Dear Editor,
Peritoneal dialysis (PD) after removing the catheter due to peritonitis in patients with chronic kidney disease is a treatment option that is certainly not free from subsequent complications and technique failures.
We present two clinical cases with early malfunction of the peritoneal catheter due to multiple adhesions.
Case 1: patient 67 years of age with a history of diabetes mellitus on automatic peritoneal dialysis (APD) who was admitted with a case of peritonitis and exit orifice infected with Burckolderia cepacia and an abdominal ultrasound image suggesting chronic cholecystitis. Given the poor clinical evolution and the persistent cloudy peritoneal fluid, we decided to remove the catheter and perform cholecystectomy in the same surgical procedure. Subsequently, the patient underwent haemodialysis (HD) and received antibiotic treatment (cyprofloxacine and meropenem) for two weeks after removal of the catheter according to the antibiogram.
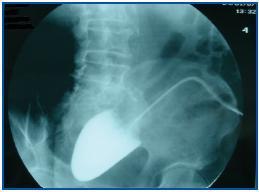
The patient decided to have the new peritoneal dialysis catheter implanted a month and a half after its removal (abdominal CAT showed no changes). The procedure was performed by general surgery, during which the lax adhesions that were observed were liberated. One month after implantation, we observed that draining was difficult. A peritoneography was taken (50ml iobitridol 300mg/l), revealing the presence of contrast limited to a small cavity (figure 1).
In light of these results, we decided to transfer the patient to HD and remove the peritoneal catheter, which was completely clogged by omental adhesions.
Case 2: male patient aged 78 with a personal history of ischaemichypertensive cardiopathy, diverticulosis, chronic kidney disease (ischaemic type), undergoing APD since February 2005. He had suffered various peritonitis episodes: Klebsiella in March 2005, E. coli in August 2005 and Serratia marcescens and E. faecalis in September 2005. The abdominal CAT images were compatible with diverticulitis, and antibiotic treatment was administered. In October 2006, he presented a new episode of peritonitis with Pseudomona aeruginosa, and for this reason, it was decided to remove the peritoneal catheter, transfer the patient to haemodialysis and administer further antibiotic treatment according to the antibiogram.
In December 2006, at the patient¿s request and due to significant vascular access difficulties, we decided to implant a peritoneal dialysis catheter (abdominal CAT was normal), liberate lax adhesions during the procedure and verify catheter function whilst in the operating room.
At 15 days after implantation, the peritoneal catheter was malfunctioning and provoking difficulties during both infusion and drainage. The peritoneography showed an image similar to that described for the previous case (figure 2).
The patient made the definitive transfer to HD once the catheter was removed; multiple adhesions were observed.
Removal of the peritoneal catheter is necessary when treating certain types of peritonitis, principally those caused by funghi, enterobacteria, or where there is a coexisting subcutaneous tunnel infection.
There is no reliable objective method for identifying irreversible peritoneal damage prior to reinsertion of a new catheter. Ultrasound and abdominal CAT images are the most widely-used tests, but they have a low sensitivity.1
After a review of 189 cases of peritonitis in which a catheter was removed and subsequently replaced, Troidle et al. concluded that only 20% continue with that method one year after the removal.2
If the decision is made to return to PD, we recommend implanting the catheter using open surgery or laparoscopic surgery that allows us to obtain more information on the abdominal cavity condition.3 This reimplantation should be performed at least 3-4 weeks after remission of the infection.4
In order to make this decision, we must take into account such factors as the severity of the peritonitis, residual diuresis, previous ultrafiltration capacity, aetiological agent, etc. With all of the above in mind, the decision must be a personalised one.
Figure 1.
Figure 2.