The most important complication of kidney biopsy is bleeding, and it is unclear whether desmopressin is effective in preventing it. Thus, the study was conducted to compare post-biopsy bleeding with or without desmopressin prescription prior to percutaneous kidney biopsy.
MethodsIn this single-centered, retrospective, and observational study, 3,018 adult patients who underwent kidney biopsy between January 1, 2003 and March 31, 2019 at our institute were recruited. Of these, 776 patients received desmopressin. To compare the differences in major bleeding events between patients administered and not administered with desmopressin, propensity score matching was performed.
ResultsBefore propensity score (PS) matching, it was observed that patients in the desmopressin group were significantly older (p<0.001) and had a higher blood pressure (p<0.001), higher serum creatinine (p<0.001), lower hemoglobin levels (p<0.001), and lower platelet counts (p=0.001) than those in the no-desmopressin group. Furthermore, the incidence of renal artery embolization was not significantly different between the two groups (p=0.077); however, blood transfusions occurred significantly more frequently in the desmopressin group (p<0.001). A comparison of the two groups after PS matching did not reveal any differences in the incidence of renal artery embolization (p=0.341), blood transfusion (p=0.579), and total major bleeding events (p=0.442). Furthermore, there was no difference in the incidence of perinephric hematoma on computed tomography or ultrasound (p=0.120).
ConclusionsWe do not recommend desmopressin administration before kidney biopsy.
La complicación más importante de la biopsia renal es la hemorragia y no está claro si la desmopresina es eficaz en su prevención. Por lo tanto, el estudio se realizó para comparar la hemorragia tras una biopsia renal percutánea con o sin prescripción de desmopresina previa a esta.
MétodosEn este estudio unicéntrico, retrospectivo y observacional se seleccionaron 3.018 pacientes adultos que se sometieron a una biopsia renal entre el 1 de enero de 2003 y el 31 de marzo de 2019 en nuestro instituto. De ellos, 776 pacientes recibieron desmopresina. Para comparar las diferencias en los acontecimientos de hemorragia mayor entre los pacientes que recibieron desmopresina y los que no, se realizó un emparejamiento por puntuación de propensión.
ResultadosAntes del emparejamiento por puntuación de propensión, se observó que los pacientes del grupo con desmopresina tenían una edad significativamente mayor (p<0,001) y presentaban una presión arterial más alta (p<0,001), una creatinina sérica más alta (p<0,001), niveles de hemoglobina más bajos (p<0,001) y recuentos de plaquetas más bajos (p=0,001) que los del grupo sin desmopresina. Además, la incidencia de embolización de la arteria renal no fue significativamente diferente entre los 2 grupos (p=0,077); sin embargo, las transfusiones de sangre se produjeron con una frecuencia significativamente mayor en el grupo con desmopresina (p<0,001). Una comparación de los 2 grupos tras el emparejamiento por puntuación de propensión no reveló diferencias en la incidencia de embolización de la arteria renal (p=0,341), la transfusión de sangre (p=0,579) y los acontecimientos de hemorragia mayor totales (p=0,442). Además, no se observaron diferencias en la incidencia de hematomas perinéfricos en la tomografía computarizada o la ecografía (p=0,120).
ConclusionesNo se recomienda la administración de desmopresina antes de una biopsia renal.
Percutaneous kidney biopsy is an important modality for diagnosing and treating glomerular disease. Complications in biopsies can be major (those that require interventions such as a blood transfusion or procedure to stop bleeding) and minor (those that do not require special interventions, for e.g., hematuria or perinephric hematoma).1
Desmopressin is a long-acting synthetic analog of vasopressin, and was originally designed to treat diabetes insipidus.2 It is now used to treat bleeding disorders as well, because it can induce an increase in the plasma levels of factor VIII and the von Willebrand factor, thereby shortening the prolonged activated partial thromboplastin time (aPTT) and the bleeding time.3
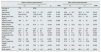
The effect of desmopressin on the risk of post-kidney biopsy bleeding remains controversial (Table 1). Two studies revealed that desmopressin decreased the bleeding risk,4,5 while one study revealed that it did not decrease the bleeding risk.6 Two additional studies also reported controversial results.7,8
Summary of studies on the effects of desmopressin on post-kidney biopsy bleeding.
| Study ID | Number of patients | Study design | Results |
|---|---|---|---|
| Manno et al.4 (2011) | 162 patients undergoing native kidney biopsy | Randomized, controlled, single-center study; Italy | Desmopressin significantly decreased post-biopsy bleeding (13.7% vs. 30.5%, p=0.01). |
| Radhakrishnan et al.6 (2014) | 43 patients (22 with native kidney biopsy and 21 with central line placement) | Retrospective single-center study; Canada | No difference in the bleeding complications between desmopressin and no-desmopressin groups (23% vs. 27%, p=1.0). |
| Peters et al.5 (2018) | 576 patients with serum creatinine above 150μmol/L (≥1.7mg/dl) undergoing native kidney biopsy | Most prospective multicenter study; Sweden | Multiple logistic regression revealed that desmopressin showed lesser major (OR: 0.38) and overall complications (OR: 0.36). |
| Athavale et al.7 (2019) | 269 patients undergoing percutaneous kidney biopsy | Retrospective single-center study; United States of America | Desmopressin decreased bleeding risk in patients with serum creatinine ≥1.8mg/dL (OR: 2.11, p=0.09), but increased the risk when serum creatinine was <1.8mg/dL (OR: 9.72, p<0.001). |
| Leclerc et al.8 (2020) | 413 patients undergoing native kidney biopsies | Retrospective single-center study; Canada | Despite a higher bleeding risk, patients using desmopressin had a similar likelihood of symptomatic hematomas (OR: 0.39) and a lower need for urgent radiologic studies (OR: 0.33). |
| Cheong et al. | 3018 patients undergoing native kidney biopsy | Retrospective single-center study; South Korea | No differences in the incidence of renal artery embolization (p=0.341), blood transfusion (p=0.579), and total major bleeding events (p=0.442). |
We previously reported that intravenous desmopressin significantly reduced the level of collagen/epinephrine and collagen/adenosine diphosphate closure time in uremic patients.2 We also reported that a single injection of desmopressin prior to invasive procedures in uremic patients using antiplatelet agents ameliorated platelet dysfunction (measured by in vitro collagen/epinephrine occlusion time).9 Based on these studies, over the past 17 years, we have administered desmopressin to some patients prior to kidney biopsy.
This study was performed to compare major post-biopsy bleeding between patients who were prescribed with desmopressin prior to percutaneous kidney biopsy and patients who were not.
Material and methodsPatientsA retrospective single-center study was conducted to compare the incidence of severe post-kidney biopsy bleeding between adult patients who were administered with desmopressin and patients who were not. Patients who underwent kidney biopsy at our institute from January 1, 2003 to March 31, 2019 were included. The exclusion criteria were as follows: (1) transplanted kidney biopsy (when kidney transplant was performed a day prior to the kidney biopsy or kidney transplant disease codes were available), (2) open kidney biopsy, (3) age <18 years at the time of kidney biopsy, and (4) mass biopsy for cancer diagnosis. A search using our center's Biomedical Research Environment revealed that 6877 patients underwent a kidney biopsy during the period specified above. Among these, 6518 patients were aged 18 years or above. After excluding for transplant kidney biopsy and open kidney biopsy, 4051 patients were identified; of these, 3018 patients were selected as the final study subjects. The patient‘s informed consent was not necessary because the data obtained was collected from clinical practice.
Data collectionThe following data were collected:
- 1.
Desmopressin administration: Yes/No
- 2.
Consumption of anticoagulants or antiplatelet drugs before kidney biopsy: Yes/No
- 3.
Baseline characteristics at the time of kidney biopsy: age, sex, weight, height, and body mass index (BMI)
- 4.
Comorbidities: diabetes mellitus, hypertension
- 5.
Blood pressure just before and after the kidney biopsy
- 1)
Systolic blood pressure (SBP) (mmHg)
- 2)
Diastolic blood pressure (DBP) (mmHg)
- 3)
Mean arterial pressure (MAP) (mmHg)
- 1)
- 6.
Blood and urine test results obtained just before and after the kidney biopsy
- 1)
Hemoglobin (g/dL), platelet (×103/μL), hematocrit (%)
- 2)
Prothrombin time (PT international normalized ratio [INR]), activated partial thromboplastin time (sec)
- 3)
Serum creatinine (mg/dL), estimated glomerular filtration rate (eGFR) (ml/min/1.73m2), blood urea nitrogen (BUN) (mg/dL)
- 4)
Spot urine albumin/creatinine ratio (g/g), spot urine protein/creatinine ratio (g/g)
- 1)
- 7.
Kidney biopsy data
- 1)
Number of needle passes, number of biopsy segments
- 2)
Clinical indication for kidney biopsy
- (i)
Hematuria and/or non-nephrotic range proteinuria
- (ii)
Azotemia
- (iii)
Nephrotic syndrome
- (i)
- 3)
Histological diagnosis
- (i)
Glomerulonephritis
- (ii)
Nephrosclerosis
- (iii)
Tubulo-interstitial nephritis
- (iv)
Lupus nephritis
- (v)
Diabetic nephropathy
- (vi)
Vasculitis
- (vii)
Amyloidosis
- (viii)
Others
- (i)
- 4)
Department that performed biopsy
- (i)
Nephrology
- (ii)
Rheumatology
- (iii)
Allergy
- (iv)
Others
- (i)
- 1)
- 8.
Bleeding events
- (1)
Renal artery embolization
- (2)
Blood transfusion (limited to red blood cell transfusion)
- (3)
Perinephric hematoma on computed tomography (CT) or ultrasound (US), Size of the hematoma
- (4)
Nephrectomy due to bleeding
- (5)
Length of hospital stay
- (1)
The eGFR presented in our electronic medical record was estimated using the modification of diet in renal disease (MDRD) equation (MDRD eGFR) and the chronic kidney disease epidemiology collaboration (CKD-EPI) equation (CKD eGFR). In the old data at our institute, it was often expressed as either MDRD eGFR or CKD-EPI eGFR alone. The difference between the two was considered insignificant and the two data were applied together and used to evaluate eGFR statistics. If data for the computation of both were available, then the MDRD equation (which has data from more patients) was applied.
In order to identify bleeding events, cases where renal artery embolization and blood transfusion were performed within 7 days from the biopsy were investigated. Furthermore, in cases where CT or US was performed within 7 days from the biopsy, the presence of perinephric hematoma was investigated. Hematoma size data were included only when it was described in the official reading. The major bleeding events were defined as cases that underwent renal artery embolization and blood transfusion.
Biopsy procedure and desmopressin administrationIn all kidney biopsies, patients were provided with a detailed explanation of the protocol and informed consent was obtained. Prior to the procedure, the patient's complete blood count (CBC) and coagulation profile were checked. Transfusions were recommended for patients with hemoglobin levels lower than 10g/dL or with platelet counts lower than 100,000/μL. Patients who consumed anticoagulants or antiplatelet drugs prior to kidney biopsy underwent a period of discontinuation. Furthermore, aspirin and clopidogrel consumption was skipped for 7 days, cilostazol for 3 days, and warfarin until the PT INR was normal.
There was no standardized hospital protocol for the administration of desmopressin in this study. Desmopressin was administered to subjects who were deemed to have a high risk of bleeding by the attending physician; these subjects were typically those with a known high risk of bleeding, i.e., patients with impaired renal function and elevated BUN, old age, high blood pressure, low hemoglobin levels, and low platelet counts. Patients in the desmopressin group received a dose of 0.3μg/kg desmopressin (Minirin®, Ferring, Saint-Prex, Switzerland) in 100cc normal saline 30min before the procedure.
A 16- or 18-gauge semiautomated, side-notch disposable biopsy needle was used for the biopsy (STARCUT®, TSK Laboratory, Tochigi, Japan). To reduce the risk of bleeding, 18-gauge needles (9–12cm in length) were used in most cases.10 By using needles of a gauge thinner than that of the usual ones, the risk of bleeding was reduced. Therefore, even in patients with a relatively high bleeding tendency, punctures were repeated several times to obtain sufficient tissue. For native kidney biopsy, we aimed to collect more than 25 glomeruli and obtain an average of about three segments. The biopsies were conducted using real-time ultrasound guidance. After the procedure, a sandbag was placed on the biopsy site for 3h and the patient rested in a supine position. Then, after being transferred to the ward, the blood pressure and pulse rate were measured periodically, and the CBC was checked the next morning. If vital signs became unstable or other bleeding complications, such as gross hematuria or severe abdominal pain, were detected, CT or US was performed and renal artery embolization and blood transfusion were undertaken as required. CT or US was not performed routinely after kidney biopsy in patients without any symptoms.
Ethics statementsThis study was conducted in accordance with the ethical standards of the Declaration of Helsinki (as revised in Brazil, 2013). This research protocol was approved by the Institutional Review Board of our institute (No. 2019-0427).
Statistical analysisWhen numerical data satisfied normality, they were expressed as mean±standard deviation, and a Student's t-test was performed to compare the means of the two independent groups. The chi-square test and Fisher's exact test were performed to compare categorical data between the two groups. The frequency of occurrence was expressed as a percentage (%). To compare the difference according to whether desmopressin was administered or not, propensity score matching (PS matching) was performed. After performing multiple imputations, the average of PSs estimated from each completed dataset was used. In case of a 2:1 or 3:1 matching, several patients in the desmopressin group were lost; thus, a 1:1 matching was performed. Post-matching outcome comparison was performed using logistic regression, with correlation allowed within the matching pair and a robust estimator. PS matching was performed using the R software, version 3.6.1, while the remaining tests were performed using IBM SPSS Statistics for Windows, version 23 (IBM Corp., Armonk, N.Y., USA). In addition, p<0.05 was considered statistically significant.
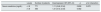
ResultsComparison of baseline characteristics before kidney biopsyThere were no significant differences in the weight, height, and BMI between the two groups; however, the age was significantly higher in the desmopressin group than in the no-desmopressin group (p<0.001). Furthermore, the SBP, DBP, and MAP were also significantly higher in the desmopressin group than in the no-desmopressin group (p<0.001). The hemoglobin, platelet, and hematocrit levels were significantly lower in the desmopressin group than in the no-desmopressin group (p<0.001, p=0.001, and p<0.001, respectively). The PT (p<0.001) and aPTT (p=0.025) were significantly higher in the desmopressin group than in the no-desmopressin group. Serum creatinine and BUN were significantly higher (p<0.001), while eGFR was significantly lower (p<0.001) in the desmopressin group than in the no-desmopressin group. The urine protein/creatinine ratio (p=0.007) was also significantly higher in the desmopressin group than in the no-desmopressin group. The use of anticoagulants or antiplatelet drugs before renal biopsy was significantly more in the desmopressin group as compared to in the no-desmopressin group (p<0.001) (Table 2).
Baseline characteristics before kidney biopsy and kidney biopsy information.
| Desmopressin group | No-desmopressin group | p | |
|---|---|---|---|
| N=776 (25.7%) | N=2242 (74.3%) | ||
| Age (years) | 50.2±16.8 | 43.5±16.1 | <0.001 |
| Men/women (women %) | 432/344 (44.3%) | 1087/1155 (51.5%) | 0.001 |
| Weight (kg) | 64.2±12.6 | 64.1±13.0 | 0.869 |
| Height (cm) | 163.9±8.9 | 163.7±9.1 | 0.690 |
| Body mass index (kg/m2) | 23.9±3.6 | 23.8±3.8 | 0.581 |
| Systolic blood pressure (mmHg) | 126±19 | 121±17 | <0.001 |
| Diastolic blood pressure (mmHg) | 79.6±11.7 | 77.3±10.8 | <0.001 |
| Mean arterial pressure (mmHg) | 95.1±12.9 | 91.9±11.9 | <0.001 |
| Blood parameters | |||
| Hemoglobin (g/dL) | 11.3±2.6 | 12.6±2.3 | <0.001 |
| Platelet (×103/μL) | 243±93 | 256±82 | 0.001 |
| Hematocrit (%) | 33.7±7.4 | 37.7±6.4 | <0.001 |
| Prothrombin time (INR) | 1.02±0.11 | 0.98±0.09 | <0.001 |
| aPTT (sec) | 29.2±5.8 | 28.6±4.3 | 0.025 |
| Serum creatinine (mg/dL) | 2.87±2.68 | 1.24±1.25 | <0.001 |
| eGFR (ml/min/1.73m2) | 45.0±34.5 | 73.6±28.2 | <0.001 |
| BUN (mg/dL) | 33.5±22.9 | 19.3±13.1 | <0.001 |
| Spot urine tests | |||
| Urine albumin/creatinine ratio (g/g) | 1.8 (0.5, 4.5) | 1.5 (0.5, 3.9) | 0.161 |
| Urine protein/creatinine ratio (g/g) | 2.4 (1.0, 5.8) | 1.7 (0.7, 4.1) | 0.007 |
| Comorbidities | |||
| Diabetes mellitus | 202 (26.0%) | 233 (10.4%) | <0.001 |
| Hypertension | 315 (40.6%) | 637 (28.4%) | <0.001 |
| Anticoagulant/antiplatelet use before biopsy | 264 (34.0%) | 601 (26.8%) | <0.001 |
| Number of needle passes | 4.08±1.11 | 3.73±1.09 | <0.001 |
| Number of biopsy segments | 3.33±0.82 | 3.20±0.80 | 0.003 |
| Clinical indication for kidney biopsy | <0.001 | ||
| Hematuria and/or non-nephrotic range proteinuria | 421 (54.3%) | 1507 (67.2%) | |
| Azotemia | 282 (36.3%) | 300 (13.4%) | |
| Nephrotic syndrome | 73 (9.4%) | 435 (19.4%) | |
| Histologic diagnosis | <0.001 | ||
| Glomerulonephritis | 518 (66.8%) | 1307 (58.3%) | |
| Nephrosclerosis | 16 (2.1%) | 34 (1.5%) | |
| Tubulo-interstitial nephritis | 50 (6.4%) | 67 (3.0%) | |
| Lupus nephritis | 47 (6.1%) | 334 (14.9%) | |
| Diabetic nephropathy | 24 (3.1%) | 101 (4.5%) | |
| Vasculitis | 40 (5.2%) | 99 (4.4%) | |
| Amyloidosis | 8 (1.0%) | 33 (1.5%) | |
| Others | 73 (9.4%) | 267 (11.9%) | |
| Department that performed the biopsy | <0.001 | ||
| Nephrology | 675 (87.0%) | 1722 (76.8%) | |
| Rheumatology | 42 (5.4%) | 157 (7.0%) | |
| Allergy | 7 (0.9%) | 140 (6.2%) | |
| Others | 52 (6.7%) | 223 (9.9%) | |
Note: Data are expressed as mean±standard deviation, medians (25th and 75th percentile), or absolute frequencies and percentiles. aPTT, activated partial thromboplastin time; eGFR, estimated glomerular filtration rate; BUN, blood urea nitrogen.
The incidence of clinical indications for kidney biopsy were significantly different between the desmopressin and no-desmopressin groups (p<0.001). Hematuria and/or non-nephrotic range proteinuria (54.3% in the desmopressin group, 67.2% in the no-desmopressin group) were the most common indications. The incidence of azotemia as an indication was higher in the desmopressin group than in the no-desmopressin group (36.3% vs. 13.4%), while the incidence of nephrotic syndrome as an indication was higher in the no-desmopressin group than in the desmopressin group (19.4% vs. 9.4%). The histological diagnosis also differed between the two groups (p<0.001): Glomerulonephritis was the most common (66.8% in the desmopressin group, 58.3% in the no-desmopressin group), while lupus nephritis was more common in the no-desmopressin group (14.9% vs. 6.1%). The departments where the biopsy was performed differed significantly between the two groups (p<0.001); however, the nephrology department was the most common in both groups (87.0% in the desmopressin group, 76.8% in the no-desmopressin group) (Table 2).
Bleeding events within 7 days before PS matchingThe incidence of renal artery embolization did not differ significantly between the two groups (p=0.077); however, blood transfusions occurred significantly more frequently in the desmopressin group than in the no-desmopressin group (p<0.001). The frequency of perinephric hematoma (detected by CT and US) was significantly higher in the desmopressin group than in the no-desmopressin group (p<0.001). In both groups, there was no case in which nephrectomy was performed due to complications from renal biopsy. After biopsy, hemoglobin levels were significantly lower in the desmopressin group than in the no-desmopressin group (p<0.001); moreover, hemoglobin reduction was significantly higher in the desmopressin group (p<0.001). The size of the hematoma was significantly larger in the desmopressin group as compared to in the no-desmopressin group (p=0.016). Post-biopsy SBP (p<0.001) and MAP (p=0.002) were higher in the desmopressin group than in the no-desmopressin group; moreover, the reduction in SBP was significantly greater in the desmopressin group (p=0.007). Hospital stay was significantly longer in the desmopressin group than in the no-desmopressin group (p<0.001) (Table 3).
Bleeding events within 7 days.
| Desmopressin group | No-desmopressin group | OR (95% CI) | p | |
|---|---|---|---|---|
| N=776 (25.7%) | N=2242 (74.3%) | |||
| Bleeding events | ||||
| Renal artery embolization | 4 (0.5%) | 3 (0.1%) | 3.87 (0.86, 17.32) | 0.077 |
| Blood transfusion | 85 (11.0%) | 63(2.8%) | 4.26 (3.04, 5.96) | <0.001 |
| Perinephric hematoma on CT | 34 (4.4%) | 36 (1.6%) | 2.81 (1.74, 4.52) | <0.001 |
| Perinephric hematoma on US | 13 (1.7%) | 4 (0.2%) | 9.53 (3.10, 29.32) | <0.001 |
| Perinephric hematoma (total) | 42 (5.4%) | 39 (1.7%) | 3.23 (2.07, 5.04) | <0.001 |
| Hemoglobin after biopsy (g/dL) | 10.5±2.3 | 12.5±2.3 | <0.001 | |
| Hemoglobin reduction (g/dL) | 0.79±0.99 | 0.17±0.89 | <0.001 | |
| Size of hematoma (mm)a | 32.0±14.0 (N=16) | 18.2±15.9 (N=15) | 0.016 | |
| Post-biopsy blood pressure | ||||
| SBP after biopsy (mmHg) | 120±18 | 116±16 | <0.001 | |
| DBP after biopsy (mmHg) | 74.2±11.3 | 73.4±10.3 | 0.116 | |
| MAP after biopsy (mmHg) | 89.3±12.4 | 87.8±11.4 | 0.002 | |
| SBP reduction (mmHg) | 6.34±16.24 | 4.53±14.54 | 0.007 | |
| Length of hospital stay (day) | 10.5±15.2 | 6.4±11.1 | <0.001 | |
OR, odds ratio; CI, confidence interval; CT, computed tomography; US, ultrasound; SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure.
The age, sex, BMI, SBP, MBP, hemoglobin, platelet count, hematocrit, PT, aPTT, serum creatinine, eGFR, and BUN were chosen as variables that could influence bleeding events. Following PS matching for these variables, there were no differences in the variables between the two groups, as the standardized mean difference (SMD) was less than 0.1 (Table 4).
Propensity score matching for comparison of differences according to whether desmopressin was administered or not.
| Before matching desmopressin | After matching desmopressin | ||||||
|---|---|---|---|---|---|---|---|
| (+) | (−) | p | SMD | (+) | (−) | SMD | |
| Number of patients | 776 | 2242 | 627 | 627 | |||
| Age (years) | 50.2±16.8 | 43.5±16.1 | <0.001 | 0.405 | 49.0±16.7 | 49.2±16.0 | 0.014 |
| Women (%) | 344 (44.3%) | 1155 (51.5%) | 0.001 | 0.144 | 290 (46.3%) | 297 (47.4%) | 0.022 |
| Body mass index (kg/m2) | 23.9±3.6 | 23.8±3.8 | 0.581 | 0.024 | 24.1±3.7 | 23.9±3.9 | 0.044 |
| Systolic blood pressure (mmHg) | 126±19 | 121±17 | <0.001 | 0.286 | 124±19 | 123±18 | 0.095 |
| Mean arterial pressure (mmHg) | 95.1±12.9 | 91.9±11.9 | <0.001 | 0.260 | 94.2±12.8 | 93.2±12.4 | 0.076 |
| Hemoglobin (g/dL) | 11.3±2.6 | 12.6±2.3 | <0.001 | 0.543 | 11.8±2.6 | 11.8±2.5 | 0.009 |
| Platelet (×103/μL) | 243±93 | 256±82 | 0.001 | 0.144 | 247±91 | 247±84 | 0.001 |
| Hematocrit (%) | 33.7±7.4 | 37.7±6.4 | <0.001 | 0.576 | 35.1±7.2 | 35.2±7.0 | 0.006 |
| Prothrombin time (INR) | 1.02±0.11 | 0.98±0.09 | <0.001 | 0.349 | 1.00±0.10 | 1.00±0.09 | 0.003 |
| aPTT (sec) | 29.2±5.8 | 28.6±4.3 | 0.025 | 0.104 | 29.0±6.1 | 28.7±4.7 | 0.040 |
| Serum creatinine (mg/dL) | 2.87±2.68 | 1.24±1.25 | <0.001 | 0.782 | 2.10±1.93 | 2.10±2.06 | 0.002 |
| eGFR (ml/min/1.73m2) | 45.0±34.5 | 73.6±28.2 | <0.001 | 0.907 | 53.0±33.6 | 54.6±31.6 | 0.046 |
| BUN (mg/dL) | 33.5±22.9 | 19.3±13.1 | <0.001 | 0.765 | 28.5±20.2 | 28.4±19.3 | 0.002 |
SMD, standardized mean difference; INR, international normalized ratio; aPTT, activated partial thromboplastin time; eGFR, estimated glomerular filtration rate; BUN, blood urea nitrogen.
Comparison of the two adjusted groups revealed no intergroup differences in the incidence of renal artery embolization (p=0.341), blood transfusion (p=0.579), and total major bleeding events (p=0.442). Furthermore, total bleeding events (including perinephric hematoma on CT/US) did not differ between the two groups (p=0.239) (Table 5).
Outcome comparison after propensity score matching.
| Desmopressin | OR (95% CI) | p | ||
|---|---|---|---|---|
| (+) | (−) | |||
| Number of patients | 627 | 627 | ||
| Renal artery embolization (%) | 3 (0.5%) | 1 (0.2%) | 3.01 (0.31, 29.01) | 0.341 |
| Blood transfusion (%) | 46 (7.3%) | 41 (6.5%) | 1.13 (0.73, 1.75) | 0.579 |
| Total major bleeding (%) | 48 (7.7%) | 41 (6.5%) | 1.19 (0.77, 1.83) | 0.442 |
| Perinephric hematoma on CT/US (%) | 26 (4.1%) | 16 (2.6%) | 1.65 (0.88, 3.11) | 0.120 |
| Total bleeding events (%) | 63 (10.0%) | 51 (8.1%) | 1.26 (0.86, 1.86) | 0.239 |
| Serum sodium reduction (mmol/L) | 3.83±4.33 | 1.91±3.79 | 1.92a (1.45, 2.40) | <0.001 |
| Significant hyponatremia (<125mmol/L) (%) | 34 (6.0%) | 15 (2.7%) | 2.33 (1.25, 4.32) | 0.008 |
OR, odds ratio; CI, confidence interval; CT, computed tomography; US, ultrasound.
The degree of serum sodium reduction was significantly greater in the desmopressin group than in the no-desmopressin group by an average of 1.92 (p<0.001). Furthermore, the incidence of significant hyponatremia of less than 125mmol/L was significantly higher in the desmopressin group than in the no-desmopressin group (p=0.008) (Table 5).
Subgroup analysis on matched data for major bleeding eventsComparison of the two groups based on a creatinine level of 1.8mg/dL revealed that desmopressin did not significantly change the major bleeding risk in both groups (p=0.808 for serum creatinine less than 1.8mg/dL, p=0.482 for more than 1.8mg/dL, and p=0.870 indicating the difference between the two groups) (Table 6).
DiscussionThis is the largest study to investigate the effect of desmopressin on major bleeding risk (requiring renal artery embolization and blood transfusion) following kidney biopsy. To investigate the major bleeding events, of the 3018 patients analyzed, 776 and 2242 were categorized into the desmopressin and no-desmopressin groups, respectively. After adjusting the two groups by PS matching, we concluded that there was no difference in the major bleeding risk after desmopressin administration. Regarding major post-biopsy bleeding, Peters et al.5 reported that multiple logistic regression revealed that prophylaxis using desmopressin prior to native kidney biopsy led to lesser major complications (for example, bleeding, acute hydronephrosis, and septicemia that requires transfusion and/or an invasive intervention; odds ratio [OR]: 0.38). Furthermore, Leclerc et al.8 reported that patients who received desmopressin had a likelihood of symptomatic hematomas similar to those who did not (OR: 0.39) and a need for urgent radiologic studies lower than those who did not (OR: 0.33). Regarding minor post-biopsy bleeding in this study, there was no difference in the incidence of perinephric hematoma on CT or US between the two groups (p=0.120).
The Caring for Australians with Renal Impairment (CARI) guidelines (2018) recommended that as there is a lack of evidence to support the benefit or harm of desmopressin administration prior to renal biopsy, care units should continue their existing practice until a higher level of evidence is available.11 In 2011, Whittier suggested that although desmopressin may play a role in patients at a high risk of bleeding (which deserves a study in itself), administering desmopressin off-label to all patients undergoing percutaneous kidney biopsy is premature and possibly hazardous.1 In this study as well, we observed a greater sodium reduction in the desmopressin group than that observed in the no-desmopressin group. Considering the increased risk of thrombotic events or hyponatremia associated with desmopressin use,11 we do not recommend desmopressin use before kidney biopsy.
Previous studies reported that the serum creatinine, blood pressure, age, gender, hemoglobin, and platelet count were the risk factors of bleeding after kidney biopsy. In a study by Corapi et al.10 that compared and analyzed 34 studies through meta-analysis of bleeding complications of native kidney biopsy, the transfusion rate was significantly higher in women (≥50%) (p=0.03) and when the mean serum creatinine level was ≥2.0mg/dL (p=0.02). Furthermore, although age ≥40 years (p=0.2) and mean SBP ≥130mmHg (p=0.09) were not significant risk factors, they were associated with a tendency for high transfusion requirements. Moreover, Xu et al.12 also reported that a low platelet count significantly increased the risk of severe bleeding after renal biopsy. In our study, compared to the no-desmopressin group, the desmopressin group was older and had a higher blood pressure and serum creatinine level and lower hemoglobin and platelet levels. As a result, blood transfusions were significantly more common in the desmopressin group before PS matching. A striking observation was the higher number of transfusions in the desmopressin group than in the no-desmopressin group (11% vs. 2.8%) with an average hemoglobin reduction of 0.79±0.99g/dL and a mean post-biopsy hemoglobin level of 10.5g/dL.
Therefore, PS matching was performed to reduce selection bias and compare the bleeding events in the two groups. The SMD13,14 was calculated by comparing all variables deemed to affect bleeding, and was found to be less than 0.1 after correction. Because there were some variables with many missing values, we performed multiple imputations and used the average of PSs from all completed data sets. Because there were fewer patients in the desmopressin group, after matching, the two groups were organized based on those who had the potential to receive desmopressin, and reflected the “average treatment effect on the treated patients” rather than the “average treatment effect” (Table 4). On comparing the bleeding events between the two adjusted groups, no intergroup differences were noted in the incidence of both, renal artery embolization and blood transfusion.
The major limitation of this study is its retrospective and observational nature, which may have inherent selection bias. In our hospital, there was no protocol for administering desmopressin; therefore, desmopressin was administered to people at a high risk of bleeding, as judged by the attending physician. Furthermore, the predominant use of small caliber needles in a generalized way (usually 18-gauge) or a large number of punctures (4 passes and 3.7 passes) could be confounders and influence the absence of differences between the desmopressin and no-desmopressin groups.
ConclusionsWe do not recommend desmopressin administration before kidney biopsy.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone.
We would like to thank to our institute's statistics department for helping with statistics. Also, thank you to Editage for English language editing.