Antecedentes: Un importante obstáculo que dificulta el despliegue de soluciones tecnológicas en sanidad es el rechazo que encuentran los sistemas desarrollados por los usuarios que tienen que utilizarlos (ya sean profesionales sanitarios o pacientes), que consideran que no se adaptan a sus necesidades reales. Objetivos: (1) Diseñar una arquitectura tecnológica para la asistencia remota de pacientes nefrológicos aplicando una metodología que prime la implicación de los usuarios (profesionales y pacientes) en todo el diseño y desarrollo; (2) ilustrar cómo las necesidades de los usuarios pueden ser recogidas y respondidas mediante la tecnología, aumentando el nivel de aceptación de los sistemas finales. Métodos: Para obtener las principales necesidades que existen actualmente en Nefrología se implicó a un conjunto de servicios españoles de la especialidad. Se realizó una recogida de necesidades mediante entrevistas semiestructuradas al equipo médico y cuestionarios a profesionales y pacientes. Resultados: Se extrajeron un conjunto de requisitos tanto de profesionales como de pacientes y, paralelamente, el grupo de ingenieros biomédicos identificó requisitos de la asistencia remota de pacientes desde un punto de vista tecnológico. Todos estos requisitos han dado pie al diseño de una arquitectura modular para la asistencia remota de pacientes en diálisis peritoneal y prediálisis. Conclusiones: Este trabajo ilustra cómo es posible implicar a los usuarios en todo el proceso de diseño y desarrollo de un sistema. Fruto de este trabajo es el diseño de una arquitectura modular adaptable para asistencia remota de pacientes nefrológicos respondiendo a las preferencias y necesidades de los usuarios pacientes y profesionales consultados.
Background: A major obstacle that hinders the implementation of technological solutions in healthcare is the rejection of developed systems by users (healthcare professionals and patients), who consider that they do not adapt to their real needs. Objectives: (1) To design technological architecture for the telecare of nephrological patients by applying a methodology that prioritises the involvement of users (professionals and patients) throughout the design and development process; (2) to show how users’ needs can be determined and addressed by means of technology, increasing the acceptance level of the final systems. Methods: In order to determine the main current needs in Nephrology, a group of Spanish Nephrology Services was involved. Needs were recorded through semi-structured interviews with the medical team and questionnaires for professionals and patients. Results: A set of requirements were garnered from professionals and patients. In parallel, the group of biomedical engineers identified requirements for patient telecare from a technological perspective. All of these requirements drove the design of modular architecture for the telecare of peritoneal dialysis and pre-dialysis patients. Conclusions: This work shows how it is possible to involve users in the whole process of design and development of a system. The result of this work is the design of adaptable modular architecture for the telecare of nephrological patients and it addresses the preferences and needs of patient and professional users consulted.
1. INTRODUCTION
The application of information and communications technology (ICT) in the healthcare domain has revolutionised all areas and specialties of care. In Nephrology, the application of ICT may provide care with advanced capabilities, such as the remote monitoring of haemodialysis patients, the monitoring of dialysis sessions for the early detection of problems and the transfer of data and messages from the home to the healthcare organisation or the development of artificial kidneys.1-4 These advances have not yet been implemented in healthcare practice mainly because there are various obstacles that hinder the effective application of ICT. One of them is the rejection of the systems by those who have to use them (whether they be healthcare professionals or patients), who consider that they are not adapted to their real needs.1,5,6
Apart from the advanced capabilities involved in applying ICT, another benefit that is often discussed is the improvement in healthcare process efficiency and the reduction of associated costs.7,8 An example supporting telemedicine for peritoneal dialysis patients is9 that this technique involves saving expenses on medical transport and obtains a positive response from patients. Given the ageing population, the resulting growing demand for healthcare services and the current economic climate, this type of technique that optimises resources and improves the cost-efficiency relationship of healthcare becomes indispensable. This is particularly urgent in Nephrology, given that renal replacement therapy has high costs and is very demanding from an organisational point of view.10,11
As a result, the effective application of ICT in healthcare, although it can be beneficial on various levels (organisational, care, etc.), has many complex requirements from very diverse disciplines (technology, healthcare, resource management, etc.). Some of these are:
- Sustainability must be one of the keys of the developments, prioritising solutions with a high cost-efficiency rate. That is, we must try to apply the most suitable (not the latest) technology with respect to the particular needs of the problem.12,13
- In a setting as fragmented as healthcare, the systems must be integrated and cooperate with each other with the aim of reducing the impact of isolated systems. Interoperability is a necessary requirement for the advancement of healthcare information systems with advanced capabilities.14
- The continuity of care should be promoted through administrative, regional and time barriers. Healthcare practice is increasingly distributed and shared between separate organisations. The continuity of care, closely related to aspects of technical and organisational interoperability, is a key requirement for strengthening the quality of healthcare services.15
- Given the highly sensitive nature of the information managed in this setting (mainly administrative and health data), the protection of systems and confidentiality of communications are indispensable requirements for any application of ICT in healthcare.16
- Lastly, from the clinical point of view, a key aspect in the development of ICT solutions must be the involvement of users in the whole design process and as evaluators of developments. User (whether they be healthcare professionals or patients) contributions are often avoided in the design and development of the systems, resulting in technological applications with major rejections by users because they are not adapted to the daily practice methods or they have limited usability.17
The complexity involved in covering and satisfying such a wide and heterogeneous spectrum of requirements (those previously described are only some examples) is one of the main obstacles for the development of efficient and complete solutions. The application of ICT in healthcare following a methodological approach will be key to coping with this complexity and will also allow the implementation of new healthcare settings, cost reduction and an improvement in healthcare processes.
Taking into account the current situation of the Spanish healthcare system, a project called e-Nefro18 has been developed in which a methodology that applies ICT to healthcare is put into practice and it prioritises the involvement of its users in all the stages of its design and development. The methodology is explained in section 2, as well as the key aspects on which it is based. Section 3 briefly describes the aim of this initiative, it explains the requirements provided by users and experts and it presents an initial approach to the system design. Section 4 summarises the conclusions.
2. METHODOLOGY FOR APPLYING INFORMATION AND COMMUNICATIONS TECHNOLOGIES IN HEALTHCARE
The domain of ICT system design and development methodologies has grown exponentially in the last few decades and there are currently many methodological approaches with different aims (development of software and/or hardware, for example), means of operation (in cascade, iterative, etc.) or key aspects (usability, user experience, sustainability, etc.).19
One of the factors that most affects the success of ICT applications in healthcare is the imperfect understanding between the parties involved in the design, development and use of the systems, particularly whenever the users’ requirements are established. All information systems need to be user-centred in terms of design. This is applied with greater emphasis in the healthcare domain and mainly whenever the systems are directly involved in patient care, since the latter may be users of the system (aside from professional users). Recognising the final users as key participants to be involved in all stages of system design and development may contribute to the latter having greater opportunities of success once it is implemented and in use.
User involvement and the consideration of their needs in the design and development processes are widely recognised aspects, but it is still not very clear how they can be used in practice.20 There are many different work philosophies that try to involve users in the design processes, such as user-centred design,21 participatory design,22 design for all (which strengthens the inclusion of all types of users)23 or human-centred design (which is addressed in regulation ISO 9241-210).24 The benefits of proposals focussed on the user and applied to the healthcare domain include: greater patient safety, better healthcare results and greater user satisfaction.25,26
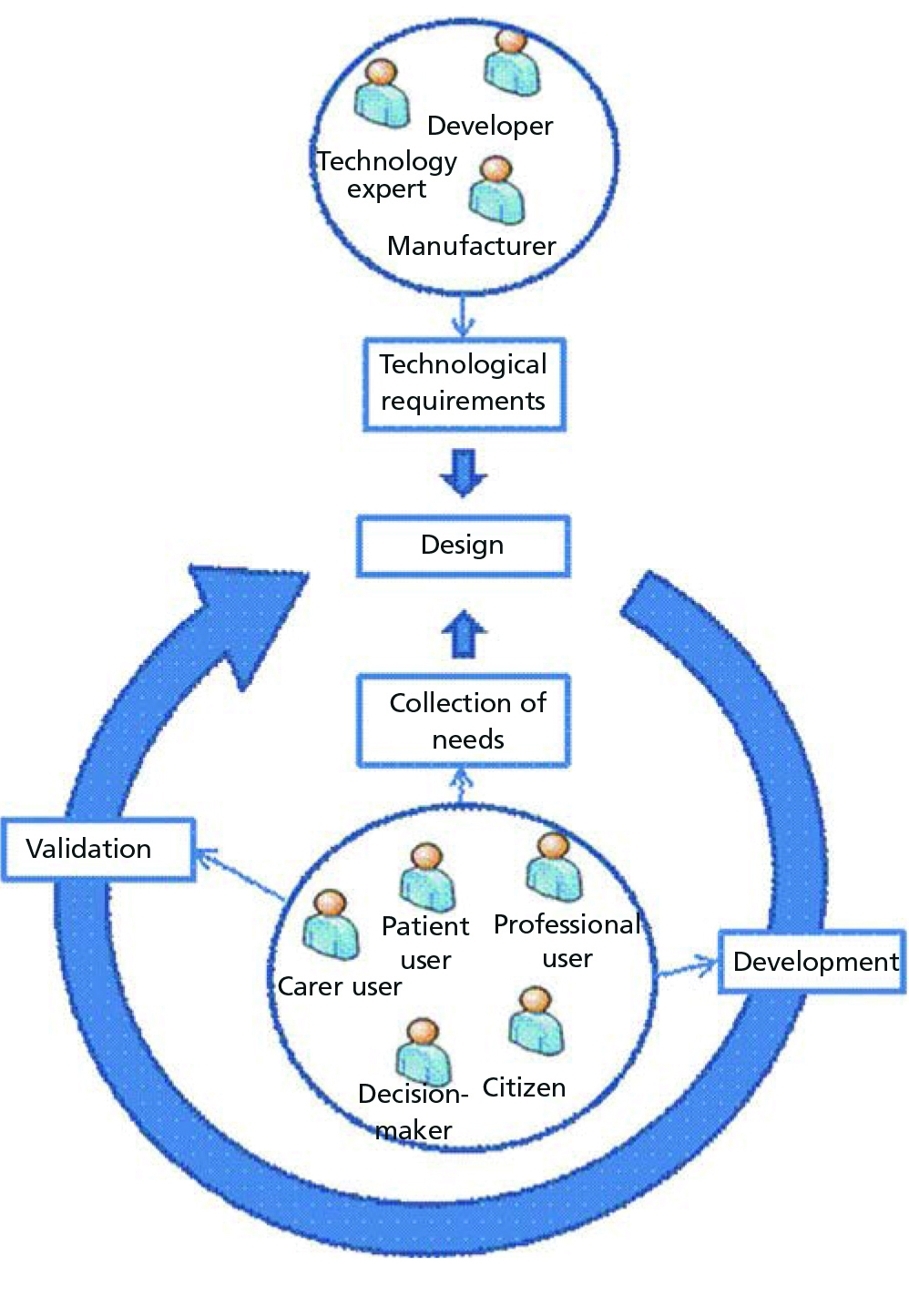
Resulting from the analysis of general purpose methodologies, a method of applying ICT in the healthcare domain has been set out (Figure 1). This methodological approach takes into account design principles considered as good practices in the applicable regulations.24 These are:
As illustrated in Figure 1, our methodological proposal begins with a collection of user requirements (taking into account the wide heterogeneity of potential users) and of the technological requirements defined by the team of developers. An initial design of the system is thereby carried out for the first iteration and it is developed and validated with the users. This cycle continues and functionality is added to the system until the complete solution is achieved.
Below, we describe the application of this methodology to the e-Nefro project, whose objective is the design and development of a telecare system for pre-dialysis and peritoneal dialysis patients.
3. APPLICATION OF THE METHODOLOGY TO AN EXAMPLE CASE: THE E-NEFRO PROJECT
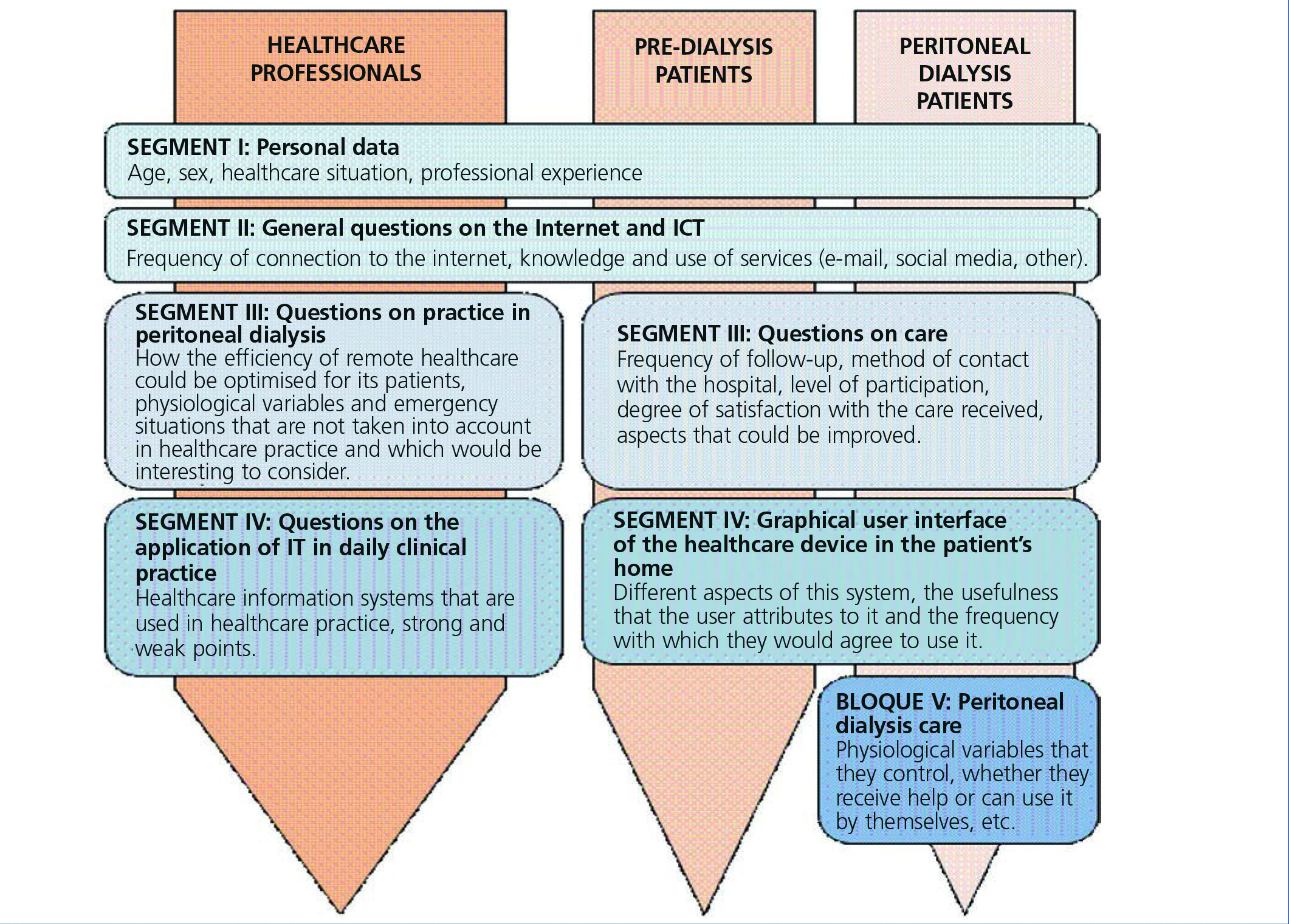
The e-Nefro project (Adaptable modular architecture for the comprehensive telecare of kidney patients)18 is a multicentre effort between the Universidad de Sevilla and various national hospitals, whose objective is to establish architecture that is applicable and adaptable to the telecare of pre-dialysis and peritoneal dialysis patients. It is being carried out using the methodology presented in the previous section, with users having an active role in the design and development of the end solution. With the aim of involving them in the development of the systems to be applied, the first step was to determine the main current needs in a group of Spanish Nephrology services from the experiences and perspective of nephrologists and the patients themselves. This garnering of needs and requirements was carried out in three stages:
Furthermore, the development team, composed mainly of experts in biomedical engineering, established the main technological requirements that the system and its support infrastructure would have to meet. These requirements are displayed in section 3.2.
3.1. Technology-independent aspects: the users’ point of view
The interviews and questionnaires allowed two sets of requirements to be extracted: those from professional users and those identified by the patient users. This section briefly reports the most significant results of this needs collection task.
Firstly, the healthcare professionals interviewed and surveyed thought that, by using technology, the efficiency of their care work could be improved, although they identified various obstacles and weak points that hinder this improvement process. The requirements that they proposed and that could be resolved by technology include:
From the questionnaires to patient users, we have deduced that the design and development of a telecare system for pre-dialysis and peritoneal dialysis patients must take into account:
3.2. Technology-dependent aspects
In parallel to the study of the needs of professionals and patients, the group of biomedical engineers carried out an analysis from the technological point of view of patient telecare. The decentralised setting of healthcare that is determined by the remote monitoring of pre-dialysis and peritoneal dialysis patients in their home imposes a set of technological requirements on the solutions to develop. The most important are listed below:
3.3. Design of technological architecture for the telecare of pre-dialysis and peritoneal dialysis patients
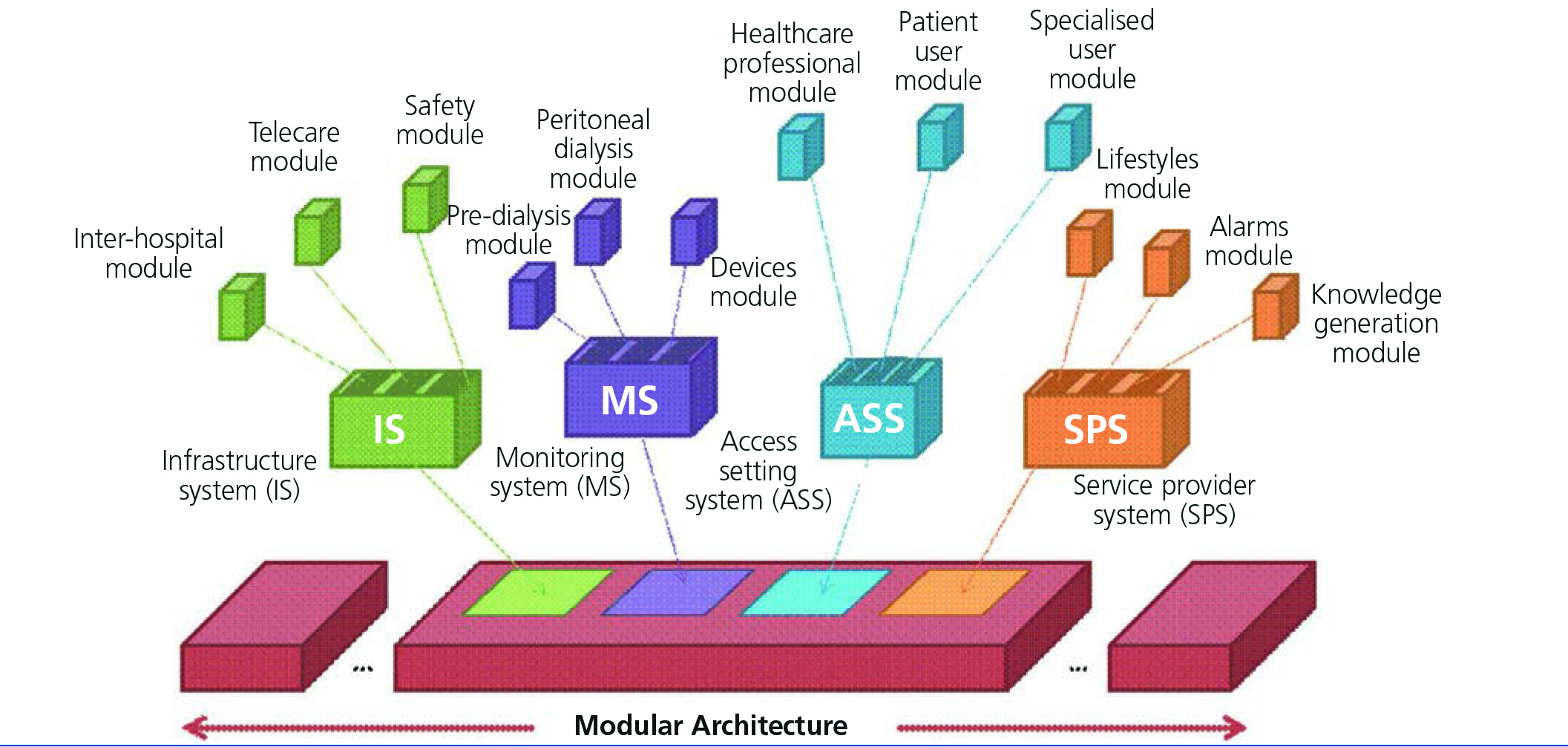
Given the technological and user requirements, the architecture that has to be designed is very complex. The use of middleware, providing elements and capabilities that allow most requirements of the distributed systems to be resolved makes it possible to simplify this complexity. One of the most widespread design paradigms of distributed systems, service-oriented architecture (SOA),27 establishes an architectural model that seeks system agility, efficiency and productivity, as well as services as its key component. The main characteristic of SOA is that it is independent of the underlying implementation technology. Applying this paradigm facilitates the satisfaction of functional requirements related to the operation, distribution and heterogeneity of the systems. The system is configured as services that, by their own definition, are autonomous and physically independent units (requirements of concurrency and asynchrony). Furthermore, use of the publication and discovery of services paradigm on which SOA is based satisfies distribution, scalability and heterogeneity requirements. On this middleware (which will consist of implementing SOA technology such as web services technologies28), services specific to the application domain will be developed, that is home telecare for pre-dialysis and peritoneal dialysis patients.
To build flexible architecture that can be adapted to different settings and that is able to evolve over time, the most appropriate approach would be to follow a modular design in which the architecture is broken down into cooperating and independent systems, each centred on specific functionality with the possibility of replacing or adding modules without the need to modify the whole architecture. Figure 3 displays a diagram of this architecture that comprises an infrastructure of communications (falling primarily under middleware) and a set of systems, each centred on specific aspects of the complete architecture. Each subsystem is in turn composed of modules or services that encompass specific functionalities. An infrastructure system (IS) is defined and includes the basic functionality of communication between the patient’s home and the hospital (telecare module), between hospitals (interhospital module) and of data protection and privacy control (safety module). The IS provides the basic technological components that support the communication of data between systems (sending variable measurements from home to the hospital, transfer of patient histories between hospitals, etc.), as well as different means of communication between individuals (messaging, videoconferences, etc.).
The access setting system (ASS) groups the whole functionality related to the specialised, patient user and healthcare professional interfaces. These modules allow access to architecture services to be personalised according to user preferences, their limitations and their authorised permits. The ASS will cover management and compliance with the preferences that each user has for accessing platform services. Some of these preferences could be: the frequency of receiving new information, the group of alert events that they wish to receive or the interface parameters in line with potential functional limitations for users (font size, use of screen reader software, auditory limitation, etc.).
The aim of the monitoring system (MS) is to provide architecture with the capability of sending, receiving and consulting data between the patient’s home and the healthcare organisations, using the MS mechanisms both for communication and for safety. Furthermore, included in this system are all the specific pre-dialysis and peritoneal dialysis patient healthcare services. The remote configuration of devices and access to data obtained would also be carried out using this system. It would include, on one hand, the devices that automatically collect the user’s physiological variables and send them to the hospital, and on the other, the information systems that allow the patient (and specialised) user, through computers or mobile devices, to be aware of the activities determined by the professionals in their care plan. The professionals could also be aware of the incidents that occur to their patients, exchange messages with them and adapt the care plan of each, allowing continuous monitoring of the therapy, through various devices (mobiles, tablets or computers).
Lastly, the service provider system (SPS) complements the architecture with a set of general purpose services added within the healthcare setting. These services contribute added value to the system and may be provided by one or several providers. In this system, we may find services designed for data processing, alarm management (notifying the relevant users in accordance with the protocol defined for each one) and knowledge generating tools (clinical decision support systems, simulation via mathematical models, etc.)
We see how the modules, although independent and separate, are closely linked to one another. As such, for example, whenever a user accesses the system, they consult the corresponding ASS module to recover how they wish to access the information and how the latter should be presented. The safety module would have to be consulted previously in order that the user may authorise access to the system and indicate what functionality is available for it. In accordance with the service that the user will employ, MS or SPS modules will be used.
Once the system is designed, the next step will consist of an iterative and incremental process of development in which involvement of the final users will be constant, and there will be a guarantee of acceptance once the system is developed. We should state that the aspects of usability of the devices and systems developed are envisaged in subsequent stages of the methodology and they will be addressed in the project when design has begun on the final user interfaces and devices.
4. CONCLUSIONS
One of the main keys for the acceptance of systems by final users (professionals and patients) is using their specific needs as a basis and involving them in the whole design and development process. This methodological requirement has been put into practice in the e-Nefro project, whose objective is to establish architecture that is applicable and adaptable to telecare of pre-dialysis and peritoneal dialysis patients. For the study of needs, we conducted a set of interviews and questionnaires for professionals and patients, whose results have been presented in this study.
We determined various requirements from the results. Patients wish to: automatically monitor and transfer their health conditions between consultations, but without having to participate actively or be in contact with their doctors and mainly in order to notify medical staff about emergency situations and receive information on the treatment of the illness in accordance with their preferences. Healthcare professionals identified the following needs: the ability to access complete and reliable patient user registries, as well as patient user data updated in real time at any time, receive critical events in real time and avoid being inundated with non-critical interventions/alarms and the possibility of accessing useful information (with a flexible visualisation of the latter in accordance with the needs and preferences of each professional user) in order to evaluate patient progression.
These user needs, in combination with technological requirements identified by the developers, have led to the design of modular architecture adaptable to the different existing settings and to the preferences of patient and professional users. Specific telecare services will be developed for pre-dialysis and peritoneal dialysis users, although its flexibility will allow it to be re-used in any other specialty and clinical setting.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Figure 1. Methodology for applying the healthcare information and communications technologies is incremental and user-centred.
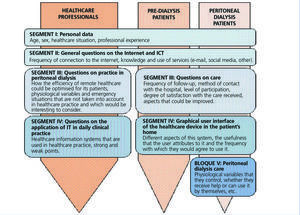
Figure 2. Diagrams of the questionnaires used for healthcare professionals and patients.
Figure 3. Modular architecture for the telecare of pre-dialysis and peritoneal dialysis patients.