Introduction: Chronic renal disease (CRD) affects physical, emotional and social wellbeing of children. Renal adult and adolescent patients have a poorer quality of life (QL) than healthy population but few studies have been performed in children with CRD and appropriate QL measurement tools. Objectives: To assess QL in children with CRD comparing it with healthy children. Material and methods: Cross-sectional study in 71 children with CRD and 57 healthy children with the generic health status tool MOSF-SF-20 answered by children older than 9 and their parents and only by parents when children were younger than 9. Results: Children with CRD have a poorer QL than healthy children with significant differences in general self-esteem, physical performance and physical activity and no significant difference in socialization. On the contrary they refer less pain and emotional discomfort than healthy population. Perceived QL of children by parents is also worse in CRD population affecting all but pain dominions. 9-12 years old children and their parents agree in all QL dominions while parents underestimate social function and emotional well-being when their children were older than 12. Conclusions: QL in children with CRD is worse than in healthy children mainly in physical function and general self-esteem and agree with parents perceptions.
Introducción: La enfermedad renal crónica (ERC) afecta al bienestar físico, psíquico y social del niño. En adultos y adolescentes se ha descrito una peor calidad de vida (CV) en enfermos renales que en población sana, pero hay pocos estudios con instrumentos de medida de CV en niños con enfermedad renal. Objetivo: Estudiar la CV de los niños con ERC y compararla con un grupo control de niños sanos. Material y métodos: Estudio transversal en 71 niños con ERC y 57 sanos utilizando el cuestionario de salud general MOS-SF-20 en mayores de 9 años y sus padres o sólo en éstos en los menores de 9 años. Resultados: Los niños con ERC tienen peor CV que los niños sanos con diferencia significativa en la percepción de la función física, del rol físico y del estado general de la salud y no significativa en la socialización. Los niños enfermos refieren menos dolor y mejor bienestar emocional que los niños sanos. La calidad percibida por los padres es también peor en la población de niños enfermos que en la de niños sanos en todos los dominios excepto en el dolor. La CV percibida por los padres coincide en todos los dominios con la de los niños de 9 a 12 años e infravalora la función social y el bienestar emocional en los niños mayores de 12 años. Conclusiones: La CV en niños con ERC es peor que en niños sanos y afecta sobre todo al ámbito físico y a la salud general, en lo que coinciden niños y padres.
INTRODUCTION
Chronic kidney disease (CKD) is a progressive and irreversible disease that requires frequent clinical and analytical controls, a diet restricting foodstuffs and sometimes liquids, and the taking of drugs several times a day in the majority of cases. This causes not only medical but also parental dependence and the alteration of typical childhood activities such as play, study, development and growth. Children and their parents must learn how to coexist with the disease, which implies a break with their normal life, physical, academic and social activities.1
There are very few publications on the quality of life (QoL) of children with CKD. The majority of studies have been conducted on adolescent or adult patients who started with the disease in childhood.2,3
The objective of our work was to study the QoL perceived by children with CKD, understanding this as a multidimensional concept that includes physical, psychological and social well-being,4 and compare the results with the QoL of a control group of healthy children.
MATERIAL AND METHODS
Transversal study whose accessible population was children treated in the Children’s Nephrology Department of the Gregorio Marañón University Hospital, Madrid, Spain. 71 CKD patients (more than 3 months’ evolution) were included. Of them, 22 were following conservative treatment, 33 had received kidney grafts and 16 were receiving substitution therapy: 11 peritoneal dialysis (PD) and five haemodialysis (HD). The target population was the paediatric population of the Autonomous Community of Madrid and included 57 healthy controls of similar age and socioeconomic level to those of the patient group.
All patients and controls participated in the study voluntarily; the procedure was verbally explained to them previously and they gave their consent to be included.
We used the general health questionnaire MOS-SF-20 (20-item Medical Outcomes Study). This is a self-administered, generic, multidimensional quality of life test, developed by Stewart in 1988, that determines physical, mental and social state as well as general well-being (mental health, pain and general perception of health), whose validity has been studied in adult populations subjected and not subjected to dialysis.5,6 It consists of 20 items or questions that contain information across six functioning domains:
1. Physical functioning, which reflects how health limits daily physical activities for self-care, walking or climbing stairs (6 items: questions 3.1-3.2-3.3-3.4-3.5-3.6).
2. Physical role functioning, or how health interferes with work, school or other daily activities (2 items: questions 4-5).
3. Social functioning, which refers to how state of health and emotional problems interfere with normal social activities (1 item: question 6).
4. Emotional well-being/mental health, which addresses how emotional problems interfere with work or other daily activities and the general state of mental health in-cluding depression, anxiety and emotional behaviour (5 items: questions 7-8-9-10-11).
5. Pain, its intensity and repercussions in normal work and daily activities (1 item: question 2).
6. General health perception, evaluating the personal estimate of current health and resistance to the disease (5 items: questions 1-12.1-12.2-12.3-12.4).
Each question is scored from 0 to 100. The maximum obtainable score is 2,000 and indicates the best QoL. We applied for and received permission to use the MOS-SF-20.
The questionnaire was completed by healthy and sick children. In children under 9 years of age, it was answered exclusively by the parents who gave their opinion on the condition of their children. In children over 9, both parents and children answered separately to compare the results.
Socio-demographic variables were collected: age, civil status, education and work situation of the parents, social level, housing type, number of siblings, working situation in patients over 18, education and school delay.
Methodology
The description of quantitative variables is expressed as mean and standard deviation (SD) and qualitative variables as percentage or frequency. A simple or bivariant analysis was conducted to show associations, using the Chi-square test for qualitative variables where possible, otherwise Fisher’s exact test was used. The non-parametric ANOVA (Kruskal-Wallis) was used to compare the mean values of independent groups when the sample was less than 30 or the variances were not homogeneous.
We determined the reliability of the questionnaire through Cronbach’s alpha coefficient which measures internal consistency. A coefficient higher than 0.7 is an indication of good internal consistency.
The concordance of opinion between parents and children older than 9 years of age was studied using the intraclass correlation coefficient (ICC). This coefficient is used to determine agreement between two distinct groups using the same scale. A value greater than 0.9 indicates excellent agreement, and 0 indicates total disagreement.
RESULTS
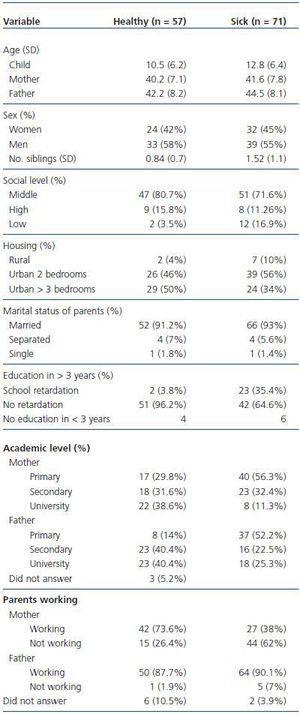
Table 1 shows the sociodemographic data of the healthy and sick population. The two samples (cases and controls) are homogeneous as far as the ages of the children, mothers and fathers and also with respect to the sex of the children and their education. They are not homogeneous in the number of siblings (p < 0.01), nor in school delay, which is greater in the patient group. There is a difference in the percentage of mothers who work between the two populations, being less in the mothers of sick children. Although there appears to be no differences in social level, civil status of the parents, work or housing, this could not be determined given the small sample size.
The reliability of the questionnaire measured with Cronbach’s alpha coefficient has very good internal consistency. The coefficient was 0.8 in the sick children, 0.79 in the healthy children, 0.84 in the parents of sick children and 0.73 in the parents of healthy children.
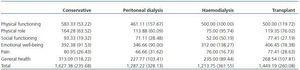
Tables 2 to 4 reflect the results of the MOS-SF-20 questionnaire.
As far as the QoL perceived by the children, there are significant differences in physical functioning (p < 0.01), physical role functioning (p < 0.01), perception of health (p < 0.01) and overall QoL (p < 0.01), the highest scores being in the healthy population which expresses better QoL in this group. We also found differences, although insignificant, in socialisation. The children with CKD mention less pain and better emotional well-being than the healthy children, although not significantly.
With respect to the QoL of children perceived by their parents, this is worse in the sick children with significant difference (p < 0.01) in the domains of physical functioning, physical role functioning, social functioning, general health and total QoL. Emotional well-being is also worse, although without significant differences. Curiously, as in the case of children, pain intensity is worse in the healthy population.
In QoL referred to by the sick children according to therapeutic modality, we have found significant differences between HD and the remaining treatments in the emotional well-being domain and insignificant differences in the domains of physical and social functioning, physical role and overall QoL, improving in PD, conservative treatment and transplant (TX), these last two groups being the ones expressing better QoL. Only those subjected to PD are found to be worse in general health while those subjected to haemodialysis are better in pain, both domains with no significant differences.
The opinion of the parents of the sick children showed significant differences in the domains of physical and social functioning and overall QoL; patients in conservative treatment were found to be better. In emotional well-being, physical role functioning, pain and general health, those in dialysis (HD or PD) were worse, but with no significant differences.
The correlation between the answers of parents and children over the age of 9 measured by ICC was greater than 0.7, indicating good parent-child agreement. We divided the children into three age groups: from 9 to 12 years, 12 to 15 and older than 15 (table 5). In the first group (9-12 years), the ICC was above 0.79 in all items on the questionnaire. In the second group, it was greater than 0.8 in all items except social functioning (0.33), physical functioning (0.58) and emotional well-being (0.46). In the over 15 group, the ICC was higher than 0.7 in all items except social functioning (0.64) and emotional well-being (0.57).
DISCUSSION
QoL is a multidimensional and subjective concept that includes the physical, social and emotional functioning of the child and his or her family, and is altered in the majority of children with chronic disease. The degree to which QoL is affected is not always related to the severity of the disease; given its dual subjective-objective nature, it is also influenced by other economic or social factors or individual expectations.7,8 Currently, therefore, the medical treatment of chronic diseases is not enough and an attempt must be made to improve the perceived well-being of the child and strengthen his or her functional abilities.9,10 In recent years, interest in this field has grown, but its study in infancy is difficult due to the absence of specific, known and validated questionnaires in Spanish able to determine health related quality of life (HRQoL) in paediatric patients with chronic kidney disease, a situation made worse by the inherent difficulty of small children to answer questionnaires. For that reason, the majority of studies conducted have asked the caregivers (parents, teachers, physicians) about the QoL of the children, whose perspective may be different, or questioned adolescents and adults with CKD since childhood.2,3 In the last 5 years a greater effort has been made and there are now publications of QoL in children, although the majority of studies still use generic measuring instruments.11-13
Our selection of the generic MOS-SF-20 questionnaire (abbreviated form of the SF-36) was made, like Morton et al.,6 because of the ease of completion by parents and children, since it is shorter and requires only 10 minutes to answer. The validity of this questionnaire has already been studied in adult populations subjected and not subjected to dialysis.5-14 Furthermore, for this study we determined the reliability of the questionnaire through Cronbach’s alpha coefficient which showed a good internal consistency (α > 0.7).
In the results obtained from the children’s answers (older than 9 years) a worse overall perceived quality of life is observed in the sick children, with significant differences in the domains of physical functioning, physical role functioning and general health perception. The score obtained in socialisation, without being significant, is worse in the sick population. Paradoxically, it is interesting that, although without significant difference, healthy children had somewhat lower scores and, therefore, worse perception of emotional well-being and pain than sick children. McKenna and Goldstein obtained similar results using the generic PedsQL questionnaire. The former11 compares a healthy population of 59 children with CKD in conservative treatment, dialysis or transplant, and Goldstein12 studies 96 patients from 2 to 18 years. Both find worse scores across all domains (physical, emotional, social and academic) than in the healthy population.
Our data also agrees with a multicentric American study which uses a generic questionnaire (CHIP-AE) to analyse 113 CKD patients of 10 to 18 years of age comparing them to 226 healthy subjects of the same age group.2 As with our patients, the sick children in this study showed greater alteration in their physical activity and health, but felt they had more support from their families and a better family environment than the healthy children, which may correspond to the better emotional well-being reported by our patients. This could be explained by the overprotection received by sick children, which in the long term can be harmful for adult life as shown by Grootenhuis et al’s study.3 In this study, sick children had fewer possibilities of adopting socially risky behaviour than healthy children. In our group we found no significant differences in social functioning, although the scores of the sick children were somewhat lower. It is interesting that the sick children reported less sensation of pain, although not significantly less, than the healthy ones, which may be explained by the different perception of this by healthy and sick children.
The perception of parents regarding CKD children’s QoL is also significantly worse (p < 0.01) over almost all domains, except emotional well-being where the difference is insignificant. As far as pain, parents of sick children believe that their children feel less pain than the parents of healthy children.
The coincidence of scores between parents and children stands out in almost all domains, except general health, emotional well-being and pain, which are overvalued by parents. Parents agree with their sick children in the worse perception of physical functioning, physical role functioning and general state of health, as well as in not being affected by pain. Furthermore, they believe their children have greater socialisation difficulties than the children feel. The worse score of the parents in relation to their children with CKD appears across all domains except the physical role, which indicates that they perceive a worse QoL for their children than the children themselves express. The same discrepancies are obtained in McKenna’s study,11 where caregivers underestimate the QoL of the children with an ICC of 0.63. This disagreement between parents or caregivers and the children has been published both in healthy populations and in children with chronic diseases.15,16 In general, parents tend to believe that their children have more problems and worse QoL than expressed by the children themselves.17-19 The majority of authors, therefore, recommend that, when measuring QoL in childhood, both opinions, that of the children and that of their closest caregivers, are taken into account.20
We also emphasize the fact that there are fewer working mothers among the sick children than in the healthy population. Many of them leave their jobs to look after their children, which mostly explains the overprotection of their children making them feel emotionally good during childhood. Mothers, however, express greater anxiety and/or depression.
The aim of the study with this generic questionnaire was not to analyse differences between the distinct treatments of the sick children: for that it would be necessary to use a questionnaire specific to kidney disease. We did, however, identify a tendency towards a worse quality of life in patients subjected to dialysis (HD or PD) in the majority of domains. This has been described in the adult population21 and in a recent work in Spanish adolescents with terminal kidney disease22: in a generic questionnaire, adolescents subjected to transplant report to be more satisfied with their health than the group subjected to dialysis, with no differences when compared to the control group of healthy adolescents, although differences do exist between the group subjected to dialysis and the healthy population.
Our study has certain limitations, such as the number of patients included, since the study was conducted in a single medical centre, and the use of a questionnaire for adults. However, we feel this questionnaire has been a useful tool because, although basic, is it very easy for children to answer, includes QoL domains and has been validated in adults with CKD. With it, we obtain very similar results to studies published recently in other countries and the QoL impact in our patients is demonstrated. We believe it is fundamental that paediatric nephrologists evaluate not only the clinical course of the disease but also the child’s perception of it and of his or her treatment. To that end, the opinion of the caregivers can be sought, but there should be an attempt to obtain the opinion of the children themselves, which may differ in some aspects to that of their parents. Based on the specific needs of each child and his or her family, revisions and treatments can be individualised. This is the only way to obtain not only some acceptable clinical parameters but also to foster an adequate integral social, physical and emotional development that allows the sick child to become an autonomous adult.
In conclusion, we can mention that the main limitation found in this work is the use of a generic test and, therefore, a highly important objective would be to use a specific questionnaire in Spanish, which currently does not exist. With that in mind, we have begun the development of such a questionnaire for future studies.
SUPPORTING SUMMARY
1. What is known about the issue?
Quality of life is affected in chronic diseases. Many studies in adults with chronic kidney disease demonstrate a worse quality of life. QoL has been studied less in children because of the difficulty they have in answering questionnaires, and there are publications questioning parents and caregivers or adolescents and adults who have had kidney disease since childhood. Only in recent years, American data have been published in 3 reports with 59 children (reference 11), 96 (reference 12) and a multicentre study with 113 (reference 2).
2. What does this study contribute?
Information on the quality of life in Spanish children with chronic kidney disease, using a generic general health test (MOS-SF-20), that is compared with healthy children. The test was filled out by children older than 9 years of age and by the parents of all children, older and younger than 9. The concordance of answers between parents and children was obtained to evaluate whether parents are useful to assess the quality of life of their children.
Acknowledgements
We would like to thank our small patients and their families for their collaboration in completing the questionnaires and their patience with us.
Table 1. Sociodemographic data
Table 2. Table 2. MOS-SF-20 answered by children and MOS-SF-20 answered by parents
Table 3. MOS-SF 20 answered by children according to therapeutic modality
Table 4. MOS-SF 20 answered by parents according to therapeutic modality
Table 5. Concordance between parents and children. Intraclass correlation coefficient (ICC)