber utilizado tres sistemas diferentes de DPAC. Nuestra hipótesis es que las condiciones socioeconómicas de los pacientes ingresados para diálisis peritoneal influyen en la tasa de peritonitis.
Peritonitis has been the most common complication of continues ambulatory peritoneal dialysis (CAPD) since it was first implemented, and it remains the leading cause of treatment failure and transfer to other renal replacement therapies. This study presents a Colombian series with a total of 2,469 episodes of peritonitis in 914 patients from a cohort of 1,497 patients on PD, who were followed for almost three decades at a single center. This is the largest Latin American series of patients with PD-related peritonitis. Objective: To describe the CAPD-related peritonitis in a cohort of patients followed for 27 years at a single center, and compare the results with those observed elsewhere in the world. Study Design: Prospective study of incident patients on CAPD from March 1981 to December 2008. Results: In our center, the rate of peritonitis has been steady between 0.8 and 0.9 since 1981 and no significant changes have been noticed in the 27 years of follow up. The rate remains similar to that described nowadays by other large dialysis centers in the world, which have reported significant improvements in recent decades. No significant differences were found in the isolates of gram-positive and gram-negative microorganisms or fungi with respect to those reported by other large series, or in the frequency of culture-negative peritonitis. Conclusion: This study presents the largest Latin American series of patients with CAPD-related peritonitis with a total of 2,469 patients. In this study, the rate of CAPD-related peritonitis remained almost the same during the three decades of observation despite having used three different CAPD systems. Our hypothesis is that the socio-economic conditions of the patients admitted for peritoneal dialysis influences the rate of peritonitis.
INTRODUCTION
Peritoneal dialysis (PD) is a method that replaces kidney function based on the principles of conductive and convective transport through the peritoneal membrane. Despite technical improvements, peritonitis remains the main cause of technique failure, catheter loss and need to transfer to other forms of renal replacement therapy.1,2 Peritonitis causes disability, work absenteeism and in some cases the need for hospitalization.3 In addition, patients with frequent episodes of peritonitis have a higher risk of death independently of other factors.4 The incidence of PD-related peritonitis varies among different dialysis centers and periods of time.5-10 Since the procedure was first implemented more than three decades ago, there have been several changes in the PD systems that appear to have modified the incidence of peritonitis. Improvements in the connection systems have yielded the greatest impact as reported in large series around the world.11-17
CAPD was introduced in Latin America in the early 1980s, and also in this region there has been a reduction in the incidence of peritonitis, which is directly, associated with the emergence of safe connection systems.15,18-21 In Colombia the Hospital Universitario San Vicente de Paúl was the first hospital to implement this variety of renal replacement therapy. This medical center is located in the second largest city in the country and is the main referral center for an extensive region. Three different connection systems have been used since the beginning of the PD program and over 1,400 patients have been under PD in this hospital. Despite the widespread use of this form of dialysis in Colombia, there are few data regarding CAPD-related peritonitis22,23 and reporting our experience is essential as part of a continuous quality improvement program.
OBJECTIVES
The aims of this study were to describe the rate of CAPD-related peritonitis in a cohort of patients treated in a university hospital, and to compare the results with those observed elsewhere in Latin America and the world; as well as to describe the prevalence, microbiological characteristics, treatment outcome and peritonitis-free survival with three different CAPD systems.
METHODS AND STUDY POPULATION
This is a prospective cohort study of patients treated at a single center, the Hospital Universitario San Vicente de Paúl. This is a university hospital and a referral center for a population of almost 5 million people. The PD program began in 1981 and since then it keeps detailed follow-up of patients who have belonged to it. In these three decades three different PD systems have been used: The standard (Baxter) method between 1981 and 199;24 the twin-bag disconnecting systems (Fresenius Medical Care) between 1997 and 2002,25 and the Stay-safe ANDY disk (Fresenius Medical Care) system from 2002 to 200826 years in which these systems came to Colombia. The standard method consists of a bag of dialysate which is punctured with a pin covered with gauze impregnated with iodopovidone (povidoneiodine), after entering the liquid into the peritoneal cavity the transfer line is sealed and then stored in the patient's clothing without taking line; gravity drainage ocurred by placing the bag on the floor, when the drainage ends the bag is replaced by the aseptic technique and then the cycle gets repeated. The Twin-bag method consists of two bags, the first containing the dialysate liquid and the second bag is empty (for drainage), both are joined by a catheter; at the time of infusion the transfer line is closed, a five seconds wash with dialysate is conducted and then the catheter is opened to infuse fluid into the peritoneal cavity, at the end a clamp is placed onto the transference line separating the two bags. The third method, the Stay-safe ANDY consists of connecting the transfer line to a pin attached to a disc which has a knob with four positions to direct infusion and catheter drainage, once the cycle is completed an occlusive pin is placed upon the transfer line, the line is taken off the disc and a cap covered with yodopividona (povidoneiodine) is placed.
Patients have been switched from one system to the next during the three decades. All patients who enter the program are trained in the CAPD procedure for a week. Most patients have used the manual peritoneal dialysis, but since February 10 of 1992 is also provided automated peritoneal dialysis with Fresenius Medical Care cycler. The diagnosis of peritonitis is made according to already established criteria.27 Whenever it is possible, a sample is taken for cell count and culture before starting treatment. Empirical treatment is started with cephalothin plus an aminoglycoside antibiotic. The latter has varied from netilmicin during the first years of the program, to gentamicin, and then amikacin during these last 11 years. In cases of fungal peritonitis the antibiotic treatment is stopped and the peritoneal catheter removed. After knowing the causative microorganism, the treatment is given according to the antibiogram. If the peritonitis is caused by Pseudomonas aeruginosa, the catheter is always removed due to the high risk of re-infection.
The electronic records of the CAPD program from March 1981 to December 2008 were examined in order to develop the study. We included all patients over 15 years of age, but those with less than 30 days of follow-up were excluded. We performed a descriptive analysis using absolute distributions, percentages and summary measures. Statistical analyses were performed using Epidat version 3.1 and SPSS version 17. Chi-square tests of independence were used or Fisher's exact test when necessary, and patient survival was calculated using the Kaplan–Meier method. A p value of less than 0.05 was considered significant.
Although a patient may have used the three techniques for peritoneal dialysis at different points in time, the statistical analysis that was performed kept each technique independent.
Definitions
Criteria of peritonitis: cloudy peritoneal fluid, white cell count greater than 100 per mm3 (after a dwell time of at least 2 hours) with at least 50 polymorphonuclear neutrophilic cells.
Recurrence of peritonitis: An episode that occurs within 4 weeks of completion of therapy of a prior episode but with a different organism.
Relapse of peritonitis: An episode that occurs within 4 weeks of completion of therapy of a prior episode with the same organism or 1 sterile episode.
RESULTS
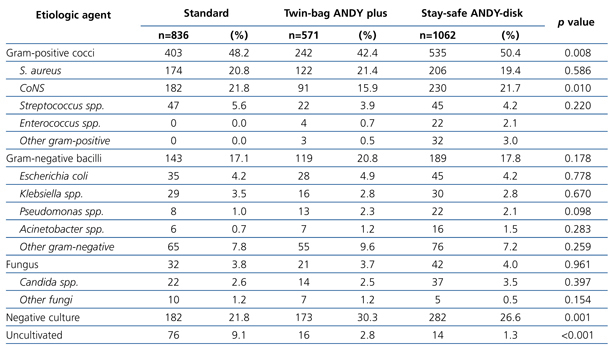
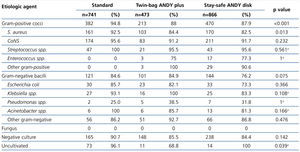
This study presents a Colombian series with a total of 2469 episodes of peritonitis in 914 patients from a cohort of 1,497 patients on CAPD, who were followed for almost three decades at a single center (between March 1981 and December 2008). 766 (51%) were females and 731 (49%) males, with a cumulative follow-up of 3,068 years. The mean follow-up was 28 months (range 1-195). The total number of patients was distributed as follows according to the CAPD systems: 443 patients in the standard system, 482 patients in the twin-bag system and 572 patients in the stay-safe ANDY disk system. The average age was 32±10 years in 1981 and 52±17 years in 2008. There were 2,469 episodes of peritonitis in 914 patients, which were distributed like this: 836 episodes for the standard system, 571 for the twin-bag system and 1,062 for stay-safe ANDY disk system. Microbiological isolation was obtained in 1,726 of the 2,469 episodes of peritonitis (Table 1), 637 episodes were culture negative and in 106 the culture was not taken because the patients had already started antibiotic treatment at the time of consultation since they lived in remote rural areas with poor access to health services. In 30 patients the episode of peritonitis was the cause of death (1.2% of all peritonitis). During the observation period died 259 patients (17.3%) from all causes.
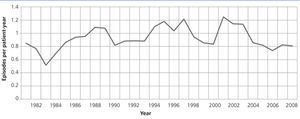
Episodes
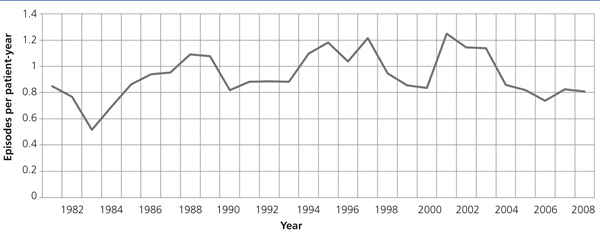
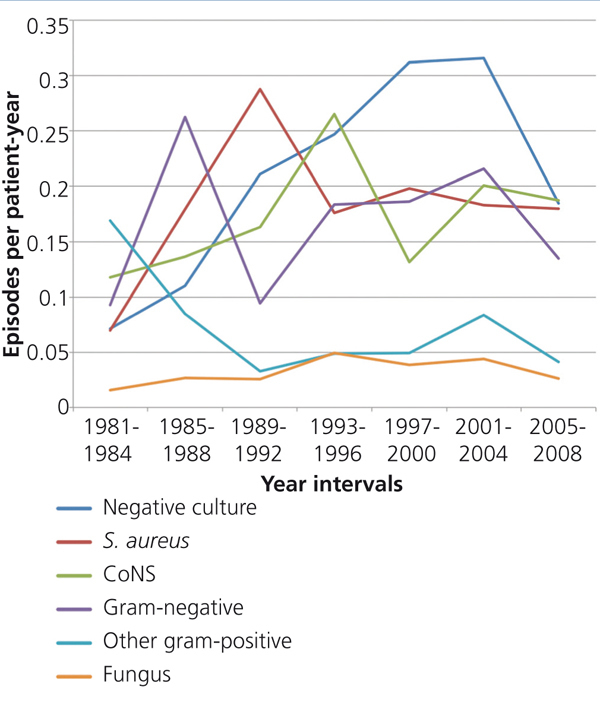
In general there were no significant changes in the 27 years of follow-up despite changes in the techniques of CAPD. The incidence of peritonitis was 0.84 episodes per patient-year in 1981 and 0.80 episodes per patient-year in 2008, the global rate of peritonitis was 0.9. The average rate of peritonitis observed using the standard technique was 0.90 episodes per patient-year; with the twin-bag ANDY plus technique 1.0 episodes per patient-year, and with the stay-safe ANDY-disk technique 0.90 episodes per patient-year (Figure 1).
Isolates
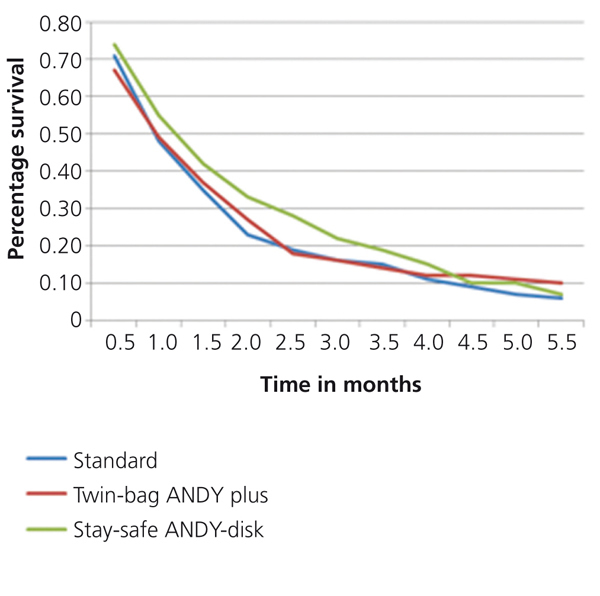
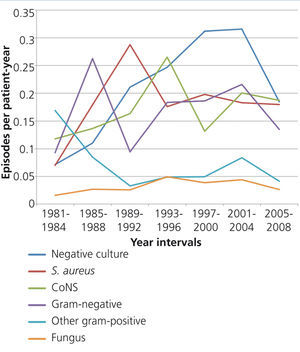
During the three periods of CAPD, gram-positive organisms were isolated more often (on average 48% of episodes), followed by gram-negative (on average 18% of episodes). Staphylococcus aureus and Coagulase-Negative Staphylococcus (CoNS) were the most commonly isolated gram-positive bacteria (Table 1). Gram-positive isolates were different in the three periods (p=.008). There were a lower percentage of gram-positive bacteria during the twin-bag ANDY-plus period compared to the standard (p=.023) and stay-safe ANDY disk periods (p=.002) (Figure 2). This difference was given by the proportion of isolates of CoNS which was significantly lower in the twin-bag ANDY-plus period compared to the standard (p=.006) and stay-safe ANDY disk periods (p=.005). No difference was found in the percentage of CoNS between the standard and stay-safe ANDY disk (p=.952) systems. Escherichia coli was the most frequently isolated gram-negative bacteria during the three decades (on average 4.4% of all episodes) without significant differences between techniques. There were also no differences among fungal isolates, which represented 3.8% of all episodes. On average, the percentage of culture-negative episodes was 25.8%, with a lower percentage during the standard PD period compared to the twin-bag ANDY-plus (p<.001) and stay-safe ANDY-disk (p=.015) periods. No difference was observed in culture-negative episodes between those on the twin-bag-ANDY plus or Stay-safe ANDY disk systems (p=.108). Uncultivated episodes decreased progressively and significantly between the three periods (p<.001), with significant differences between each of the techniques when compared to the others (p<.05 in all cases).
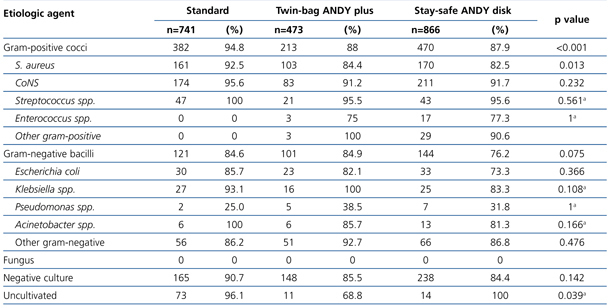
Cure
The average percentages for peritonitis cure while using the three techniques of CAPD were as follows: Standard 88%, twin-bag-ANDY-plus 82% and stay-safe ANDY-disk 81%. There was a significant difference in the cure rate of peritonitis by gram-positive cocci (p<.001), which was explained by episodes of peritonitis caused by S. aureus (Table 2). There was a higher cure rate for S. aureus peritonitis in the standard technique compared to the twin-bag ANDY-plus (p=.028) and the stay-safe ANDY-disk systems (p=.003), with no difference between the twin-bag-ANDY-plus and the stay-safe ANDY-disk (p=.654). The cure rate of uncultivated peritonitis was significantly lower in the twin-bag-ANDY plus compared to the standard (p=.003) and the stay-safe ANDY- disk (p=.044) systems, with no difference between these last two (p=1.000).
Relapse and recurrence of peritonitis
A total of 117 patients (4.7%) had relapsed and 101 patients (4%) had recurrence of peritonitis.
Survival
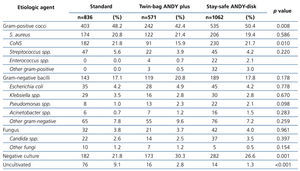
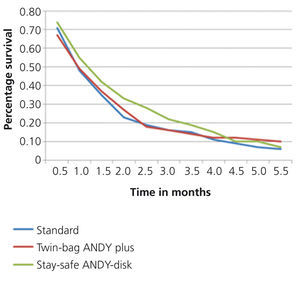
There were no statistically significant differences in peritonitis-free survival between the three techniques of CAPD (Figure 3).
Return to peritoneal dialysis
Of the 436 peritonitis unhealed in which the catheter was removed, only 110 patients (25.2%) were successfully returned to peritoneal dialysis; 50% of the patients refused to return to this mode of dialysis therapy and the other 25% was not possible due to intestinal adhesions that prevented the placement of a new peritoneal dialysis catheter.
DISCUSSION
Colombia is a developing country located in northwestern South America and has a population of 45 million inhabitants. In Colombia there are 22,000 people on dialysis, which 85% are on hemodialysis, and 15% in peritoneal dialysis. CAPD-related peritonitis is the most common acute complication of CAPD and it has been the main cause of technique failure over the years. This situation has led to technical improvements in CAPD systems and connectology which have significantly decreased peritonitis rates in randomized controlled trials11 as well as in reported long-term single-center experience.18,28 CAPD was introduced in Latin America in the late 1970s; the Hospital Universitario San Vicente de Paúl was the first center to perform this procedure in Colombia in 1981. This study presents the largest Latin American series of patients with CAPD-related peritonitis with a total of 2,469 episodes of peritonitis in 914 patients from a cohort of 1,497 patients followed for 27 years. There were no significant variations observed in the rate of peritonitis from 1981 to 2008. However, peritonitis rate has ranged 0.8-0.9 since the beginning of the program and it remains similar to that described today by other dialysis centers around the world that have reported significant improvements in recent decades.3,10 An Australian series with 2,073 episodes of peritonitis in 711 patients found a decrease from 6.5 episodes per patient-year to 0.35 episodes per patient-year over a period of 25 years.28 In Latin America, a large Brazilian study including 1,048 episodes of peritonitis in 680 patients reported an overall rate of peritonitis of 0.82 episodes per patient-year,18 very similar to the rate found in our study, however, the publication also reported a fairly significant reduction in peritonitis rate from 3.54 episodes per patient-year in the early 1980s to 0.74 episodes per patient-year in the first decade of 2000. Another Brazilian study also found a reduction in the rate of peritonitis from 1:10.5 patient-months between 1984 and 1994 to 1:20.6 patient-months after 1992 when the Y-set system was introduced.19 Figueiredo et al. also in Brazil, observed peritonitis rates close to 1:12 with the Y-set system, and rates of 1:21 patient-months when the Y-connector, ultrabag (Baxter), or ANDY Plus (Fresenius Medical Care) systems were used.20,21 Studies in other Latin American countries have also reported significant reductions in the incidence of peritonitis directly associated with the introduction of safe connection systems. In Mexico, Monteon et al. reported incidences of 1:6, 1:12 and 1:24 patients per month for the standard technique, Y-set and double bag systems respectively.15
Other countries have reported their experiences on the development of continuous ambulatory peritoneal dialysis and improvement in peritonitis rates over time.29-33 Contrasting with previous reports, in this study the rate of CAPD- related peritonitis remained almost the same during the three decades of observation despite having used three different CAPD systems. We have no clear explanation for this phenomenon, which so far has not been described in other major world series; however several factors could have influenced the situation. The change in the social security system in Colombia could have had a negative impact on the rate of peritonitis. At the beginning of the CAPD program the patients were carefully selected and diabetics, elderly patients, rural residents, illiteracy or patients in extreme poverty were not included. In the early 1990s with the implementation of a new social security system, access to renal replacement therapy was extended and since then the restrictions for entering the CAPD program are minimal. Now the program includes older patients (the mean age is 10 years more than when the program started in 1981), patients with more co-morbid disorders and social and economic difficulties like extreme poverty, illiteracy and patients living in areas distant from the dialysis center, all this has been associated in other studies to a higher risk of a first episode of peritonitis.34
In our country, CAPD became the form of renal replacement therapy most often used by individuals with geographical and economic barriers that render difficult for them to attend hemodialysis centers located in major cities. Other studies have shown a higher incidence of peritonitis in elderly patients35 and more clinical problems and a higher mortality rate in diabetics;36 a study in Hong Kong found that dependence on the social security system is associated with increased likelihood of developing peritonitis37 and in Brazil low-income and low educational level patients have a higher risk of peritonitis.38 The expansion in the coverage of the social security system has also dramatically increased the number of PD patients, which rose from 42 on average in 1980 to 260 in the first decade of 2000. This also modified the ratio of nurses per patient, which changed from 1:40 to 1:85. It has previously been shown that patient training methods influence the risk of CAPD infections,39-41 with patients on enhanced training having significantly fewer exit-site infections when compared to patients on standard training; however, in this study it was not possible to define the impact of specific changes in training methods.
As in other large series, gram-positive bacteria were the most commonly isolated organisms during the three CAPD periods (48% of isolates on average). In the Brazilian and Australian series, gram-positive bacteria were responsible for 54% and 53.9% of episodes, respectively.18,28 In our study, S. aureus and CoNS were the gram-positive bacteria most commonly isolated during the three decades (20.5% and 19.8% on average respectively). There was a significant decrease in the percentage of CoNS peritonitis with the twin-bag ANDY-plus system compared to the other two techniques. We did not observe changes in the incidence of peritonitis by S. aureus, as in other series in which the change in the incidence of this organism accounts for much of the improvement in the overall rate of peritonitis.18,28 In the Australian series CoNS became the most frequently isolated pathogen (28.2% of episodes of peritonitis)28 and in the Brazilian series S. epidermidis was the most often isolated organism in the first decade of 2000.18 A small Colombian study that analyzed 224 episodes of peritonitis in 146 patients found S. aureus in 11.2% of the episodes and S. epidermidis in 10.3% but in that study 48% of the cultures were negative.22 In other Latin American series analyzed in the mid-nineties S. aureus was the most common agent,19,42-44 but subsequent analysis have shown S. epidermidis to be the most common pathogen isolated.21,45,46
Gram-negative bacteria were isolated in 18% of all episodes of peritonitis, a finding similar to that previously reported elsewhere.6,18,28,47-50 Fungal peritonitis occurred in approximately 3.8% of all episodes, with Candida spp. being responsible for most cases. The overall incidence of fungal peritonitis has remained low since 1981; other authors have reported similar results.10,18,28,51 We observed a lower cure rate of peritonitis caused by S. aureus with the twin-bag ANDY-plus and stay-safe ANDY-disk techniques when compared to the standard technique. This finding may be explained by the increasing resistance of these bacteria to antibiotic drugs, which has spread worldwide in the last decades. Peritonitis-free survival at 5 years was almost equal with the three techniques, a result which correlates with the behavior of the peritonitis rate.
Culture-negative peritonitis episodes represented on average one quarter of all episodes, with a significant increase in the incidence over the 27-year period. This remains a major diagnostic problem also in other parts of the world: 27% in the UK,51 18.8% in USA,52 16.7% in Scotland,10 13.4% in Australia28 and 26% in Brazil.18 The high proportion of culture-negative peritonitis demonstrates a substantial diagnostic problem, one explanation for this is the lack of adequate standardization of reference laboratories in the taking and processing of samples for the detection of microorganisms in the peritoneal fluid which persists even with advances in microbiological isolation techniques and highlights the need to implement standardized systems for sample acquisition and processing.
In conclusion, the peritoneal dialysis-associated peritonitis depends on multiple factors. In this study, the rate of CAPD-related peritonitis was similar throughout the three decades reviewed, despite the use of three different CAPD systems. It seems that other factors like socio-cultural and educational level of these patients, accessibility to healthcare services and the distance to the dialysis center, could influence the rate of peritonitis, a complication that negatively impacts the quality of life of CAPD patients.
Conflict of interest
The authors declare that there is no conflict of interest associated with this manuscript.
Table 1. Microbiological isolation according to the PD technique.
Table 2. Cure rate according to the microorganism during the three techniques of peritoneal dialysis.
Figure 1. Annual incidence of peritoneal-dialysis related peritonitis episodes according to three peritoneal dialysis techniques. Standard 1981-1996. Twin-bag ANDY plus 1997 - 2001 and Stay-safe ANDY-disk 2002-2008.
Figure 2. Incidence of peritoneal-dialysis related peritonitis from 1981 to 2008 according to the microorganism prevalence expressed as episodes per patient-year.
Figure 3. Peritonitis-free survival.