Kidney transplantation (KT) is the treatment of choice as a renal replacement therapy (RRT) technique.1,2 One of the strategies we have to counteract the imbalance between the supply and demand of organs in patients on the kidney transplant waiting list (KTWL) is living donor kidney transplant (LDKT). Currently, this RRT option is not well known, so it is essential to inform patients about this modality when explaining the different RRT options.3–5 Among the different strategies addressed in our country to increase the availability of organs, the 50 × 22 Plan is currently in force. This plan seeks to exceed 50 donors per million population and 5500 transplants in 2022,6 where optimising LDKT is one of the mainstays of this plan.
A retrospective observational study is presented, whose objective is to assess knowledge about aspects related to living donation and the perceived importance of LDKT through an anonymous questionnaire in a sample of 41 patients from a hospital haemodialysis unit.
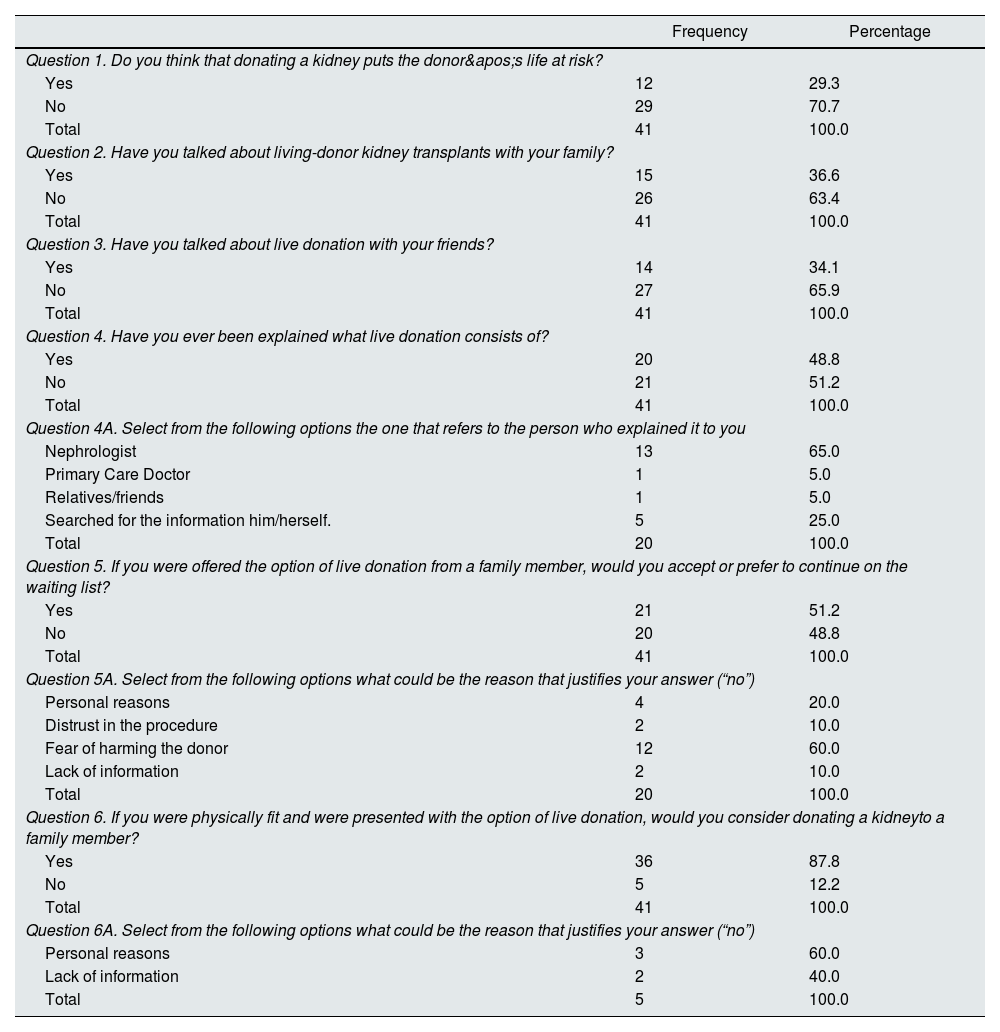
Regarding the study methodology, it was conducted a descriptive analysis of the epidemiological variables of the patients (age, sex and inclusion on the KTWL) and the responses to the questionnaire (Table 1), as well as an statistical analysis to assess the relationship between the different variables and the responses provided.
Responses to the survey of 41 patients from the Hospital Haemodialysis Unit regarding aspects of living donor-kidney transplant.
| Frequency | Percentage | |
|---|---|---|
| Question 1. Do you think that donating a kidney puts the donor's life at risk? | ||
| Yes | 12 | 29.3 |
| No | 29 | 70.7 |
| Total | 41 | 100.0 |
| Question 2. Have you talked about living-donor kidney transplants with your family? | ||
| Yes | 15 | 36.6 |
| No | 26 | 63.4 |
| Total | 41 | 100.0 |
| Question 3. Have you talked about live donation with your friends? | ||
| Yes | 14 | 34.1 |
| No | 27 | 65.9 |
| Total | 41 | 100.0 |
| Question 4. Have you ever been explained what live donation consists of? | ||
| Yes | 20 | 48.8 |
| No | 21 | 51.2 |
| Total | 41 | 100.0 |
| Question 4A. Select from the following options the one that refers to the person who explained it to you | ||
| Nephrologist | 13 | 65.0 |
| Primary Care Doctor | 1 | 5.0 |
| Relatives/friends | 1 | 5.0 |
| Searched for the information him/herself. | 5 | 25.0 |
| Total | 20 | 100.0 |
| Question 5. If you were offered the option of live donation from a family member, would you accept or prefer to continue on the waiting list? | ||
| Yes | 21 | 51.2 |
| No | 20 | 48.8 |
| Total | 41 | 100.0 |
| Question 5A. Select from the following options what could be the reason that justifies your answer (“no”) | ||
| Personal reasons | 4 | 20.0 |
| Distrust in the procedure | 2 | 10.0 |
| Fear of harming the donor | 12 | 60.0 |
| Lack of information | 2 | 10.0 |
| Total | 20 | 100.0 |
| Question 6. If you were physically fit and were presented with the option of live donation, would you consider donating a kidneyto a family member? | ||
| Yes | 36 | 87.8 |
| No | 5 | 12.2 |
| Total | 41 | 100.0 |
| Question 6A. Select from the following options what could be the reason that justifies your answer (“no”) | ||
| Personal reasons | 3 | 60.0 |
| Lack of information | 2 | 40.0 |
| Total | 5 | 100.0 |
Firstly, the findings of the study are that both sex and age are influential factors in the prevalence of chronic kidney disease (CKD) in patients on haemodialysis. As has already been observed in other series, there is a higher prevalence in men and in those about 65 years of age.7
In addition, 56% of patients were excluded from KT, which could negatively influence knowledge about LDKT. In the statistical analysis shows that there was not a significant relationship between being on the KTWL and the survey responses, except for question 2, which seems to demonstrate an association between being on the KTWL and talking about LDKT (P = .006).
One of the most relevant results obtained was that in basically half of the cases (48.8%) received information about the live donation procedure, but only 22% were on the KTWL. Furthermore, more than half (65%) of the total number of patients informed about LDKT declared that they received information from the nephrologist. However, when analysing these findings, it must be taken into consideration that the degree of information that patients received when stating that LDKT had been explained to themsince it does not have the same value the individualised and specific information about LDKT in a consultation designed for this purpose, than the rather superficial information during a medical examination by the primary care provider, by the nephrologist himself, by the media or from Internet.
Another fact worth highlighting is that 48.8% of patients would prefer to stay on the KTWL rather than accept a kidney from a family member; the fear of harming the donor is the reason that justified this response in most cases (60%). However, the vast majority (87.8%) would be willing to donate a kidney to a family member. This result can be explained by the fact that they experience first-hand the situation of RRT and everything it implies (strict control of water intake, restrictive diets, impact on quality of life, etc.).
LDKT is regulated in Spain by Transplant Law 30/1979, implemented by Royal Order 2070/1999, which allows the donation of an organ if it is compatible with life. Furthermore, it specifies that the organ will be donated to a specific person without economic, psychological or social conditions. The donor must be of legal age, with full mental faculties, and in an optimal state of health, accredited by a medical certificate.6
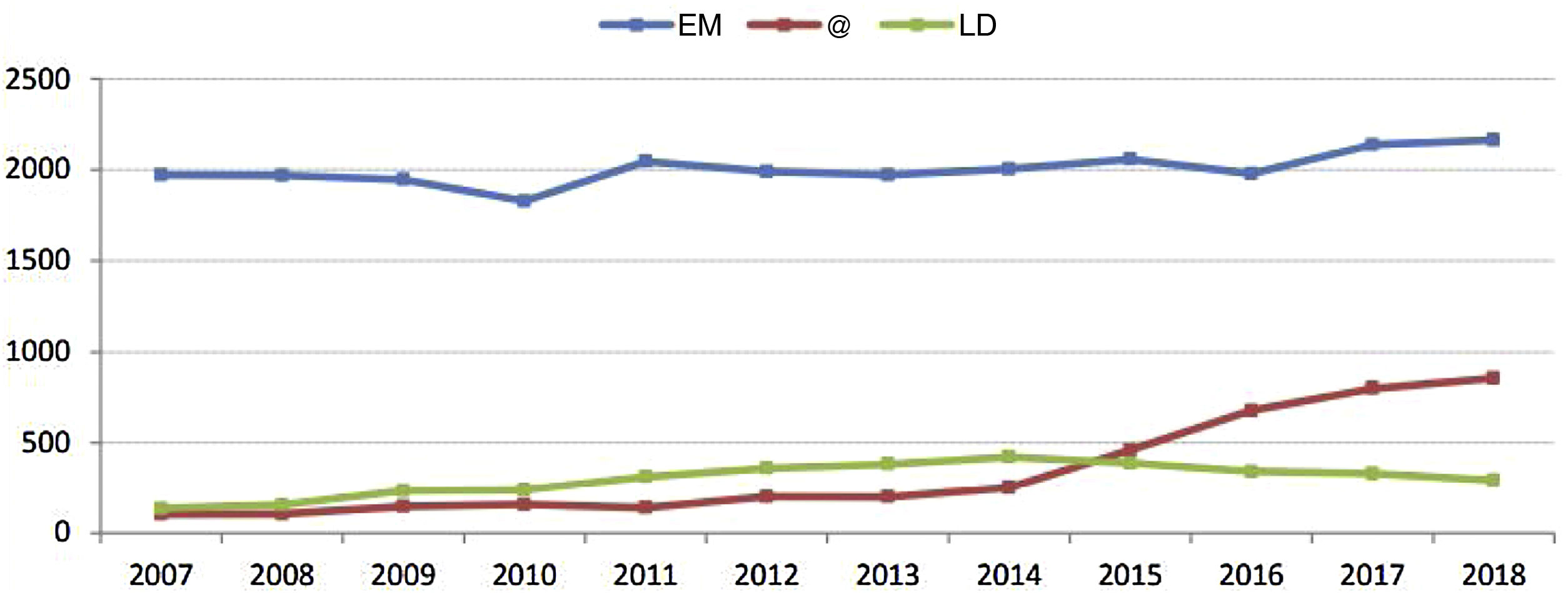
LDKT has demonstrated greater survival than cadaveric donor transplantation and a low percentage of complications in the donor.8 In Spain, around 85% of kidney transplants are from cadaveric donors, vs 10%–15% from living donors (Fig. 1), making for scant LDKT activity as compared to other countries.9
In conclusion, there must be a better promotion and detailed explanation of precisely what involves the LDKT procedure. Likewise, this information should be provided as early as possible in advanced CKD consultations, avoiding the patient's entry into dialysis, as this negatively influences the survival of the patient and the graft. To achieve this, it would be interesting to establish certain protocols/guides in which, once a certain renal function is reached, the LDKT option is explained to the patient, giving them enough time to evaluate this option and be evaluated.
Ethical considerationsThe authors declare that the protocols established in their place of work have been followed when accessing the patient's clinical records to create this publication for dissemination to the scientific community.
FundingThis study received no specific funding from public, private or non-profit organisations.
Conflicts of interestThe authors declare that they have no conflicts of interest.