To the Editor:
The association between membranous nephropathy and solid organ tumours is well known. In the case of Hodgkin’s lymphoma (HL), the most common histological type of renal involvement is minimal change glomerulonephritis followed by focal segmental glomerulosclerosis.1 We report the case of a patient with membranous glomerulonephritis (MG) who had been diagnosed five years earlier with HL and was in complete remission.
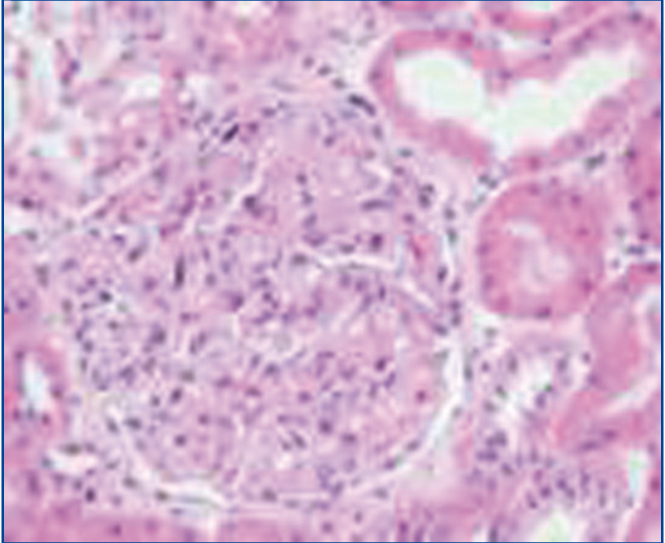
Our patient is a 50-year-old male with no relevant medical history, who was diagnosed, by biopsy of retroperitoneal adenopathy, with stage IV lymphocyte predominance HL with bone marrow involvement in October 2005. He was treated with polychemotherapy, eight ABVD cycles with increased partial response and consolidation radiotherapy on the retroperitoneal mass. In October 2006, a complete response was observed by positron emission tomography (PET) and computerised tomography (CT). The patient remained asymptomatic until March 2010, when he developed complete clinical and biochemical nephrotic syndrome with proteinuria of 12g/day and normal renal function. His immunological profile was negative (antinuclear antibodies [ANA] , anti-DNA, c and p anti-neutrophil cytoplasmic antibodies [ANCA], anti-GBM Ab, C3-C4, hepatotropic virus and human immunodeficiency virus serologies negative, cryoglobulins negative, immunoglobulins, blood and urine electrophoresis). Renal biopsy showed 13 glomeruli with slight mesangial matrix expansion, without interstitial or vascular abnormalities, with immunofluorescence positive for IgG with a granular pattern and weakly positive for C3; the electron microscope study displayed subepithelial electron dense deposits, consistent with stage 1 MG. Given this diagnosis, secondary causes of MG and HL recurrence were ruled out by additional studies (CT of the chest, abdomen and pelvis, PET-CT and bone marrow biopsy). After treatment with oral chlorambucil and steroids for 18 weeks, there was partial remission (proteinuria 3.5g/day in November 2010). During the following three months, the patient was treated with tacrolimus (4mg/day) and low-dose prednisone, with complete remission being achieved in February 2011, which was maintained after discontinuation of immunosuppressive therapy. The nephrotic syndrome currently remains in complete remission with normal renal function and no evidence of recurrence of HL 22 months later.
On reviewing the literature, we found more than 150 cases of HL associated glomerulonephritis, while only 5% of these were MG.2 In most patients, MG manifests simultaneously with HL or its recurrence, but it may do so even a year before the latter is detectable.3 In the present case, HL was inactive at the time of diagnosis, despite which we assumed the existence of an aetiopathogenic relationship between the nephrotic syndrome MG and HL. Cervera et al. and Gomez-Campderá et al. described similar cases in which MG appeared 30 to 18 months after HL was in complete remission without evidence of recurrence.4
The HL-MG association aetiopathogenesis is not well defined, and abnormalities in T lymphocytes function and the overexpression of proto-oncogenes in HL appear to play an important role in the formation of immune complexes. These abnormalities in the immune system last for a long time despite HL being cured,1,5 which may predispose these patients to diseases mediated by T lymphocytes abnormalities.
MG treatment, when associated with active or recurrent HL, is based on combination chemotherapy of the underlying disease (ABVD or ABVD combined with COPP), with a high cure rate in both processes, as stated by Lien et al. in their review of paraneoplastic glomerulopathies.1 Since our case involved HL that was in complete remission, the patient was treated with conventional therapy used in primary MG, with a good response and complete remission of symptoms.
In summary, MG is not only associated with solid organ tumours, but also with haematological diseases, although it is not the most common form of renal involvement. The immunity of patients who have suffered HL continues to be abnormal for some time after its cure. In all patients with a history of HL and nephrotic syndrome, we should rule out HL recurrence. This situation will determine the treatment and progression of the renal pathology.
Acknowledgements
We express our gratitude to Prof. J. Forteza (Head of the Department of Anatomical Pathology at the Hospital Clínico Universitario de Santiago de Compostela) for the electron microscope study.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Figure 1. Glomerulus with mesangial matrix expansion.