According to the American Society of Diagnostic and Interventional Nephrology, Diagnostic and Interventional Nephrology (DIN) is defined as the application of imaging techniques and interventionism in the field of Nephrology in order to improve the management and care of patients with kidney disease.1
DIN was originally developed by nephrologists as part of the search for solutions in light of the requirements and difficulties encountered during normal clinical practice, both on a diagnostic and treatment level2–4; the nephrologists were shaping and developing DIN, for example, by designing catheters for hemodialysis. Furthermore, ultrasound is being more widely used in medicine, proving its great benefit in the management of kidney patients since the 1990s.5,6 Currently, the majority of specialities (medical and surgical), have incorporated ultrasound into their normal clinical practice and they perform specific interventions within their speciality.7,8 This situation has not arisen in our speciality, despite the fact that the main DIN milestones were led by nephrologists. In recent decades, this field has remained neglected, with the majority of our procedures being performed by other specialists and it is losing ground as an area of interest in Nephrology. At the healthcare level, there is an impact on other specialities, such as Radiology and Vascular Surgery, which have incorporated these procedures into their service portfolios, thus increasing their workload and making difficult the diligent management of kidney patients.
There is currently some controversy between those who believe that the performance of these techniques by the nephrologist is intrusive and has no value in the training of resident doctors,9 and those who think, like us, that they should be performed by the nephrologist, since it provides greater autonomy, they are performed faster and improve the patient management.10 Unfortunately, only few centres had a record of the procedures performed, the medical professionals do not receive specific training in the various techniques, and there is no offical exam or certification to evaluate the proficiency of the nephrologists in the performance of such procedures.11,12
From our point of view, the development of a DIN section within Nephrology is highly efficient and economically feasible; it reduces the time waiting for the procedure and optimises resources, avoiding the overload of other departments, as has already been demonstrated in previous publications.13–19 Furthermore, the incorporation of DIN impacts on decision-making and on the viability and the survival of accesses for renal replacement therapy.20
As it is an area where the boundaries are blurred with other specialities, we believe that the implementation of a DIN programme should be planned, gradually implemented and agreed upon with the other departments involved, whenever possible, thus enabling knowledge sharing21 and avoiding disputes. Furthermore, access to specific training should be ensured for all nephrologists interested in performing these techniques,11,13,22 by developing educational tools23 and establishing normal clinical practice standards, as well as an assessment or certification that officially validates the doctors’ capacity to perform diagnostic and interventional procedures.
Furthermore, the development of DIN would allow to recover clinical activities and prevent the progressive loss of diagnostic and therapeutic skills that may rely on other specialities. It would also potentiate health management processes and the continuity of inter-level healthcare, promote teaching and research, collaborate in the sustainability of the healthcare system and make the speciality more attractive, both for nephrologists and for specialists in training, an area awaiting improvement in recent years, as shown by the higher score numbers of resident choosing the medical speciality in Spain.24 Finally, we must stress that these practices are included in the specialist Nephrology guideline25 and they are an objective in the 2016–2020 strategic plan of the Spanish Society of Nephrology (SEN).26
Based on the reasons exposed above., in 2014 the SEN approved the generation of Diagnostic and Interventional Nephrology Group (Grupo de Nefrología diagnóstica e intervencionista, GNDI)27 aiming to promote the dissemination, establishment and development of DIN in Spain, and retrieve the role of the nephrologist in techniques specific to the speciality. This objective requires an increase in the number of trained nephrologists, the establishment of standards of performance and the certification of official training centres for interventional nephrologists in Spain.
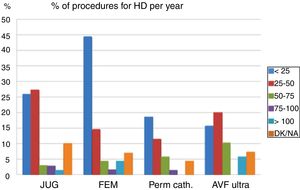
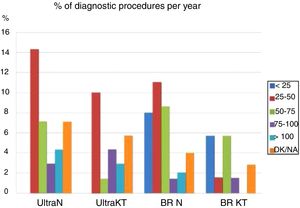
As an initial project and with the purpose of both learning and dissemination about the situation of the Spanish DIN, the GNDI conducted a survey in 2015 via email on all the Nephrology departments in Spain through the SEN. The response rate to the survey was low (35.8%) but similar to the level of participation recorded in other countries,28–30 highlighting that less than 70% of the temporary catheter implantations for haemodialysis were echo-guided, despite being recommended by the official Spanish guidelines,31,32 and less than 30% of the departments performed diagnostic ultrasounds, with the arteriovenous fistula (AVF) ultrasound being the most widely used technique (65%). We can draw the conclusion that DIN in Spain is rare, limited mainly to(techniques performed >30%) to the canalisation of ultrasound-guided catheters, kidney biopsies and AVF ultrasounds for HD (Figs. 1 and 2). Although the interpretation of our results is limited by the lack of participation, it is still representative since we obtained responses from all the autonomous communities. Regarding its future implementation, 8.5% of the centres rejected the idea of incorporating DIN into their portfolio of services.
Annual volume of interventional procedures. All the techniques performed by the nephrologist using ultrasound guidance.
DK/NA: don’t know/no answer; Fem.: temporary femoral catheter; Jug.: temporary jugular catheter; KT: kidney transplant; N: native kidney; Perm.: permanent tunnelled catheter.
Other countries that have published their experience in this field show good clinical and technical results, a lower or similar complication rate to that existing in the literature, and an improvement in the patient's comprehensive care.12,28–30 As observed in our country the response rate in those countries in which the survey was conducted was equally low (10–37%), with the exception of the survey conducted by Berns and O’Neill12 in the USA (68%). A high percentage of nephrologists from several countries referred to a lack of training in interventional and diagnostic techniques.
Compared with the level of DIN developed in the USA,12 where the term DIN was coined, we observed that Spanish nephrologists performed fewer ultrasound-guided native kidney biopsies (42% vs. 35.8%), kidney transplants (51% vs. 46%), intervention for an AVF is anecdotal and the percentage of temporary accesses for ultrasound-guided haemodialysis is considerably lower (88.5% vs. 64%). On the other hand, in Spain, the performance of diagnostic ultrasounds (NK: 8% vs. 2.6% and kidney transplants: 11% vs. 23%) and the insertion of peritoneal catheters by a nephrologist are more frequent (14% vs. 26%).
Ultimately, DIN provides professionals with greater autonomy, optimises existing resources and reduces waiting times, resulting in an improvement in the continuity of care of the kidney patient that is highly efficient and at a reduced cost. DIN in Spain is being expanded slowly. We encourage Nephrology departments to include DIN in their portfolio of services and we also encourage the residents to be trained in this new discipline, which is included in the speciality's training programme. Therefore it should be insured that all nephrologists are educated through the implementation of training programmes. Centres that provide this training must be accredited.
Please cite this article as: Sosa Barrios H, Ibeas López J, Roca Tey R, Ceballos Guerrero M, Betriu Bars A, Cornago Delgado I, et al. Situación de la nefrología diagnóstica e intervencionista en España. Nefrologia. 2018;38:459–462.