Renal infarctions are infrequent, usually they are a consequence of atheroembolism from the heart (atrial fibrillation, infective endocarditis, atrial myxoma, among others), renal vasculopathy or hypercoagulability states (resistance to activated protein C, hyperhomocysteinemia, antiphospholipid syndrome, etc.).1 Paradoxical renal infarctions associated with patent foramen ovale have also been described. We present the first case of bilateral renal infarction associated with patent foramen ovale and anticardiolipin +.
The patient was 38-year-old male with persistent pain in right renal flank with a diagnosis of renoureteral colic/acute pyelonephritis. Pain worsening and new consultations, prompted patient admission. Physical examination revealed blood pressure 147/87mmHg and body temperature of 36°C, heart with regular rhythm, no murmurs and with preserved pulmonary sounds and pain on the right flank with palpation but not induced with percussion.
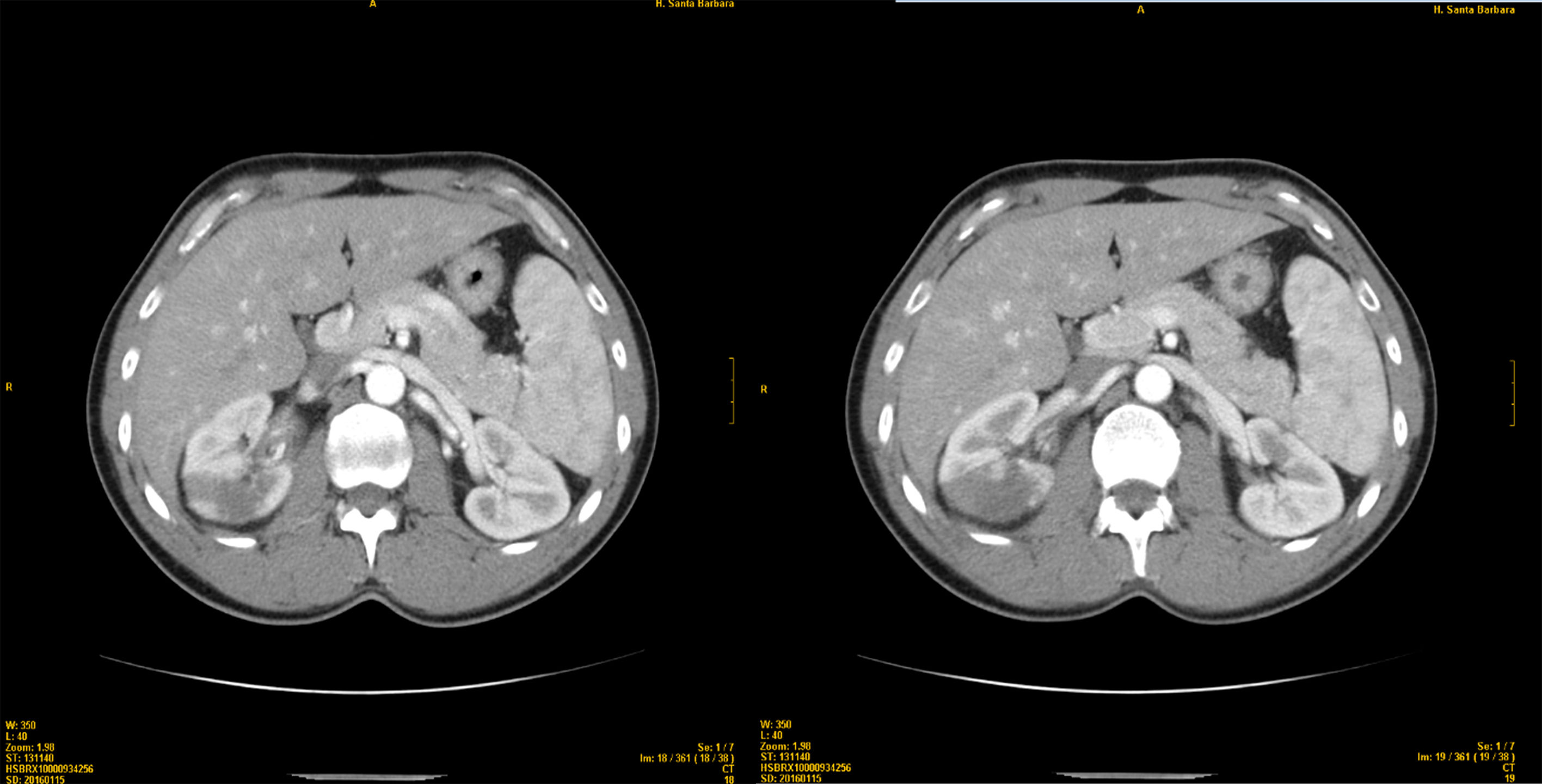
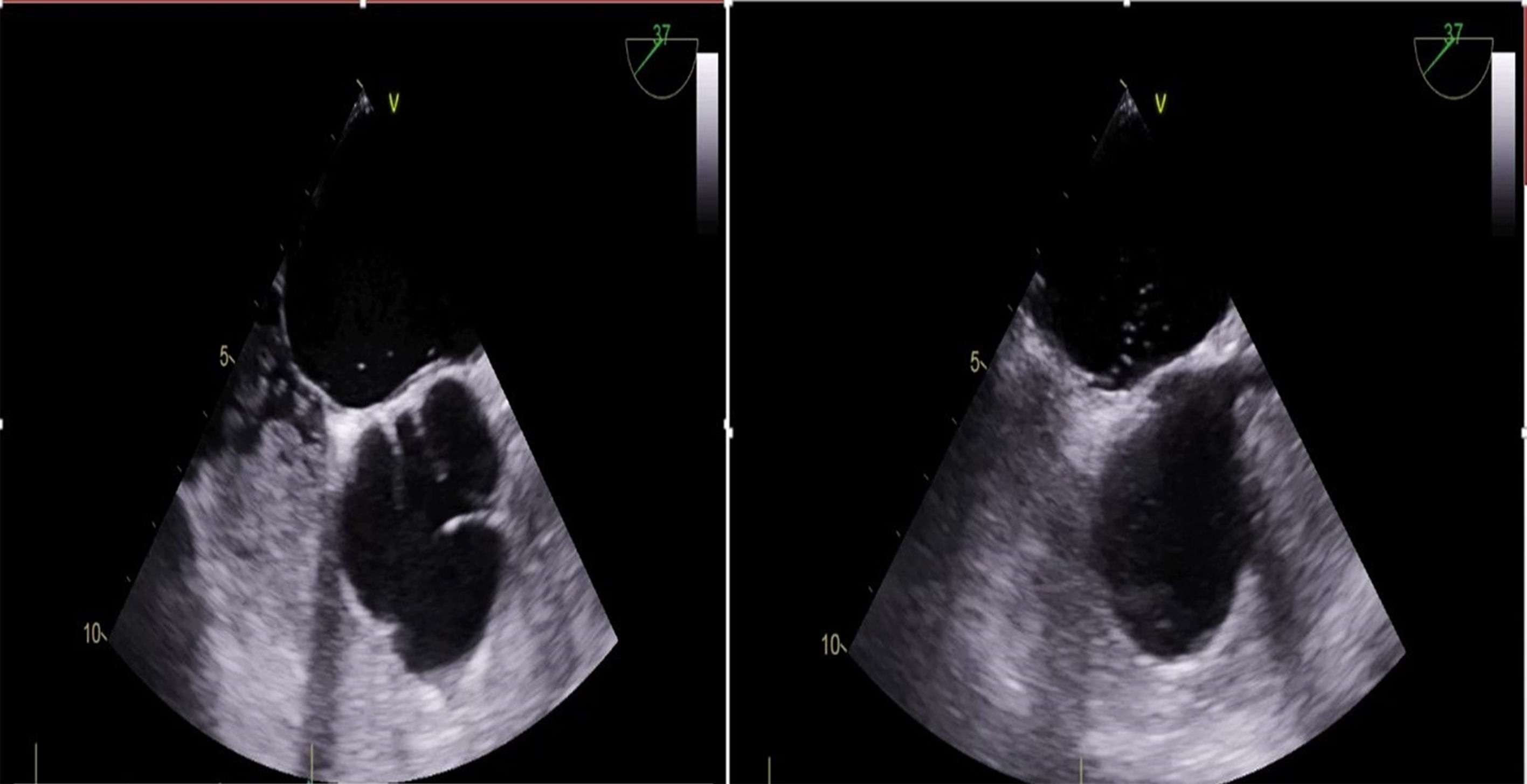
The blood chemistry showed increased LDH and APTT, with normal renal function and without proteinuria or hematuria. The electrocardiogram showed no signs of acute myocardial ischemia, and an abdominal-pelvic ultrasound revealed areas of hyperechogenicity in the right kidney. CT angiography revealed bilateral renal perfusion defects (Fig. 1), which confirmed the diagnosis of bilateral renal infarction by arteriography. The anticardiolipin antibodies were positive and a transesophageal echocardiogram revealed a patent foramen ovale without aneurysm of the interatrial septum, with the passage of bubbles while performing Valsalva maneuver (Fig. 2, Video 1). The patient developed ischemic colitis 12 days later: oral anticoagulation was started. The evolution was satisfactory and 6 months later the patient was asymptomatic and without recurrences.
Renal infarction is characterized clinically by low back pain and refractory arterial hypertension. Leukocytosis, hematuria and high CRP and LDH may be present. Renal perfusion defects in a CT angiography are very suggestive and renal arteriography is the gold standard for diagnosis
Iwasaki et al.2 described a case of isolated patent foramen ovale manifested as renal infarction with impaired renal function. Nara et al.3 diagnosed bilateral renal infarction in a patient with poorly controlled arterial hypertension, and discovered a patent foramen ovale. Finally, Ronco et al.4 attended a hypertensive urgency in a patient that was found to have renal infarction and patent foramen ovale. Transesophageal echocardiography establishes the diagnosis of permeable foramen ovale. The antiaggregation begins with the first embolism; percutaneous closure can be considered in case of recurrence or aneurysm of the interatrial septum. The antiphospholipid syndrome presents with arterial and venous thrombosis,5–7 the diagnosis is based on clinical and biochemistry findings7 and is candidate to early anticoagulation.8
Here we have described the first case with patent foramen ovale, antiphospholipid syndrome and renal infarctions. We believe that it is indicated to perform an analytical and echocardiographic studies in patients with renal infarctions to diagnose structural abnormalities or thrombophilias so that antiplatelet or anticoagulant treatment is initiated early.
Conflict of interestsThe authors do not declare conflicts of interest.
To the Cardiology and Nephrology Services of the HGUCR.
Please cite this article as: Pérez Díaz P, Sánchez de la Nieta García MD, Piqueras Flores J, Maseda Uriza R, Requena Ibáñez JA, Rayo Gutiérrez M. Foramen oval permeable con anticardiolipina+, una causa rara de infartos renales múltiples. Nefrologia. 2018;38:105–107.