To the Editor,
Lactic acidosis in metformin-treated diabetes mellitus patients is a very rare complication, with a high mortality rate and is often associated with an underlying condition, which alone could cause this very severe hydroelectrolytic imbalance. Metformin is a widely-used oral antidiabetic agent, which is eliminated by active tubular secretion, but accumulates in patients with kidney failure.1 Clinically, metformin-associated lactic acidosis (MALA) develops abruptly and is accompanied by overbreathing, abdominal pain, drowsiness and coma. Abnormal laboratory MALA indicators are a high anion gap, base excess in the arterial blood gas and high plasma lactate levels (prognostic value) and metformin plasma levels. Monitoring the lactate and metformin levels is a very useful way of evaluating the evolution and the possible modifications in the treatment. MALA treatment is controversial; using bicarbonate is usual although there is no scientific evidence associating it with a better prognosis. Low metformin binding to plasma proteins allows haemodialysis techniques with bicarbonate solutions to be used when it has been overdosed. This technique has proven to be effective in eliminating plasma metformin and also allows acidosis to be corrected.2,3 Dialysis seems to contribute significantly to treating this severe pathology and improving results where MALA is associated with acute renal failure.4 If we were to compare MALA to severe lactic acidosis located elsewhere, MALA prognosis is significantly better. Its diagnosis should be considered in all metformin-treated patients that present with lactic acidosis.5
Eighty-one year old patient with high blood pressure, dyslipidaemia, type 2 diabetes and dilated myocardiopathy (ejection fraction [EF] 30%). Usual treatment: telmisartan, torsemide, metformin 850mg/8hrs, atorvastatin, carvedilol and omeprazole. She arrived at the emergency department with diarrhoea with mucus and blood, and vomiting, which had lasted for one week, as well as oligoanuria for 24 hours.
Physical examination: blood pressure: 120/70mm Hg, heart rate (HR): 95bpm, temperature (T): 36ºC.
Neurological examination: Glasgow score 12, time/space disorientation and bradypsychia, with no signs of focusing. Rhythmic heart beat, no murmur, crackling until the middle field. No signs in the abdomen and lower limbs.
Biochemical tests showed: haemoglobin: 11.7g/dl; leukocytes: 18 030 (78.9% neutrophils); platelets: 307 000; glucose: 68mg/dl; urea: 133mg/dl; creatinine: 6.89mg/dl; sodium: 134mEq/l; potassium: 4.4mEq/l; pH: 6.89; pCO2: 29mm Hg; bicarbonate: 6.9mmol/l; ionic calcium: 3.85mg/dl; anion gap: 28. Normal coagulation. Urine: pH: 6; creatinine: 71mg/dl; proteinuria: 400mg/dl; 100 red blood cells/field; 60 leukocytes/field; positive ketone bodies and negative drugs (benzodiazepines, barbiturates). Normal abdominal ultrasound with symmetrical kidneys (12cm); good corticomedullary delimitation.
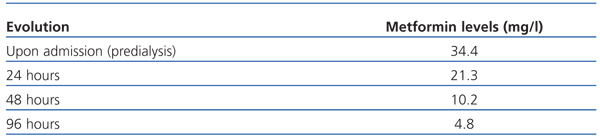
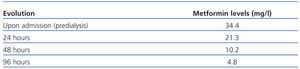
Electrocardiogram: left bundle branch block (LBBB) at 93bpm. Chest X-ray: cardiomegaly and normal cranial computerised tomography (CT). She was diagnosed with stage 2 chronic kidney failure secondary to acute prerenal hypertensive and diabetic nephropathy in a tubular necrosis phase and high anion gap lactic metabolic acidosis. Repletion treatment with physiological saline solution (PSS) at 0.9%, and dextrose solution at 5%, loop diuretics and 1M sodium bicarbonate. Despite this treatment, she continued with anuria and her cognitive function continued to deteriorate. We therefore decided to perform her first 2-hour haemodialysis session without ultrafiltration. Having confirmed hyperlactacidaemia (10.7mmol/l), high metformin levels (34.4mg/l; therapeutic levels 1.3-5) and symptoms of heart overload with haemodynamic disorder, we decided to perform dialysis for four days and then every 48 hours until reaching a constant lactate decrease and non-toxic levels of metformin (Table 1). She received 7 sessions in total. She received empirical antibiotic therapy with third-generation cephalosporin; the urine and faecal cultures were negative.
She was discharged without any neurological and renal symptoms, with creatinine at 1.6mg/dl and the following treatment: carvedilol at a dosage of 6.25mg/24hrs, repaglinide at a dosage of 1.5mg/8hrs, telmisartan, atorvastatin, torsemide at a dosage of 10mg/24hrs and omeprazole at 20mg/24hours.
She currently presents with 1.26mg/dl creatinine and is neurologically stable.
Table 1. Evolution of metformin levels