The presence of malnutrition in patients with Chronic Kidney Disease (CKD) is high, it can be made worse by SARS-CoV2 infection.
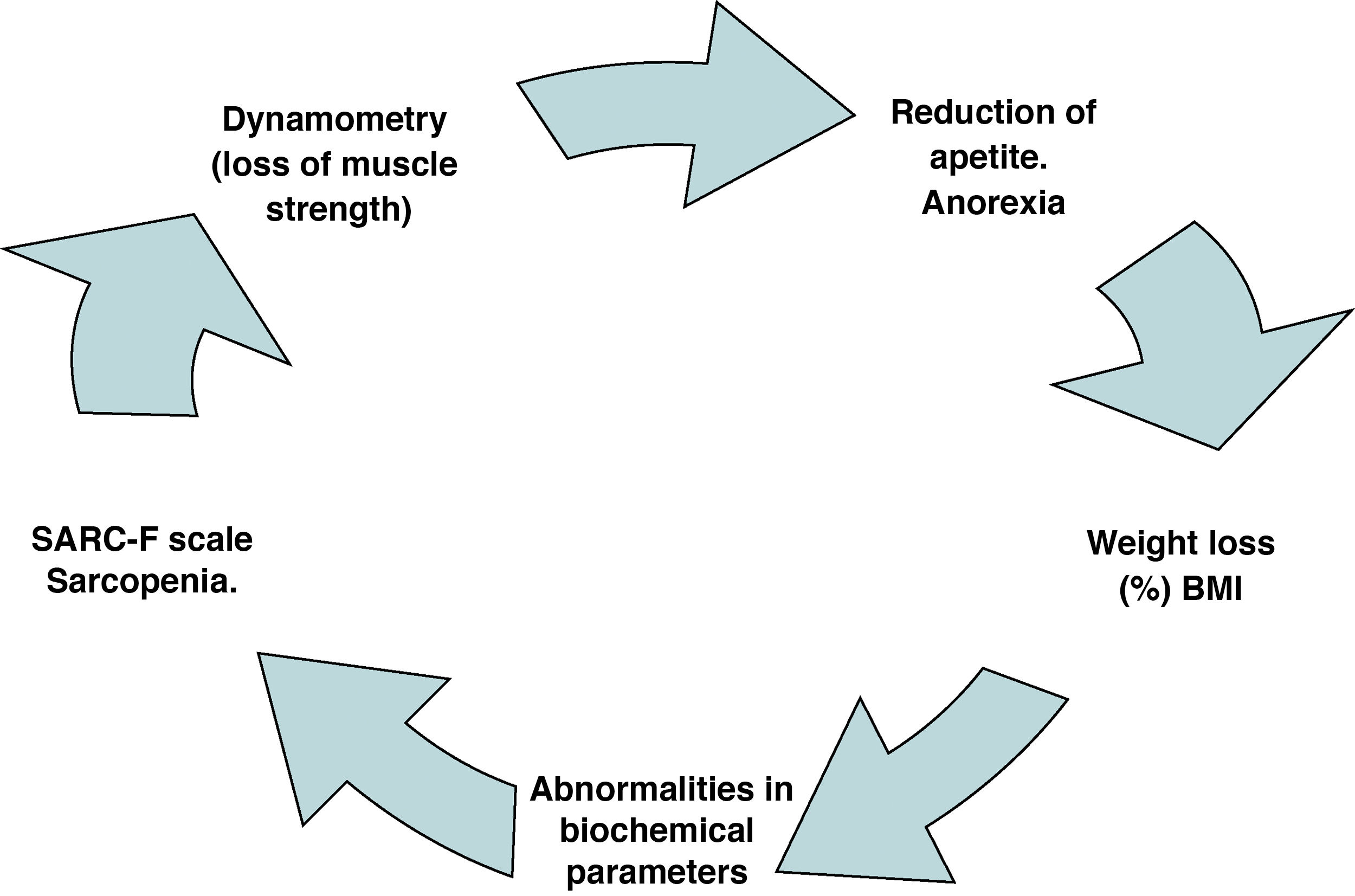
The nutritional assessment should be adapted to minimize the infection, recommending monitoring: weight loss percentage, body mass index (BMI), loss of appetite, analytical parameters and functional capacity using the dynamometer. As well as the sarcopenia assessment using the SCARF scale, and the possibility of using the GLIM criteria in those patients who have been tested positive by MUST.
It is important to adapt the nutritional recommendations in the caloric and protein intake, to the CKD stage and to the SARS-CoV2 infection stage. In patients with hypercatabolism, to prioritize preserving the nutritional status (35 kcal/kg weight/day, proteins up to 1.5 g/kg/day). The rest of the nutrients will be adapted to CKD stage and the analytical values.
In the post-infection stage, a complete nutritional assessment is recommended, including sarcopenia. The energy and protein requirements in this phase will be adapted to the nutritional status, with special attention to the loss of muscle mass.
Dietary recommendations need to be tailored to side effects of SARS-CoV-2 infection: anorexia, dysphagia, dysgeusia, and diarrhea.
Anorexia and hypercatabolism makes it difficult to meet the requirements through diet, therefore the use of oral nutritional supplements is recommended as well as the enteral or parenteral nutrition in severe phases.
La presencia de malnutrición en pacientes con Enfermedad Renal Crónica (ERC) es elevada, puede agravarse por la infección por SARS-CoV2.
La valoración nutricional se debe adaptar para minimizar contagios, recomendando monitorizar: porcentaje de pérdida de peso, índice de masa corporal (IMC), pérdida de apetito, parámetros analíticos y capacidad funcional mediante dinamometría. Así como valorar la sarcopenia mediante la escala SCARF, y la posibilidad de utilizar los criterios GLIM en aquellos pacientes que el cribado MUST ha dado positivo.
Es importante adaptar las recomendaciones nutricionales en ingesta calórica y proteica, al estadio de la ERC y a la fase de infección por SARS-CoV2. En pacientes hipercatabólicos priorizar preservar estado nutricional (35 kcal/kg peso/día, proteínas hasta 1,5 g/kg/día). El resto de nutrientes se adaptarán a estadío de ERC y valores analíticos.
En la etapa post-infección, se recomienda realizar valoración nutricional completa, incluyendo sarcopenia. Los requerimientos energéticos y proteicos en esta fase se adaptarán a la afectación del estado nutricional, con especial atención a la pérdida de masa muscular.
Es necesario adaptar las recomendaciones dietéticas a efectos secundarios de la infección por SARS-CoV-2: anorexia, disfagia, disgeusia, y diarrea.
La anorexia y el hipercatabolismo dificulta el cumplimiento de los requerimiento a través de la alimentación, por lo que se recomienda la utilización de soporte nutricional oral y en las fases severas la nutrición enteral o la parenteral.
The outbreak of the SARS-CoV-2 infection pandemic generates enormous challenges in relation to the health of kidney patients and the organization of health care.
The worse evolution of SARS-CoV-2 infection in elderly patients with comorbidities is due in part to the usual presence of malnutrition and sarcopenia, regardless of body mass index (BMI).1,2 This is intensified in chronic kidney disease (CKD), since the prevalence of deterioration in nutritional status is high, therefore increases the probability that the infected patient is already malnourished.3 Consequently, the integral care of patients with CKD and SARS-CoV-2 infection, should include the diagnosis of malnutrition and the early implementation of nutritional intervention guidelines. This action should be integrated into the global therapeutic strategy aiming of reduce complications of the disease and facilitate the recovery of the patient.
Nutrition protocol in patients with chronic kidney disease and SARS-CoV-2 infectionNutritional assessment of patients with chronic kidney disease and mild/moderate SARS-CoV-2 infectionThe risk of malnutrition in patients with CKD and SARS-CoV-2 infection will be higher than in the general population. This is a consequence of the disease itself and its treatment. Also, it is likely that the patients had previous malnutrition and the frequent association with other diseases.
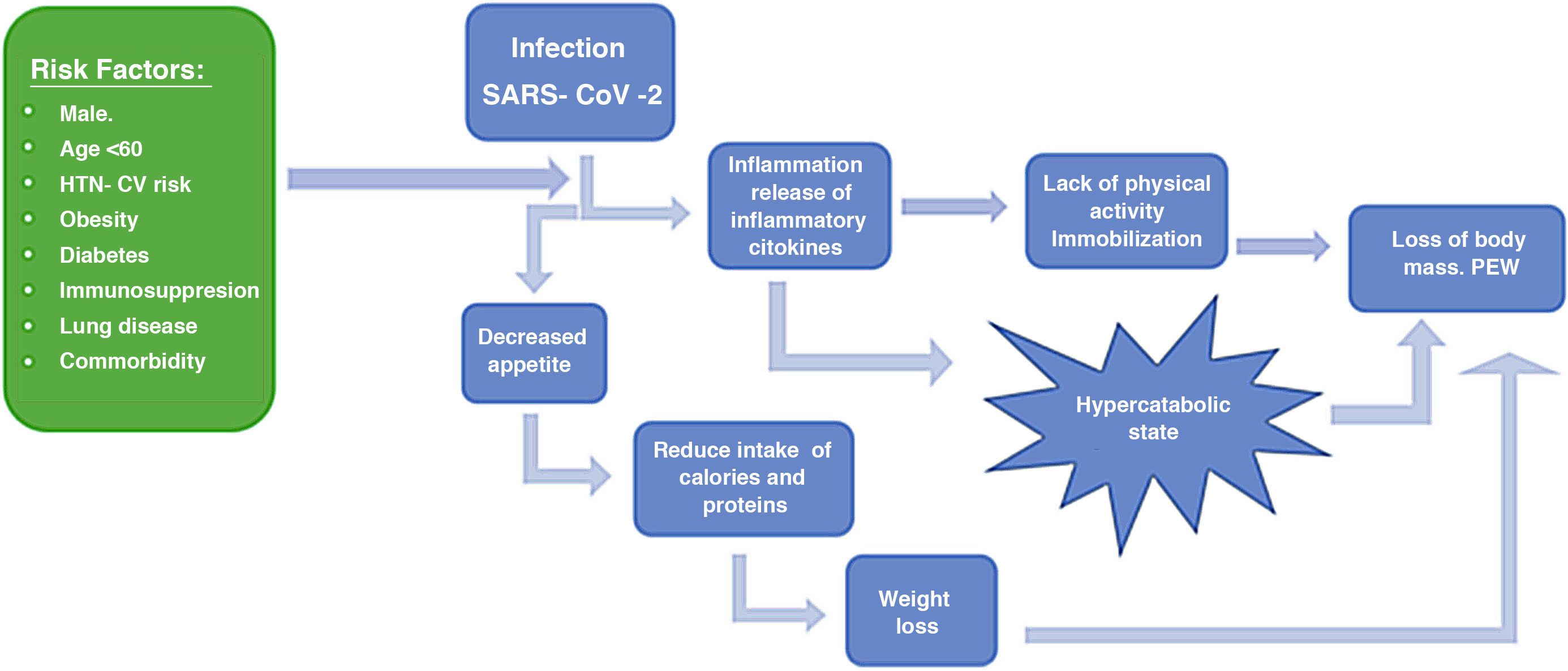
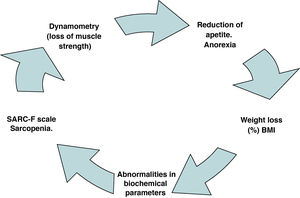
SARS-CoV-2 infection in patients with CKD will develop, even in asymptomatic cases, a subclinical inflammatory alteration, that can affect nutritional status (Fig. 1).
This evidence reinforces the concept that nutritional disorders in these patients should be managed systematically and urgently, also considering that the immune response is weakened by inadequate nutrition.4,5
Nutritional assessment should be the first step in the comprehensive evaluation of the patient with CKD and SARS-CoV-2 infection. Knowing their nutritional status will determine whether there is malnutrition and initiate the treatment early and verify the effectiveness of the treatment.
To avoid contagion, there are 5 aspects used to perform a minimum nutritional assessment: a) percentage of weight loss, b) BMI, c) degree of loss of appetite, d) perform dynamometry and e) s analytical parameter (albumin, prealbumin and CRP). The rest of the tools commonly used to perform a nutritional assessment are very useful, but they require physical contact and disinfection of the material, so their use is limited.
A specific aspect to consider is the loss of appetite and the senses of smell and taste, being more marked in the elderly. It is convenient to assess the presence of dysphagia described in SARS-CoV-2 infection, as well as the diarrhea processes exacerbated by the treatments used. Another point to take into account is dyspnea, which causes fatigue during meals.
The European Nutrition Society (ESPEN)6 recommends the use of nutritional screening such as the Malnutrition Universal Screening Tools (MUST ) method for the early nutritional assessment of patients with SARS-CoV-2 infection; subsequently, if the screening has tested positive, apply the Global Leadership Initiative on Malnutrition (GLIM)7 criteria for nutritional assessment.
To assess sarcopenia, it is recommended the use of the Simple Questionnaire to Rapidly Diagnose Sarcopenia (SARC-F)8 and dynamometry9 is recommended to measure muscle strength (Fig. 2).
Nutritional assessment in critically ill patients with chronic kidney disease and severe SARS-CoV-2 infectionThe American Societies of Critical Medicine (SCCM) and Enteral and Parenteral Nutrition (ASPEN) recommend the use of the NUTRIC score10,11 in critically ill patients.
Once the assessment of the nutritional status has been performed, it is recommended to monitor the nutritional status periodically in any of the phases of SARS-CoV-2 infection by qualified and trained personnel within the framework of an interdisciplinary team (doctor, dietician nutritionist, nursing …). In hospitalized the periodicity of follow-up patients should be weekly.12,13
Nutritional recommendations in patients with chronic kidney disease and SARS-CoV-2 infectionThe main objective of the nutritional recommendations during the process of SARS-CoV-2 infection is to ensure a good nutritional status, and to avoid possible metabolic alterations produced by CKD.14,15
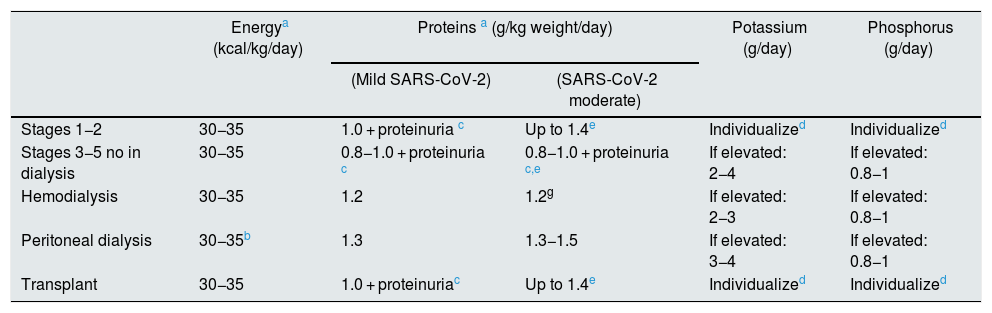
In the case of presenting moderate/severe infection by SARS-CoV-2, it is very likely to detect the appearance of PEW and inflammatory processes, being necessary to prioritize the maintenance of nutritional status; adapting the nutritional recommendations by increasing protein and calories (Table 1).
Table of nutritional requirements according to CKD stage in patients with mild/moderate SARS-CoV-2 infection.
| Energya (kcal/kg/day) | Proteins a (g/kg weight/day) | Potassium (g/day) | Phosphorus (g/day) | ||
|---|---|---|---|---|---|
| (Mild SARS-CoV-2) | (SARS-CoV-2 moderate) | ||||
| Stages 1−2 | 30−35 | 1.0 + proteinuria c | Up to 1.4e | Individualized | Individualized |
| Stages 3−5 no in dialysis | 30−35 | 0.8−1.0 + proteinuria c | 0.8−1.0 + proteinuria c,e | If elevated: 2−4 | If elevated: 0.8−1 |
| Hemodialysis | 30−35 | 1.2 | 1.2g | If elevated: 2−3 | If elevated: 0.8−1 |
| Peritoneal dialysis | 30−35b | 1.3 | 1.3−1.5 | If elevated: 3−4 | If elevated: 0.8−1 |
| Transplant | 30−35 | 1.0 + proteinuriac | Up to 1.4e | Individualized | Individualized |
CKD: chronic kidney disease; TCV: total caloric value.
The nutritional assessment protocol in the post - infection SARS-CoV-2 patient will be the same as that applied during the infection period, but in this case, as there is no risk of contagion, we can apply the all the tools available to us. (bioimpedance, anthropometry, dynamometry …). Therefore, in all cases a nutritional screening will have to be applied, either the MUST or MST and analytical parameters such as albumin, prealbumin and PCR. If the screening is positive, the nutritional assessment will have to be carried out using the GLIM criteria or any validated nutritional assessment method for the kidney patient as a subjective global assessment (SGA) or Malnutrition-Inflammation Score (MIS). It is convenient to complete the assessment with the SARC-F sarcopenia scale and assess the intake (caloric and protein) through the 3-day record or through appetite surveys, in the case of anorexia.
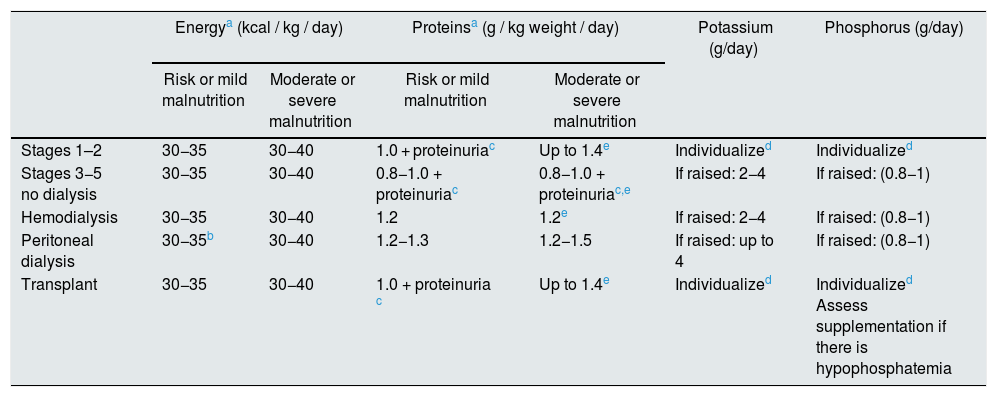
Nutritional recommendations in patients with chronic kidney disease and post - infection by SARS-CoV-2The nutritional recommendations in the post-infection process by SARS-CoV-2 have been developed according to the degree of alteration of the nutritional status: a) risk of malnutrition or mild malnutrition and b) moderate or severe malnutrition (according to the reference assessment method in each center).
Regarding the nutritional recommendations indicated in Table 2, they should only be applied during the period of SARS-CoV-2 disease and in the recovery process. It is recommended to reapply the specific recommendations for patients with CKD once the nutritional status has been recovered.
Nutritional requirements according to the stage of CKD in patients after SARS-CoV-2 infection.
| Energya (kcal / kg / day) | Proteinsa (g / kg weight / day) | Potassium (g/day) | Phosphorus (g/day) | |||
|---|---|---|---|---|---|---|
| Risk or mild malnutrition | Moderate or severe malnutrition | Risk or mild malnutrition | Moderate or severe malnutrition | |||
| Stages 1–2 | 30−35 | 30−40 | 1.0 + proteinuriac | Up to 1.4e | Individualized | Individualized |
| Stages 3−5 no dialysis | 30−35 | 30−40 | 0.8−1.0 + proteinuriac | 0.8−1.0 + proteinuriac,e | If raised: 2−4 | If raised: (0.8−1) |
| Hemodialysis | 30−35 | 30−40 | 1.2 | 1.2e | If raised: 2−4 | If raised: (0.8−1) |
| Peritoneal dialysis | 30−35b | 30−40 | 1.2−1.3 | 1.2−1.5 | If raised: up to 4 | If raised: (0.8−1) |
| Transplant | 30−35 | 30−40 | 1.0 + proteinuria c | Up to 1.4e | Individualized | Individualized Assess supplementation if there is hypophosphatemia |
CKD: chronic kidney disease.
A dietary advice will be given taking into account the clinical severity, the result of the nutritional assessment, the degree of affectation of muscle mass and function, and the nutritional treatment received.18 If necessary will apply nutritional support.
In all degrees of SARS-CoV-2 affectation, it is essential an adequate nutritional support. Protein intake must be maintained and even increased in all clinical situations of the infection, with an adequate caloric and vitamin intake.19
Dietary interventionThe dietary advice will take into account the phase of infection and the CKD stage, following the recommendations in Tables 1 and 2 and considering the following aspects6:
- •
Anorexia, for which it is recommended to divide the intakes and enrich the diet.
- •
Alterations in the senses of taste and smell. Then it is recommended common culinary techniques to flavor foods.
- •
Dysphagia, modify the texture of solids and liquids.
- •
Fatigue, for which easy chewing diets are recommended, even compressed.
- •
If Diarrhea use an astringent diet.
The increase in energy and protein requirements secondary to the hypercatabolic state, associated with the decreased intake due to anorexia, makes it difficult to receive the caloric and protein requirements through food. For this reason, the first measure recommended by the ESPEN guidelines is to enrich the diet with culinary resources.6
In cases where these measures are not sufficient, ESPEN recommends the early use of oral nutritional supplementation that should be maintained until at least one month after the end of symptoms.6
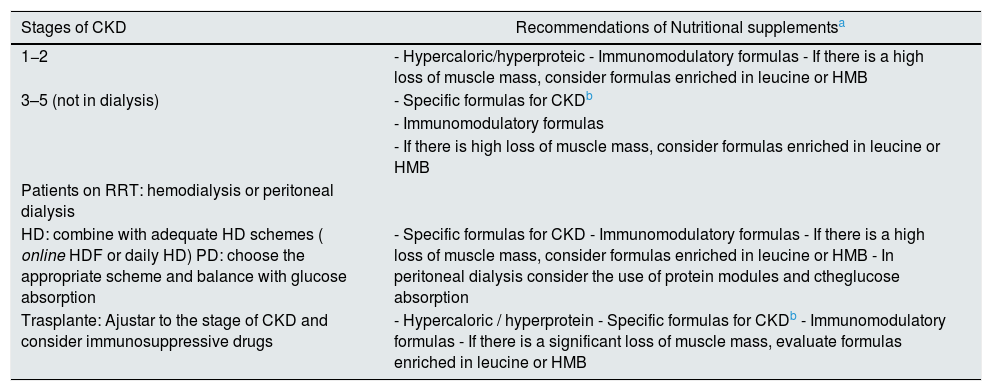
The choice of the nutritional support formula will vary according to the phase of CKD and the severity of the malnutrition. There are several therapeutic options to be chosen by the clinician. The recommended formulas adapted to the CKD phase are described below (Table 3). It is convenient to determine the levels of vitamin D, zinc and selenium and supplement if they are low.20
Recommendations of nutritional supplements in patients with CKD and SARS-CoV-2 infection.
| Stages of CKD | Recommendations of Nutritional supplementsa |
|---|---|
| 1−2 | - Hypercaloric/hyperproteic - Immunomodulatory formulas - If there is a high loss of muscle mass, consider formulas enriched in leucine or HMB |
| 3–5 (not in dialysis) | - Specific formulas for CKDb |
| - Immunomodulatory formulas | |
| - If there is high loss of muscle mass, consider formulas enriched in leucine or HMB | |
| Patients on RRT: hemodialysis or peritoneal dialysis | |
| HD: combine with adequate HD schemes ( online HDF or daily HD) PD: choose the appropriate scheme and balance with glucose absorption | - Specific formulas for CKD - Immunomodulatory formulas - If there is a high loss of muscle mass, consider formulas enriched in leucine or HMB - In peritoneal dialysis consider the use of protein modules and ctheglucose absorption |
| Trasplante: Ajustar to the stage of CKD and consider immunosuppressive drugs | - Hypercaloric / hyperprotein - Specific formulas for CKDb - Immunomodulatory formulas - If there is a significant loss of muscle mass, evaluate formulas enriched in leucine or HMB |
DM: diabetes mellitus; CKD: chronic kidney disease; HMB: hydroxymethylbutyrate.
Note: Evaluate the administration of supplements of vitamins D, Zn and Se.
It is recommended to perform physical activity adapted to the characteristics of the patient as a complement to nutritional treatment.
In the event that oral feeding is not possible, the enteral route is always preferable to parenteral providing that the intestine is functioning.
To administer the necessary amount of nutrients, take into consideration the recommendations of ESPEN6:
- •
In the case of polymorbid patients over 65 years of age it is recommended 27 kca l and 1 g of protein per kg of weight/day.
- •
Malnourished and polymorbid patients it is recommended 30 kcal and 1–1.5 g of protein per kg weight/day.
- •
In ICU patients it is recommend its initiation of it is recommended the initiation of tube feeding when they become hemodynamically stable, with compensated hypoxemia, and always with vigilance for signs of intolerance and intestinal ischemia. It is recommend 15−20 kcal and 1.3 g of protein per kg of weight per day. Administration in these patients should be progressive depending on GI tolerance; it may take more than 3 days to reach 80–100% of the recommended amount. Meanwhile, they will require parenteral nutrition (PN).
It should be noted that in the obese patient, the adjusted weight must be calculated to determine the recommended requirements (adjusted weight = ideal weight + (real weight-ideal weight) × 0.33).
All these values must be individualized according to nutritional status, clinical situation, kidney function, and GI tolerance. In addition, it is recommended to rule out deficiencies of vitamins A, D, B6, B12, C, as well as Zn and Se, since these deficiencies have a deleterious effect on viral infections in general.
The risk of aspiration must always be considered. In intensive care patients and those with significant dyspnea, enteral nutrition (EN) should be initiated at very low doses, with a continuous infusion pump and the use of prokinetics. If possible, administer to the jejunum.6
In intubated and mechanically ventilated patients with SARS-CoV-2 infection, EN can be initiated through a nasogastric tube. In many cases it is required postpyloric administration The prone position is not per se a contraindication in patients with EN, but it makes its administration difficult.
Retrovirals such as lopinavir or ritonavir should be administered in solution and PVC or silicone tubes, avoiding polyurethane tubes because they can harden. In addition, they tend to cause diarrhea, in which case we would recommend the use of peptide formulas and an infusion pump.
Hydrochloroquine and azithromycin can be administered by gavage in tablets dissolved in 10 ml of water.21
It must not be forgotten the risk of sarcopenic dysphagia in patients who have lost a lot of weight or who have not eaten for a while because they have been on EN or PN.
Regarding the EN formulas to be used, the specific formulas available are the same as those used for the oral route as supplementation. In these cases, we should be more cautious in their use because they will be the only nutritional support received by the patient. A control of biochemical parameters is required every one or two days initially to monitor plasma levels of creatinine, urea, calcium, phosphorus and electrolytes. Depending on the residual kidney function of the patient, these specific formulas may be used alone or in combination with non-specific ones if required by the presence of other comorbidities such as diabetes, diarrhea, malabsorption t…
In patients with stress hyperglycemia and dyspnea due to respiratory failure, the provision of formulas rich in monounsaturated fats can fulfill the dual function of controlling postprandial blood glucose and reducing CO2 production. Although we must not forget that in patients with gastroparesis, high gastric residue (> 500 ml) or diarrhea, it would be more advisable to use peptide formulas, with a continuous infusion pump, and if possible in a post- pyloric placement. It should be remembered that the blood glucose levels recommended by the ESPEN Council in all patients is between 6−8 mmol/l (108−140 mg/dl), although the clinically useful range is between 140 and 180 mg / dl, adapted to the age and comorbidity of the patient22.
Parenteral nutritionPN is contemplated as a joint treatment with EN when caloric and protein requirements are not met using the GI tract6.
In patients with CKD, it will be taken into account the administration of fluids and electrolytes, as well as the calcium / phosphorus and potassium balance. Patients with diabetes, respiratory failure and critically ill patients will receive specific nutrition13.
The Metabolism and Nutrition Working Group of the SEMICYUC23,24 and ASPEN25 recommends that in patients with PN consider:
- -
If refeeding syndrome is suspected, start with 25% of the calculated caloric intake, and monitoring phosphate, magnesium and potassium concentration. The first 72 h is the period of highest risk of refeeding syndrome in these patients.
- -
The total dose of caloric and protein should be reached in the first week and take into account the lipid contribution of propofol.
- -
Maintain blood glucose <180 mg / dl with insulin analogues twice a day and regimens with rapid subcutaneous or IV insulin.
- -
Do not administer formulas with high lipid content in the presence of hypertriglyceridemia (TG> 400 mg / dl) that in these patients appears to be related to severe inflammation.
- -
The formulas of PN recommended in the first week, during the inflammatory phase, should limit soy lipid emulsions due to their inflammatory effect. A mixture of monounsaturated, polyunsaturated, and medium chain triglycerides might be adequate. Patients receiving propofol can develop hypertriglyceridemia rapidly, TG monitoring is advised every 24 h25.
- -
Adapt the formulas of total parenteral nutrition (TPN) to the characteristics of the renal patient. In the case of hemodialysis patients, it ca bu used intradialysis PN combined with another modality of nutritional support.
- -
Use readymade 3- chamber TPN.
- -
It is recommended to maintain TPN until reaching the full dose of EN in the first week and if the requirements are not achieved.
The patient with CKD and SARS-CoV-2 infection presents a high risk of malnutrition.
In processes of infection by SARS-CoV-2 in patients with CKD it is recommended nutritional assessment by: percentage of weight loss or BMI, loss of appetite, analytical parameters and dynamometry.
In patients with mild/moderate SARS-CoV-2 infection and CKD, it is recommended to adjust the energy and protein requirements to the stage of the disease and the presence of inflammation.
In patients CKD post SARS-CoV-2 infection, it is recommended a complete nutritional assessment, paying special attention to the decrease in muscle mass and the appearance of sarcopenia.
Nutritional support should begin with the adaptation of dietary recommendations, paying attention to the presence of anorexia, ageusia, anosmia, diarrhea, dysphagia, and dyspnea.
The different guidelines recommend the early use of nutritional supplementation that should be maintained for one month after the infection.
Conflict of interestsMr. Alberto Caverni Muñoz presents an employment relationship with Nutricia laboratories, this does not affect the scientific content of this article.
The rest of the authors declare that they have no potential conflicts of interest related to the contents of the article.
Please cite this article as: Pérez-Torres A, Caverni Muñoz A, Lou Arnal LM, Sanz Paris A, Vidal Peracho C, La Torre Catalá J, et al. Consenso multidisciplinar sobre la valoración y el tratamiento nutricional y dietético en pacientes con enfermedad renal crónica e infección por SARS-CoV-2. Consenso de nutrición en enfermedad renal crónica einfección por SARS-CoV-2. Nefrologia. 2021;41:453–460.
This article is based on the multidisciplinary consensus on nutritional and dietary assessment and treatment in patients with Chronic Kidney Disease and SARS-CoV-2 infection.