Primary tubulopathies are rare and usually present at pediatric age. Recent advances in genetic diagnosis and treatment have changed its natural history. This study provides the clinical spectrum of a series of primary tubulopathies diagnosed in a Pediatric Nephrology Unit and to offer long-term follow-up data regarding growth, estimated glomerular filtration (eGFR) and intercurrent complications.
Patients and methodsObservational study in 53 patients with primary tubulopathies and identified genetic defect: Gitelman syndrome (36%), distal renal tubular acidosis (15%), cystinuria (11%), X-linked hypophosphatemic rickets (7%), Dent-syndrome Lowe (7%), cystinosis (6%), and 1–2 cases of other tubulopathies. Demographic, analytical and clinical data were collected at diagnosis, during evolution and at the time of the study.
ResultsThe age (median and interquartile range) at diagnosis was 5.08 years (1.33−8.50). The most frequent presentation manifestations were metabolic decompensations associated with intercurrent processes (40%) and short stature (38%). Height (mean ± SD) was −1.39 ± 1.49 at diagnosis and 1.07 ± 1.54 after a follow-up of 18.92 (6.25−24.33) years. Sixteen (32%) developed an eGFR <90 ml/min/1.73 m2. Three patients required replacement renal replacement. Eleven patients had metabolic decompensations that required hospitalization, 9 renal colic and/or kidney stones and 10 mental problems. Six of 8 patients with distal renal tubular acidosis developed sensorineural deafness.
ConclusionsPrimary tubulopathies are a heterogeneous group of diseases that cause growth impairment, largely reversible with treatment, risk of eGFR reduction and significant extrarenal complications derived or associated.
Las tubulopatías primarias son raras y se presentan habitualmente en la edad pediátrica. Avances recientes en diagnóstico genético y tratamiento han cambiado su historia natural. Este estudio presenta el espectro clínico de una serie de tubulopatías primarias diagnosticadas en una Unidad de Nefrología Pediátrica y ofrece datos seguimiento a largo plazo sobre crecimiento, filtrado glomerular estimado (FGe) y complicaciones intercurrentes.
Pacientes y métodosEstudio observacional en 53 pacientes con tubulopatías primarias y defecto genético identificado: síndrome de Gitelman (36%), acidosis tubular renal distal (15%), cistinuria (11%), raquitismo hipofosfatémico ligado al X (7%), síndrome de Dent-Lowe (7%), cistinosis (6%), y 1 o 2 casos de otras tubulopatías. Se recogieron datos demográficos, analíticos y clínicos al diagnóstico, durante la evolución y en el momento del estudio.
ResultadosLa edad (mediana y rango intercuartil) al diagnóstico fue de 5,08 años (1,33-8,50). Las manifestaciones de presentación más frecuentes fueron descompensaciones metabólicas asociadas a procesos intercurrentes (40%) y talla baja (38%). La talla (media ± DE) fue de −1,39 ± 1,49 al diagnóstico y 1,07 ± 1,54 tras un seguimiento de 18,92 (6,25,24,33) años. Dieciséis (32%) desarrollaron FGe <90 ml/min/1,73 m2. Tres pacientes requirieron reemplazo renal sustitutivo. Once enfermos tuvieron descompensaciones metabólicas que requirieron hospitalización, 9 cólicos nefríticos y/o cálculos renales y 10 problemas mentales. Seis de 8 pacientes con acidosis tubular renal desarrollaron sordera neurosensorial.
ConclusionesLas tubulopatías primarias son un grupo heterogéneo de enfermedades que ocasionan afectación del crecimiento, reversible en gran medida con tratamiento, riesgo de reducción de FGe e importantes complicaciones extrarrenales derivadas o asociadas.
Primary renal tubulopathies are rare congenital diseases that affect the renal tubule, producing metabolic, mineral and acid-base balance alterations. Demographic, clinical, and biochemical information is based on single cases or case series including a limited number of patients. In recent years there has been a growing interest in these entities due to the advances in genetic diagnosis and the incorporation of new therapeutic targets, with the consequent improvement in morbidity and mortality.1 Presently, there is large number of these patients that require a change to adult medical services, with the associated and inherent risk of loss of medical follow-up. There are only a limited number publications that analyze the long-term follow-up of patients with tubulopathies.
The present study presents the long-term follow-up data of a group of patients with tubulopathy diagnosed during childhood in a pediatric hospital unit. The objective is to provide information on the evolution of these diseases mainly related to growth, kidney function, development of nephrocalcinosis or urolithiasis and intercurrent complications.
Patients and methodsLongitudinal study of patients with primary tubulopathies diagnosed during pediatric age in the Pediatric Nephrology Service of the Central University Hospital of Asturias The study lasted from their diagnosis to their last follow-up, using the digitized clinical history of computer support during the period between January 1 from 1988 to December 31, 2018. Informed consent was obtained after reading the document explaining the characteristics of the study. It was requested the collaboration and permission of the nephrology services of our hospital (32 patients) and of other hospitals in the region of Asturias (10 patients) and outside the province (6 patients) to update the data required for follow-up. In addition, we contacted 5 patients whose medical follow-up was unknown.
Patients included were diagnosed in pediatric age with: Gitelman syndrome (GS), distal renal tubular acidosis (DRTA), cystinuria, cystinosis, X-linked hypophosphatemic rickets (XLHR), nephrogenic diabetes insipidus, hypomagnesemia syndrome with hypercalciuria and nephrocalcinosis (FHHNC), Gordon syndrome, Dent disease (DD), Lowe syndrome (LS), mitochondrial diseases, hypophosphatemic rickets with hypercalciuria (HHRH), and epidermal growth factor receptor defect. Patients diagnosed with acquired transient renal tubulopathies, secondary to drugs, toxic or autoimmune diseases, diagnosed with primary tubulopathies in adulthood, not located due to lack of administrative information and/or who refused to enter the study were excluded. The diagnosis was made on the basis of clinical and biochemical data and, if possible, the diagnosis was confirmed by genetic study.
A data collection form was prepared that included personal data, clinical, analytical and radiology information since diagnosis to the last follow-up. Information was obtained from the medical records.
Estimated glomerular filtration rate (eGFR) was calculated using serum creatinine values using the revised Schwartz equation for pediatric patient2 and the CKD-EPI 2009 for adults.3 Due to the persistent abnormalities of tubular function with secondary biochemical alterations, all patients had chronic kidney disease. Chronic kidney failure was considered if eGFR < 90 ml/min/1.73 m 2 and ESRD if eGFR < 15 ml/min/1.73 m2.4
Reference values from the 2010 Growth Spanish Study were used to calculate standard deviations (SD) of the corresponding height for age and gender.5 Growth retardation was considered to be a height below −2 SD.6 If height of the parents was available the genetically determined height was calculated according to the following formula: (father’s height + mother’s height ± 13)/2 according to Tanner's formula.7
The study was approved by the Regional Research Ethics Committee of the Principality of Asturias. The statistical analysis was performed using the SPSS software package for Windows v. 16 (IBM Corp, Armonk, NY, USA). Descriptive statistics were used in the study. The quantitative variables were expressed as mean and SD (x¯ ± SD) or median and interquartile range, and qualitative variables as proportion and percentage, unless otherwise indicated.
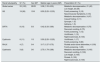
ResultsPresentation and diagnosisA total of 53 pediatric patients, from 44 families, were included. All of them Caucasian. The most frequent tubulopathy was GS in 19 cases of which 16 (84%) were of gypsy ethnicity, followed by DRTA, cystinuria, XLHR and cystinosis (Table 1). The remaining tubulopathies were less frequent, less than 3 cases per each specific type of tubulopathy (nephrogenic diabetes insipidus, FHHNC, DD, LS, Gordon syndrome, HHRH, mitochondrial diseases, and epidermal growth factor receptor defect) and accounted for approximately 25% of the total.
Primary tubulopathies. Data at presentation in the total series and in the most prevalent diseases, with 3 or more children.
| Renal tubulopathy | N.º (%) | Sex M/F | Median age in years (IQR) | Presentation N.º (%) |
|---|---|---|---|---|
| Global series | 53 (100) | 28/25 | 5.08 (1.33−8.50) | Metabolic decompensation, 21 (40) |
| Low height, 20 (38) | ||||
| GS | 19 (36) | 10/9 | 8.50 (5.25−12.33) | Family screening, 3 (16) |
| Neuromuscular Symptoms, 3 (16) | ||||
| Metabolic decompensation, 9 (47) | ||||
| Casual finding, 2 (11) | ||||
| Syncope, 1 (5) | ||||
| Asthenia, 1 (5) | ||||
| DRTA | 8 (15) | 5/3 | 0.42 (0.33−3.69) | Metabolic decompensation, 6 (75) |
| Recurrent vomiting, 6 (75) | ||||
| Family screening, 1 (12) | ||||
| Urolithiasis, 1 (12) | ||||
| Nephrocalcinosis, 8 (100) | ||||
| Cystinuria | 6 (11) | 1/5 | 5.50 (2.25−12.25) | Urolithiasis, 1 (17) |
| Family screening, 5 (83) | ||||
| RHLX | 4 (7) | 0/4 | 3.17 (1.27−5.75) | Rickets and/or bone deformities, 4 (100) |
| Family screening, 1 (25) | ||||
| Cystinosis | 3 (6) | 3/0 | 2.75 (1.79−2.88) | Metabolic decompensation, 3 (100) |
| Recurrent vomiting, 3 (100) | ||||
| Low height, 3 (100) | ||||
| Rickets, 3 (100) | ||||
| Nephrocalcinosis, 3 (100) |
DRTA: distal renal tubular acidosis; F: female; M: male; N.º: number of cases; XLHR, X-linked hypophosphatemic rickets; IQR: interquartile range; GS: Gitelman syndrome.
The most frequent initial clinical manifestations were (Table 1): metabolic abnormalities that included electrolyte, acid-base and/or calcium phosphate alterations, associated with intercurrent processes (21 cases, 40%), growth retardation (20 cases, 38%), recurrent vomiting (11 cases, 21%), polyuria (10 cases, 19%), abdominal pain (10 cases, 19%), rickets and bone deformities (7 cases, 13%), asthenia (6 cases, 11%), urolithiasis (4 cases, 8%), tetany or paresthesia (3 cases, 6%).
All patients diagnosed with XLHR and Fanconi syndrome (3 cystinosis and one mitochondrial disease) had bone lesions of rickets at the beginning and those with FHHNC and HHRH started with nephrocalcinosis.
At the beginning of the disease, extrarenal manifestations were frequent. Seven patients presented ocular involvement: 3 patients cystine deposits corresponding to those diagnosed with cystinosis, 2 cases with LS had congenital cataracts, one case of bilateral corneal edema in one of the mitochondrial diseases, in which investigation of associated renal involvement revealed hyperaminoaciduria, and, finally, chorioretinitis was observed in one of the patients with FHHNC. Four out of the 8 patients (50%) diagnosed with DRTA had hearing loss. The epidermal growth factor receptor defective tubulopathy showed severe generalized alopecia and erythroderma that evolved poorly, and it was resistant to treatment.
The most representative laboratory values presented at the diagnosis of the most prevalent tubulopathies, shown in Table 1, are detailed below. The data corresponding to the children with cystinuria are not included since they only presented increased urinary excretion of dibasic amino acids.
- -
GS. Venous blood gases: pH 7.47 ± 0.70; bicarbonate 29.12 ± 4.43 mEq/l. Serum biochemistry: potassium 2.55 ± 0.39 mEq/l; Chloride: 98.13 ± 4.42 mEq/l; magnesium: 1.40 ± 0.36 mg/dl. Urine biochemistry: fractional excretion of potassium: 23.61 ± 12.09%; fractional excretion of magnesium: 6.37 ± 1.92%; ratio calcium/creatinine 0.02 ± 0.02 mg/mg.
- -
DRTA. Venous blood gases: pH 7.22 ± 0.10; bicarbonate 12.4 ± 3.4 mEq/l. Serum biochemistry: potassium 2.78 ± 0.93 mEq/l; Chloride: 113.38 ± 7.35 mEq/l. Urine biochemistry: urinary pH Minimum: 6.81 ± 0.38; ratio calcium/creatinine 0.53 ± 0.24 mg/mg.
- -
XLHR. Serum biochemistry: phosphorus: 259 ± 0.34 mg/dl; Calcium: 9.60 ± 0.54 mg/dl; alkaline phosphatase: 916.12 ± 176.01 U/l; parathyroid hormone: 36.50 ± 31 pg/ml; calcidiol: 44.28 ± 17.79 ng/ml. Urine biochemistry: tubular reabsorption of phosphate 66 ± 13%.
- -
Cystinosis Venous blood gases: pH 7.33 ± 0.01; bicarbonate 17.7 ± 2 mEq/l. Serum Biochemistry: Uric acid: 1.2 ± 0.4 mg/dl; magnesium 2.19 ± 0.1 mg/dl; phosphorus 2.50 ± 0.62 mg/dl; alkaline phosphatase 1249.67 ± 35.23 U/l. Urine biochemistry: tubular reabsorption of phosphate 56.01 ± 22.50%; ratio calcium/creatinine 0.08 ± 0.07 mg/mg; protein/creatinine ratio 2.23 mg/mg.
Data related to the patients genetic study is shown in Table 2.
Primary tubulopathies. Genetic study.
| Renal tubulopathy N.º (mutation found/genetic study carried out) | Findings |
|---|---|
| Gitelman syndrome | -Homozygosity. Gen SLC12A3: c.1177 + 1 G > T, splicing: 15/19 |
| 18/18 ª | -Heterozygosis. Gene SLC12A3. c.2954 G > A; p.Cys985Tyr/ no second variant: 1/19 |
| -Compound heterozygosity. Gene SLC12A3: c.1177 + 1 G > T, splicing/c.20_21delCA; p.Thr7ArgfsStop22: 1/19 | |
| -Compound heterozygosity. Gene SLC12A3: c.1142C > T; p. Thr381Met/c.2982 C > A; p.Cys994Stop: 1/19 | |
| DRTA | -Homozygosity. Gen ATP6V1B1: c.581 + 1 G > A, splicing: 3/8 |
| 5/8 | -Compound heterozygosity. Gen ATP6V1B1: c.581 + 1 G > A, splicing/c.1075 G > A; p.Glu330Lys: 1/8 |
| -Compound heterozygosity. Gen ATP6V0A4: c.581 + 1 G > A, splicing/c.1075 G > A; p. Glu330Lys: 1/8 | |
| -Heterozygosis. Gene ATP6V0A4. c.1188insA; p.Tyr 396Stop/no second variant: 1/8 | |
| -Homozygosity. Gen ATP6V1B1: c.91C > T; Arg31Stop: 1/8 | |
| -Heterozygosis. Gen ATP6V1B1: c.1181 G > A; Arg394Gln/no second variant: 1/8 | |
| XLHR | -Heterozygosis. Gen PHEX: c.871C > T; p. Arg291Stop: 3/4 |
| 4/4 | -Heterozygosis. Gen PHEX: c.1404 G > C; p.Lys468Asn: 1/4 |
| Cystinosis | -Homozygosity. Gen CTNS: indel 57 kb: 3/3 |
| NDI | -Homozygosity. Gen AVPR2: c.877 T > G; p.Trp293Gly. Family |
| 1/1ªt | |
| Dent disease | - Point mutacion (Y140X) in CLCN5 gene. Family |
| 2/2 | - Hemizigosis CLCN5 gene of exon 2−12. De novo or familiar |
| Lowe syndrome | -Heterozygosis. Gen OCRL1: c.1666 A > T; p.Arg556Stop. |
| 1/1ª | |
| FHHNC | -Homozygosity. Gen CLDN19: c.59 G > A; p.Gly20Asp |
| 1/1ª | |
| MD | -mitDNA. 5.6Kb From |
| 1/1ª | |
| Gordon syndrome | -Heterozygosis. Gen WNK1: c.1888A > G p.E630G |
| 1/1 | |
| FCE receptor defect | -Homozygosity. Gen EGFR: c.1283 G > A; p.G428D |
| 1/1 | |
| HHRH | -Heterozygosis. Gene SLC34A3: c.232 G > A; p.Gly78Arg/no second variant |
| 1/1 |
DRTA: distal renal tubular acidosis; NDI: nephrogenic diabetes insipidus; DD: Dent's disease; MD: mitochondrial disease; EGF: epidermal growth factor; FHHNC: hypomagnesemia with hypercalciuria and nephrocalcinosis; N.º: number of cases; HHRH: hypophosphatemic rickets with hypercalciuria; XLHR: X-linked hypophosphatemic rickets; LS: Lowe syndrome.
In 3 patients the study could not be updated. Two 2 of them died, one with LS due traffic accident at the age of 6 and another with GS due to unknown causes at the age of 35 and, a third patient with HHNC was lost the follow-up after being discharged from our unit at the age of 18. Patients received mineral and/or electrolyte supplements as treatment, depending on their underlying tubulopathy. In addition, hormonal treatments were established if necessary: active vitamin D in XLHR and in patients with Fanconi syndrome, thyroxine in cystinosis, recombinant human growth hormone (rhGH) in those with persistent reduction of growth, as detailed below. All patients with cystinosis also received cysteamine as a cystine depleting agent since it became available for administration.
Table 3 shows the evolution of the biochemistry in those tubulopathies with at least 3 cases diagnosed. The mean follow-up period was 18.92 (6.26–24.33) years. The values from of the last follow-up biochemistry are detailed below.
- -
GS. Venous blood gases: pH 7.44 ± 0.5; bicarbonate 29.56 ± 2.83 mEq/l. Serum biochemistry: potassium 2.90 ± 0.35 mEq/l; Chloride 97.08 ± 3.55 mEq/l; magnesium 1.42 ± 0.33 mg/dl. Urine biochemistry: fractional excretion of potassium 15.67 ± 10.04%; fractional excretion of magnesium 7.18 ± 4.01%; Calcium/creatinine ratio 0.10 ± 0.13 mg/mg.
- -
DRTA. Venous blood gas pH 7.33 ± 0.03; bicarbonate 23.08 ± 2.69 mEq/l. Biochemistry serum: potassium 4.16 ± 0.23 mEq/l; chloride: 103.75 ± 2.96 mEq/l; anion gap in blood 18.70 ± 3.16. Urine biochemistry: Urine anion gap 64.25 ± 27.41; urinary calcium/creatinine ratio 0.16 ± 0.05 mg/mg.
- -
XLHR. Serum biochemistry: phosphorus 2.46 ± 1.03 mg/dl; calcium: 9.57 ± 0.63 mg/dl; alkaline phosphatase 174.01 ± 149.89 U/l; Parathyroid hormone 95.00 ± 45.61 pg/ml; calcidiol 44.42 ± 9.88 ng/ml. Urinary biochemistry: tubular reabsorption of phosphate 78.39 ± 19.94%; urinary ratio calico/creatinine 0.05 ± 0.04 mg/mg.
- -
Cystinosis Venous blood gases: pH 7.40 ± 0.03; bicarbonate 26.3 ± 0.49 mEq/l. Serum biochemistry: Uric acid 4.56 ± 264 mg/dl; magnesium 1.94 ± 0.29 mg/dl; phosphorus 2.50 ± 0.62 mg/dl; alkaline phosphatase: 242.00 ± 314.39 U/l. Urine Biochemistry: tubular phosphate reabsorption 61.06 ± 9.49%; urine calcium/creatinine ratio 0.10 ± 0.17 mg/mg.
Primary tubulopathies. Follow-up data in the total series and in the most prevalent diseases, with 3 or more children.
| Renal tubulopathy | N.º | Median current age in years (IQR) | Median current follow-up in years (IQR) | eGFR < 90 ml/ min /1.73 m2 N.º (%) | Nephrocalcinosis N.º (%) |
|---|---|---|---|---|---|
| Global serie | 50 | 22.09 (13.56−31.65) | 18.92 (6.25−24.33) | 16 (32) | 16 (32) |
| GS | 18 | 17.63 (12.96–29.06) | 8.58 (3.04−22.13) | 2 (11) | 0 (0) |
| DRTA | 8 | 23.67 (16.65−33.23) | 20.63 (15.75−32.88) | 4 (50) | 8 (100) |
| Cystinuria | 6 | 24.83 (16.92−37.88) | 20.33 (16.63−25.67) | 2 (33) | 0 (0) |
| XLHR | 4 | 39.17 (27.79−46.83) | 36.13 (26.65−41.08) | 0 (0) | 3 (75) |
| Cystinosis | 3 | 26.17 (17.54−32.33) | 23.42 (15.75−29.42) | 2 (67) | 3 (100) |
DRTA: distal renal tubular acidosis; EGFR: estimated glomerular filtration rate; N.º: number of cases; XLHR: X-linked hypophosphatemic rickets; IQR: interquartile range; GS: Gitelman syndrome.
Table 4 shows data related to the evolution of growth. The final height was 162.6 ± 9.4 cm for 31 adult patients throughout the series. The comparison of the final height reached in each group of patients in relation to the one genetically determined was as follows. GS, 9 patients, final height 171.4 ± 12.6 and 159.4 ± 3.9 cm for males and females vs. such corresponding genetic 172.9 ± 7.2 and 163.6 ± 2.6 cm, respectively. DRTA, 6 patients, final height 166.7 ± 5.3 cm and 163.0 ± 2.5 cm for men and women vs. Corresponding genetic height of 167.8 ± 14.1 and 164.4 ± 3.3 cm, respectively. XLHR, 3 women, final height 152.6 ± 2,2 cm vs. Estimated height genetic 158.8 ± 1.44 cm.
Primary tubulopathias. Growth in the total series and in the most prevalent diseases, with 3 or more children.
| Renal Tubulopathy | At diagnosis | Last follow-up | RhGH treatment (%) | ||
|---|---|---|---|---|---|
| Low growth (%) | Height (Mean ± SD) | Low growth (%) | Height (Mean ± SD) | ||
| Global series | 20/53 (38) | −1.39 ± 1.49 | 14/53 (26) | 1.07 ± 1.54 | 7/53 (13) |
| GS | 5/19 (26) | −0.90 ± 1.28 | 3/18 (16) | −0.75 ± 1.32 | 1/19 (5) |
| DRTA | 4/8 (50) | −1.85 ± 2.09 | 3/8 (38) | −0.60 ± 2.01 | 1/8 (13) |
| Cystinuria | 0/0 (0) | −0.16 ± 0.64 | 0/0 (0) | 0.23 ± 0.2 3 | 0/6 (0) |
| XLHR | 3/4 (75) | −2.42 ± 0.52 | 2/4 (50) | −1.71 ± 0.53 | 1/4 (25) |
| Cystinosis | 3/3 (100) | −2.67 ± 0.83 | 1/3 (33) | −2.28 ± 1.08 | 3/3 (100) |
DRTA: distal renal tubular acidosis; SD: standard deviation; rhGH: human recombinant growth hormone; XLHR: X-linked hypophosphatemic rickets; GS: Gitelman syndrome.
The number of cases with impaired growth is shown, defined by height less than −2 SD of the reference values for a population of the same age and gender, with respect to the number in corresponding group.
As shown in Table 3, 16 patients (32%) had a GFR < 90 ml/min/1.73 m 2 maintained during their follow-up. Eight patients had an eGFR between 60−89 ml/min/1.73 m2 (2 cases had GS, 3 cases DRTA, one case HHRH, one case of mitochondrial disease and one of FHHNC), 4 patients had between 30−59 ml/min/1.73 m2 (one had DRTA, one case of LS, 2 cystinuria cases ), one case had between 16−29 ml/min/1.73 m2 (a case of FHHNC), 3 patients with end-stage renal disease had required renal replacement therapy for end-stage renal failure (2 cases with cystinosis had received kidney transplants and one with DD was in the peritoneal dialysis prior to transplantation). Table 3 shows the data for the most prevalent tubulopathies.
Other complicationsThroughout its evolution, and both during pediatric age and in adulthood, 11 patients presented metabolic emergencies that required hospital admissions and/or treatment with intravenous electrolyte administration. Seven of these patients had GS and developed severe hypokalemia in the context of episodes of acute gastroenteritis or asthma treated with salbutamol. A patient with Fanconi syndrome due to mitochondrial disease presented several crises of hypokalemia, rhabdomyolysis, and acute renal failure. Three of the patients with GS had syncope of unclear cause and 2 developed severe thyroid abnormalities.
Nine patients had episodes of nephritic colic and/or kidney stones: 4 with DRTA, 2 with cystinuria, one with HHRH, one case with FHHNC, one case with DD. Two patients with cystinuria required surgical interventions to remove kidney stones.
Six patients with DRTA presented sensorineural deafness, 5 were preschool age, 5 of them wearing hearing aids. None of the patients with XLHR had hearing loss.
The 3 patients diagnosed with cystinosis presented cystine crystals in the cornea with loss of visual capacity. The 2 cases of LS were underwent surgery for congenital cataracts.
One case of cystinosis was operated on after finishing its growth for keel thorax and for lower limb elongations. Two women with RHLX developed heel spurs and one underwent orthopedic surgery.
Disorders of mental adaptation, depression and/or anxiety were observed in 10 patients. A patient diagnosed with mitochondrial disease developed deafness and demyelination at the supratentorial, trunk and diencephalon levels, bilateral palpebral ptosis with partial external ophthalmoparesis. The patient with SL presented a delay of maturation with associated epileptic seizures.
DiscussionOur study analyzes 53 patients with different primary tubulopathies, mostly genetically confirmed, in a specific geographic area. The study provides original data about the clinical presentation and its long-term evolution. Although the primary tubulopathies comprise different diseases, the joint analysis of the sample is of interest since many of them share similar biochemical and clinical manifestations, such as alterations in the acid-base balance, salt loss, electrolyte abnormalities, etc. and bone and growth impairment, polyuria, urolithiasis, nephrocalcinosis, extrarenal pathology, etc. Thus, on many occasions there are difficulties with the differential diagnosis, which are increased because all of them are rare diseases and therefore there is little experience in each institution. Likewise, the long-term course of primary tubulopathies is largely unknown.
The design of our study does not provide accurate data on the prevalence of tubulopathies but confirms that are rare or very rare diseases and that the GS is the most prevalent, consistent with data recently reported in a large European cohort multicentric study.8 Although it is expected that a high percentage of patients with GS will be diagnosed in adulthood9–11 or even go unnoticed, our data show a high number of pediatric-onset cases, a finding partially justified by the high frequency of this disease in a population of gypsy ethnicity and because the diagnosis of the disease was made in asymptomatic relatives. Regarding the XLHR, the data in the literature point to a prevalence of 1/20,000 live births,12–14 a frequency that does not match the number of cases in our series. It is possible that XLHR is underdiagnosed as has been described in other European areas,13,14 probably related with the highly variable clinical spectrum of the disease and the existence of cases with mild clinical expression.15,16 A 25% of the cases were even more rare tubulopathies with a frequency consistent with the epidemiological reports.17,18
It is noteworthy that the series does not include cases of Bartter syndrome. The explanation for this fact could be that in geographically limited territories (islands, mountain areas with limited capacity of transportation)19 the appearance of genetic drift phenomena can condition the selection of a specific genetic scenario and, therefore, of primary diseases. Bartter syndrome type 3 and GS may present similar clinical manifestations and may lead to diagnostic errors,8,20 but in our cohort this does not seem to be the explanation since most patients had genetic confirmation. Other forms of Bartter syndrome would be serious enough not to go unnoticed.
Clinical and metabolic decompensation was the most frequent presentation followed by limited growth (Table 1). These findings, although generally known,21 confirm the need to rule out the diagnosis of underlying tubulopathy in a young child with severe, recurrent, or difficult to correct alterations of acid-base and/or fluid and electrolyte balance with the usual therapeutic measures. Similarly, failure to thrive and growth impairment are common manifestations of primary tubulopathies and a reason for consultation that leads to diagnosis. Radiological alterations such as nephrocalcinosis, urolithiasis, and rickets lesions correspond to some groups of tubulopathies. It is also noteworthy that family screening is a growing reason for diagnosis, there is more knowledge about the mode of transmission of tubulopathies and a greater availability of genetic studies. It is hoped that early diagnosis can facilitate the best follow-up of patients and reduce acute and long-term complications. However, the absence of a gene alteration does not exclude the presence of primary tubulopathy since, with current techniques, the genetic defect is not found in a 15–20% of cases.8,22
Our results (Table 1) indicate that in general the primary tubulopathies are pediatric entities that exhibit clinical symptoms during the first years of life and without predominance by sex. This statement is biased by the study design as no cases of adult-onset were included. The early identification of asymptomatic cases by family study also implies an early diagnosis before the beginning of manifestations. Data from the literature indicate that cystinuria more frequently begins in the second decade of life23 and it is also known that GS is a late diagnosis entity, in adulthood, in a high percentage of patients. In this regard, it is notable that more than 90% of the patients diagnosed with GS had a confirmatory genetic study and all the gypsy patients carried the same intron 9 + 1 G > T24 mutation (Table 2). Other ethnic groups with similar mutations have been described, such as: the p.Arg642Cys mutation in the Japanese population,9 the p.Thr60Met mutation in people from China25 and the p.Ser402X in those from Italy.26 In our series, a pathogenic mutation was detected in the PHEX gene in all patients diagnosed with XLHR, a higher percentage than that usually reported in the literature,27–29 25% of them of family origin and 75% de novo.
Another interesting contribution of the present study is the information on long-term follow-up, an aspect on which there are very few publications.1,30–32Table 3 shows follow-up data up to young adults, almost 2 decades, of patients diagnosed with primary tubulopathies during childhood. It should be noted that a third of the cases presented a GFR < 90 ml/min/1.73 m2. This was known in diseases such as cystinosis, and in some other diseases such as metabolic diseases, and has recently been described in patients with DRTA.32 Our study shows that 50% of young adults with DRTA had a GFR < 90 ml/min/1.73 m2, emphasizing the need to control the glomerular filtration in the monitoring of these patients. Likewise, up to 11% of patients with GS had a decrease in eGFR at a mean age of 20, with evident clinical implications for the control of these patients. Table 3 also shows that all patients with DRTA or cystinosis had nephrocalcinosis, a characteristic finding in these diseases and already present at diagnosis.33 However, the high percentage of patients with XLHR who developed nephrocalcinosis is presumably related to treatment with phosphate and vitamin D metabolites.30,34 Ultrasound is a very sensitive technique for the diagnosis of nephrocalcinosis. The practical significance of this finding is questionable, since it has not been related to the appearance of symptoms or clinical signs in patients with XLHR, it is not the cause of kidney failure in cystinosis nor does it seem to be responsible for the decrease in glomerular filtration in DRTA. Our study also confirms that medical treatment does not correct the metabolic alterations in patients with primary tubulopathies, nor does it prevent many of their extrarenal complications. The need for treatment and adherence to it should be emphasized, as well as the importance of maintaining follow-up when pediatric patients are transferred to adult units,35–37 however it is also necessary to keep in mind and monitor the potential adverse effects of medication.
The present study demonstrates the growth impairment as a prevalent manifestation of tubulopathies, a fact that was already known,9,21,32,38 and its improvement with treatment and adequate follow-up (Table 4). It should be noted that the initial impairment of growth was found to be particularly important in children with DRTA XLHR and cystinosis. The impairment in growth was reverted to near-average height values in patients with DRTA, the XLHR patients only improved partially and it was barely modified in patients with cystinosis. These data are compatible with the recovery of growth induced by the normalization of serum bicarbonate levels in DRTA,32 and with the beneficial but insufficient effect of conventional treatment with phosphate supplements and derivatives of vitamin D in XLHR15,39,40 and with the severity of undergrowth in cystinosis, the innate metabolic error that most affects growth in height.38,41 The analysis of our series also provides data on final adult height in patients with primary tubulopathies, information that is scarcely reported in the literature42–44 and also shows that 13% of patients required administration of rhGH, although in our country tubulopathies are not officially accepted as a therapeutic indication for rhGH.
In summary, this work offers relevant data on the diagnostic and evolutionary characteristics of primary tubulopathies confirmed by genetic analysis in most cases. It shows that they are rare diseases, with GS being the most common childhood-onset tubulopathy. These primary tubulopathies are heterogeneous, but sharing both initial and evolutionary clinical and analytical manifestations. It emphasizes the importance of growth impairment in these entities and its degree of reversibility according to primary nephropathy, as well as the need for rhGH administration in some cases. In addition, our study provides information on long-term follow-up of patients with primary tubulopathies diagnosed in pediatric age, highlighting the possibility of episodes of metabolic decompensation and the presence of extrarenal complications and alerts about the high risk of developing glomerular renal failure.
FundingInstituto de Salud Carlos III. Proyecto PI 17/01745.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Blázquez Gómez CJ, Gil-Peña H, Álvarez FO, Rodríguez FS. Evolución de tubulopatías renales primarias diagnosticadas en edad pediátrica. Nefrologia. 2021;41:182–190.