Uraemic pruritus (UP) is one of the symptoms with more effects on the quality of life of the haemodialysis (HD) population. Despite its high prevalence (30–70%), it is not treated adequately.1 Diphelikephaline (DFK) is a peripheral kappa-opioid receptor agonist recently approved for the treatment of UP.2 However, experience of DFK in patients on incremental haemodialysis (iHD) is limited.
We present the case of a 62-year-old woman with a right nephrectomy due to severe hydronephrosis secondary to lithiasis, arterial hypertension and type 2 diabetes mellitus. HD was started due to poor blood pressure control, hyperkalaemia, uraemic symptoms and generalised pruritus, with one weekly session of 240 min and asymmetric cellulose triacetate dialyser-1.9 m2 (ATA®). At the beginning of iHD, there was a clearance of creatinine (ClCr) and urea (KrU) measured by 24-h urine and residual diuresis of 16; 4.70 ml/min/1.73 m2 and 1900 ml respectively.
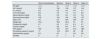
Due to the persistence of pruritus, dermatological, haematological, hepatic/biliary, neurological, psychiatric and pharmacological causes were ruled out. The patient maintained standard Kt/V adjusted to body surface area greater than 2.3 weekly volumes, high convective volume and residual diuresis with KrU > 4 ml/min. Therefore, it was considered justified not to increase the dialysis dose (Table 1). Initial treatment with moisturisers, dermal emollients, gabapentin and mirtazapine were unsuccessful. The severity of pruritus and the impact on quality of life were evaluated using the WIN-RS and SADS3 questionnaires, presenting 8 points and a moderate degree, respectively. Given the persistence of symptoms, IV DFK was requested (0.5 µg/kg/pos-HD weekly) through the Early Access Program. After 12 weeks of treatment, pruritus was reduced to 4 points and a mild degree on the WIN-RS and SADS scales, respectively (Table 1). The patient did not have adverse effects with this drug during follow-up.
Analytical evolutionary control, haemodialysis parameters and pruritus assessment scales.
| Start of haemodialysis | Baseline | Week 4 | Week 8 | Week 12 | |
|---|---|---|---|---|---|
| Hb (g/dl) | 11.5 | 12 | 11.5 | 11.2 | 11.3 |
| Na+ (mmol/l) | 139 | 139 | 136 | 137 | 140 |
| K+ (mmol/l) | 5.9 | 5.2 | 4.9 | 4.8 | 4.7 |
| Uric acid (mg/dl) | 8.8 | 7.8 | 7.4 | 7.2 | 6.8 |
| Serum albumin (mg/dl) | 2.8 | 3.2 | 3.2 | 3.3 | 3.3 |
| Serum glucose (mg/dl) | 148 | 154 | 154 | 150 | 157 |
| HbA1c (%) | 6.5 | 6.2 | N/A | N/A | 6.0 |
| Weight (kg) | 70.5 | 69.5 | 68.4 | 67 | 67 |
| Phosphorus (mg/dl) | 5.7 | 4.9 | 4.5 | 4.5 | 4.7 |
| Calcium (mg/dl) | 9 | 8.9 | 8.9 | 8.7 | 8.8 |
| PTH (pg/ml) | 189 | 180 | 210 | 212 | 288 |
| 25-Hydroxy-vitamin D (ng/ml) | 17 | 14.5 | 20.5 | 26 | 28 |
| Direct bilirubin (mg/dl) | 0.8 | 0.9 | 1 | 0.9 | 0.8 |
| WI-NRS | 8 | 8 | 7 | 6 | 4 |
| SADS | Moderate | Moderate | Moderate | Mild | Mild |
|---|---|---|---|---|---|
| Serum creatinine (mg/dl) | 4.5 | 4.35 | 4.21 | 4.06 | 4.5 |
| Serum urea (mg/dl) | 121 | 128 | 123 | 129 | 126 |
| CKD-EPI (ml/min) | 10 | 11 | 11 | 12 | 10 |
| Residual diuresis (ml/24 h) | 1900 | 1800 | 2200 | 2500 | 2200 |
| KrU (ml/min) | 4.7 | 6.2 | 6.3 | 6.5 | 6.3 |
| ClCr (ml/min/1.73 m2) | 16 | 16 | 17 | 20 | 19 |
| IFG (ml/min/1.73 m2) | 10.3 | 10.3 | 10.75 | 12.75 | 11.75 |
| Bicarbonate (mmol/l) | 15 | 18.8 | 20.3 | 24.3 | 20 |
| ACR (mg/g) | 3300 | 3300 | 3100 | 2800 | 2300 |
| VB (l) | N/A | 80 | 82 | 85 | 86 |
| Vinf-OL-HDF (l) | N/A | 24 | 26.4 | 26 | 25.3 |
| Kt/v (L) | N/A | 1.45 | 1.55 | 1.55 | 1.55 |
| BSA-normalised std Kt/V (l) | N/A | 5.24% | 5.49 | 5,87 | 5,48. |
| EKRU Casino (ml/min) | N/A | 18.1 | 18.6 | 19.4 | 18 |
| KT (l) | N/A | 53 | 56.7 | 54 | 56 |
| IDWG (kg) | N/A | 1 | 1.2 | 0.9 | 0.8 |
ACR: albumin/creatinine ratio; CKD-EPI: Chronic Kidney Disease Epidemiology Collaboration; CrCl: 24-h urinary Cr clearance; IDWG: interdialytic weight gain; Hb: haemoglobin; Hb1Ac: glycated haemoglobin; HD: haemodialysis; GFR: glomerular filtration rate; K +: plasma potassium; KrU: residual renal urea clearance; KT: efficacy of dialysis treatment; N/A: not assigned; na +: plasma sodium; PTH: paratohomorna; SADS: Patient Assessed Severity of Illness Scale; BSA-normalised std Kt/V: standard Kt/V normalised to body surface area; Vinf-OL-HDF: infusion volume in online hemodiafiltration; VB: dialysed blood volume; WI-NRS: worst itch numeric rating scale.
The management of UP continues to be complex due to its multifactorial origin. After ruling out secondary causes, different topical and systemic pharmacological treatments were proposed, with gabapentin being the only drug with a proven effect on UP.1 Furthermore, it has been classically associated with low-flow dialysis and blood levels. Kt/V < 1.5 l.4 There was a hypothesis that those patients who maintained residual renal function on peritoneal dialysis were associated with a lower incidence of UP due to the elimination of larger molecules,5 but recent studies have not found such a relationship.6 In addition, within HD techniques, high-flow HD, online haemodiafiltration and adsorptive HD are associated with improvement in PU symptoms,7 as these techniques are considered to improve the purification of uraemic toxins and the inflammatory state. However, to date, none of these dialysis treatments have been shown to be effective in preventing UP. Only kidney transplantation significantly improves the symptoms of UP.7
In a recent clinical trial, 378 HD patients with moderate-severe pruritus were randomised 1:1 to receive DFK and placebo, 3 times a week post-HD, for 12 weeks. DFK demonstrated rapid efficacy with a significant reduction in pruritus by at least 3 points on the WIN-RS itch scale compared to placebo (51.9% vs. 30.9%), providing an improvement in quality of life.8 However, studies conducted in the HD population only include patients with the conventional 3-day-a-week regimen, without including iHD patients.
For the first time, our case describes the efficacy and safety of DFK in the management of pruritus in a patient on iHD with one session per week. In our centre, in incident patients, the frequency of HD doses is adjusted based on KrU, following the criteria collected in the DIPPI9 study and the recommendations of the National Kidney Foundation-Kidney Disease Outcomes Quality Initiative (NKF-KDOQI) of 2015.10 During follow-up, our patient maintained unchanged diuresis, CrCl and KrU, with correct HD efficacy values, without the need to increase the frequency of the dialysis dose. The new document from the Spanish Society of Nephrology (SEN) on the management of pruritus in HD11 recommends the prescription of DKF for refractory cases.
According to our experience, in patients with adequate renal and dialytic clearance who present refractory pruritus, the use of DFK is useful and safe, and avoids increasing the dialysis dose. This allows us to preserve the quality of life of patients and reduce the cost associated with a greater number of weekly sessions.12
Ethical responsibilitiesThe study complied with the principles set out in the Declaration of Helsinki. The authors declare they received the informed consent of the subject studied, and respect the patient's right to privacy. No experiments were performed on humans or animals for this study.
Conflicts of interestThe author has no conflicts of interest or financial support to declare.