Introduction: Malignant hypertension (MHT) is an uncommon clinical manifestation of IgA Nephropathy (IgAN). Its prevalence, pathogenesis and evolution are not well known. Material and methods: We performed a descriptive and retrospective study to report the clinical characteristics and evolution of thirteen patients diagnosed as having IgA nephropathy by renal biopsy in our hospital who developed MHT (IgAN-MHT). Results: The prevalence of MHT in our IgAN patients was 7% (13/186). The mean age was 37±12 years and 84% were males. Mean systolic/diastolic blood pressure at presentation were 219±32/132±18mmHg, respectively. Renal function impairment was detected at admission in all the patients, with a mean serum creatinine of 4.73±3.12mg/dL. No patient showed analytical data that suggested thrombotic microangiopathy. Renal biopsies showed mild chronicity lesions and only four patients presented features of thrombotic microangiopathy. All patients were treated with renin-angiotensin-aldosterone blockers and two received steroids. They all showed a progressive loss of renal function. At the end of follow up one patient had died, ten were on chronic dialysis and two presented chronic kidney disease stage 3b. Renal survival was 69% and 35% at 3 and 6 years, respectively. Six patients received a kidney transplant: IgAN relapsed in four patients. One of them presented a new episode of MHT associated with a HELLP syndrome. Conclusions: Malignant hypertension is a form of IgAN clinical presentation having a remarkably worse renal outcome and without specific effective treatment.
Introducción: La hipertensión arterial maligna (HTAM) es una manifestación clínica poco frecuente de la nefropatía IgA (NIgA). Su prevalencia, patogenia y evolución son escasamente conocidas. Material y métodos: Estudio retrospectivo que muestra las características al diagnóstico y la evolución de 13 enfermos con NIgA demostrada por biopsia e HTAM (NIgA-HTAM) diagnosticados en nuestro centro. Resultados: La prevalencia de HTAM en nuestros pacientes con NIgA fue del 7 % (13/186). La edad media de los enfermos fue de 37 ± 12 años. El 84 % eran varones. La presión arterial media al debut del cuadro fue de 219 ± 32/132 ± 18 mmHg. Todos presentaban insuficiencia renal, con una creatinina sérica (Crs) media de 4,73 ± 3,12 mg/dl. Ningún enfermo presentaba datos clínicos de anemia hemolítica microangiopática. El daño histológico fue moderado, existiendo datos de microangiopatía trombótica en cuatro pacientes. Todos los enfermos se trataron con bloqueantes del sistema renina-angiotensina y dos recibieron esteroides. Pese a ello, la función renal se deterioró progresivamente en todos los casos. Al final del seguimiento un enfermo había muerto, diez estaban en diálisis y los dos restantes presentaban una insuficiencia renal crónica estadio 3b. La probabilidad de supervivencia renal fue del 69 % y del 35 % a los 3 y 6 años de seguimiento. Seis enfermos recibieron un trasplante renal: la NIgA recidivó en cuatro de ellos y uno presentó un nuevo episodio de HTAM asociado a síndrome HELLP. Conclusiones: La HTAM es una forma de presentación de la NIgA con un pronóstico renal muy desfavorable y para la que no disponemos de tratamientos eficaces en la actualidad.
INTRODUCTION
IgA nephropathy (IgAN) is the most common primary glomerulopathy, with haematuria (macro- or microscopic) and proteinuria being its most frequent clinical manifestations1. However, there may be other less common (atypical) expressions of this disease. One of these is malignant hypertension (MHT)2. The association between IgAN and MHT (IgAN-MHT) was reported for the first time in 1973 and since then many cases have been published as single cases or in series, with a total of 179 patients reported4-16. The pathogenesis of this complication is unknown and there is very little information available on its long-term prognosis and the efficacy of potential therapeutic measures. In this study we have reviewed all the patients diagnosed with IgAN in our hospital, identifying those who had MHT. Their clinical characteristics, pathological findings, treatment received, clinical course and post-kidney transplantation evolution were recorded and analysed for this study. We also conducted a bibliographical review on the IgAN-MHT association.
MATERIAL AND METHOD
Patients
We reviewed all patients diagnosed with (primary and secondary) IgAN in our hospital between 1975 and 2013, including in the study those who had MHT at any time during the course of the disease.
Definitions
The diagnosis of IgAN was based on the finding in a renal biopsy of predominant mesangial deposits of IgA using immunofluorescence techniques. Hypertension (HT) was defined as blood pressure (BP) greater than 140/85. MHT was diagnosed in patients who had systolic/diastolic BP greater than 180/120mmHg and who had a grade III or III/IV (Keith-Wagener-Barker classification) hypertensive retinopathy in the fundus. The fundus study was initially performed by a nephrologist and was later confirmed by an ophthalmologist.
The follow-up period was defined as the interval established between the renal biopsy and the last visit to the clinic, the loss to follow-up or the development of end-stage renal failure (ESRF). ESRF was defined as having an estimated glomerular filtration rate (eGFR) of less than 15ml/min/1.73m2 or requiring a kidney transplantation or chronic dialysis. The eGFR was calculated using the Modification of Diet in Renal Disease (MDRD-4) equation.
Data collection
We reviewed the medical histories of the patients selected and we recorded the following parameters (both in the baseline period and during follow-up): BP, serum creatinine (SCr), eGFR, proteinuria and urinary sediment, as well as the renal graft evolution in patients that underwent transplantion after reaching ESRF. All of the treatments received by patients during the follow-up were recorded.
For this study the renal biopsies of the patients included were reviewed. The oldest samples had deteriorated and fresh paraffin sections had to be cut and stained for a correct evaluation. The following histological characteristics were recorded: number of sclerosed glomeruli (global or segmental); grade of mesangial proliferation, tubular atrophy and interstitial fibrosis; thrombotic microangiopathy data (hyaline thrombi in the microcirculation; endothelial abnormality with swelling and a decrease in the capillary lumen). The grade of mesangial, tubular and interstitial involvement and the presence of nephroangiosclerosis were graded between 0 and +++ (absent, mild, moderate and severe). The histological findings were also recorded and expressed using the Oxford classification.
Statistical analysis
Quantitative variables that were normally distributed were expressed as a mean ± standard deviation, while those that were not normally distributed were expressed as a median (range). Categorical variables were expressed as percentages. Renal survival was defined as the time elapsed between diagnosis and admission to dialysis or transplantation. The survival analysis was performed using the Kaplan-Meier method. A P value of less than .05 (p<.005) was considered to be statistically significant. We performed the statistical analysis with the SPSS version 17 software for Windows.
RESULTS
Patients
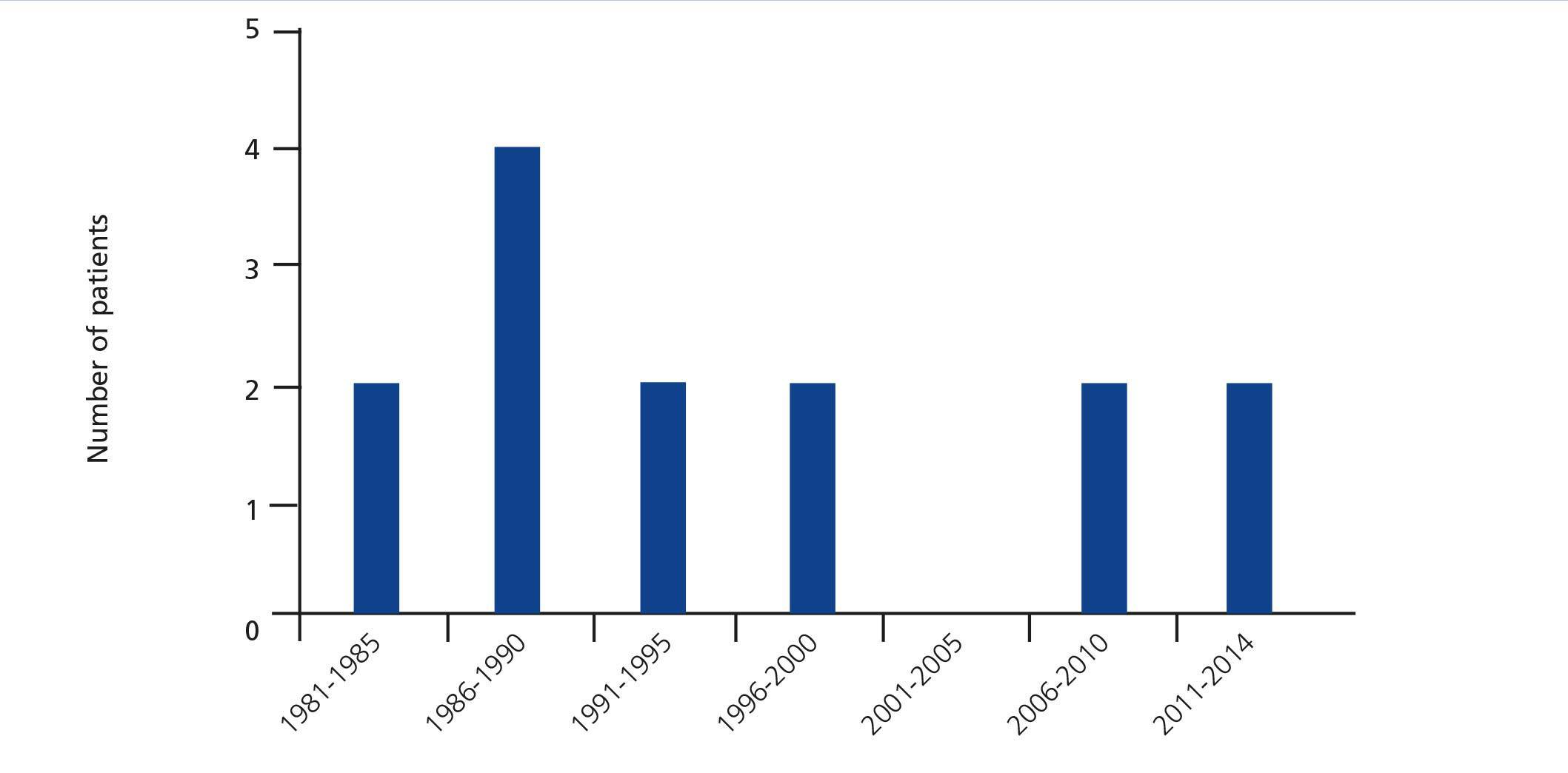
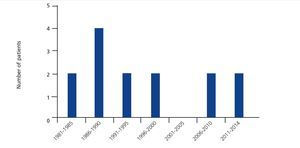
Of the total 186 patients diagnosed with IgAN in the 1975-2013 period we identified 13 with MHT. This represents 7% of the total patients with IgAN. Figure 1 displays the temporal distribution (year of diagnosis) of the 13. Seven of them were diagnosed in the decade between 1984 and 1994, and the other six were subsequently diagnosed.
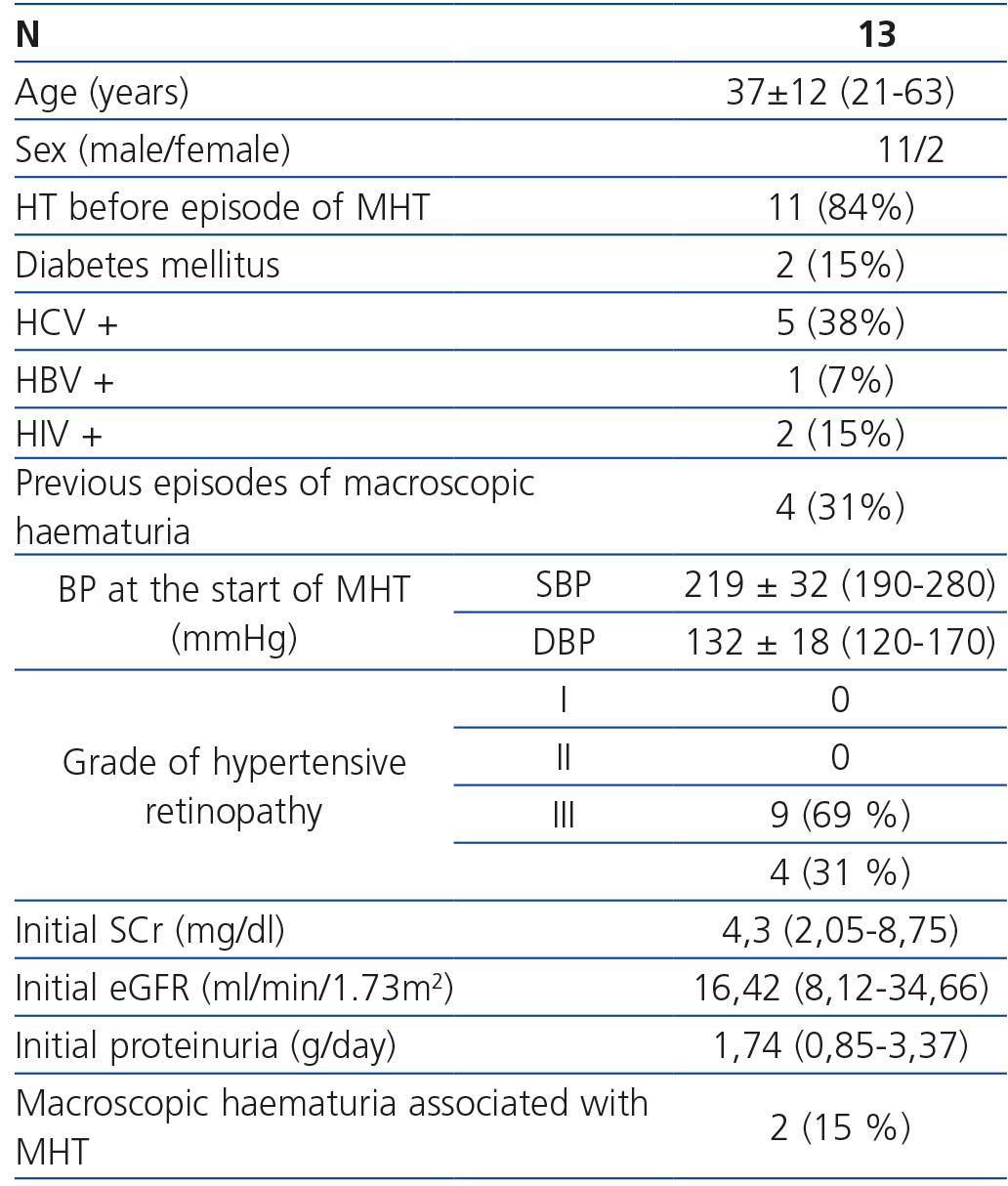
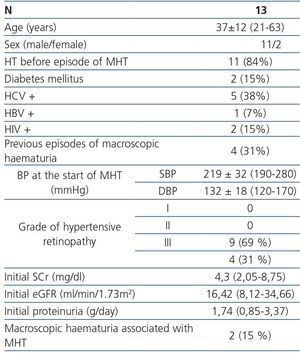
The epidemiological characteristics and the most relevant personal history of the patients are included in Table 1. No patient had previously been diagnosed with IgAN nor had they been studied for suspected kidney disease, although four of them referred to previous outbreaks of macroscopic haematuria. The mean age at the time of renal biopsy was 37±12 (21-63) years. Eleven patients (84%) were male. Five (38%) were seropositive for the hepatitis C virus (HCV), three of which were cirrhotic. One of the patients was co-infected with the human immunodeficiency virus (HIV) and another with HIV and the hepatitis B virus (HBV). No patient was being treated for HCV. The two patients with HIV received highly active antiretroviral therapy. One patient was an occasional cocaine user.
Clinical and laboratory manifestations at admission (episode of malignant hypertension)
As shown in Table 1, the mean systolic/diastolic BP during the MHT period was 219±32/132±18mmHg. All patients had renal failure at admission: SCr 4.3 (2.05-8.75) and eGFR 16.42 (8.12-34.66) ml/min/1.73 m2. Non-nephrotic proteinuria was detected in all patients: 1.74g/day (0.85-3.37g/day) and haematuria. Haematuria was macroscopic in two cases (15%) and microscopic in the remaining cases. No patients had laboratory data suggestive of thrombotic microangiopathy: anaemia with thrombopaenia, an increase in LDH or the presence of schistocytes in the peripheral blood smear.
Renal biopsy
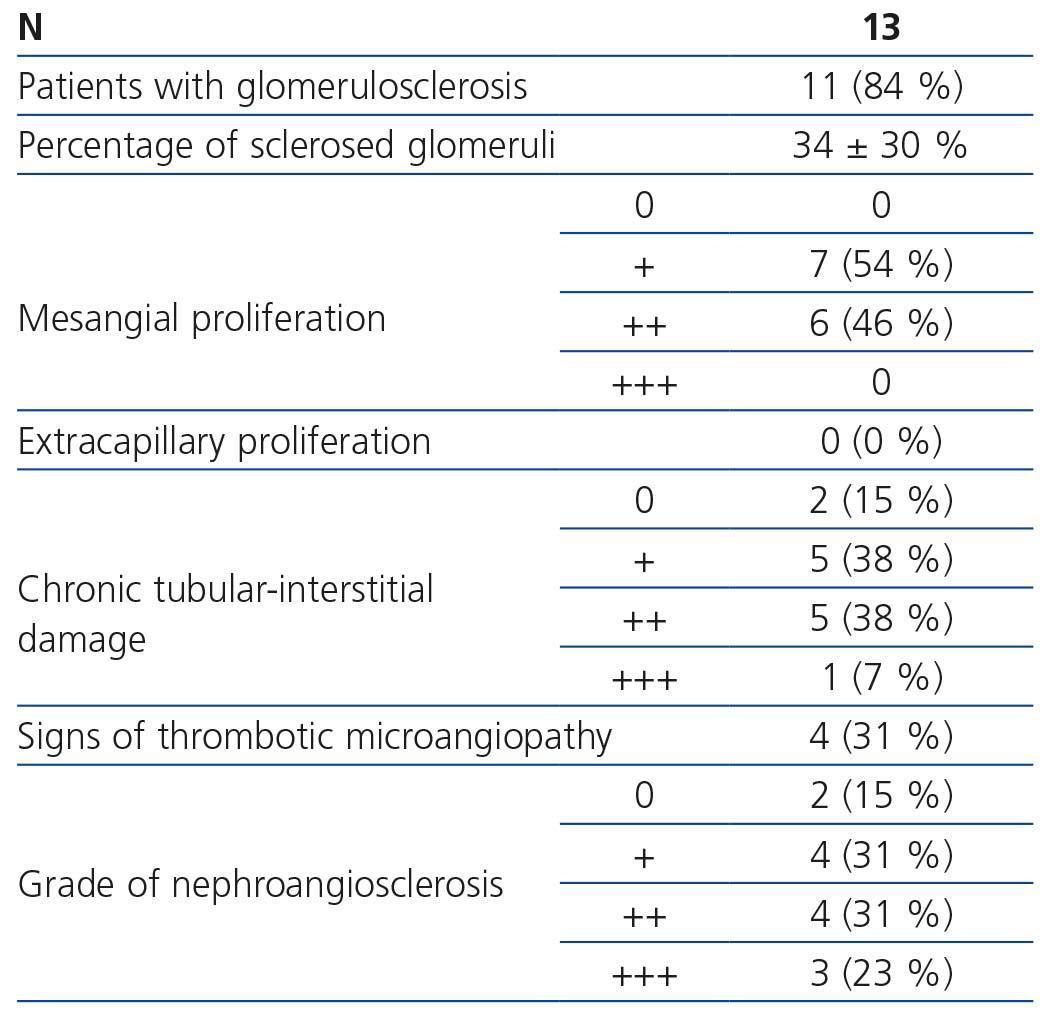
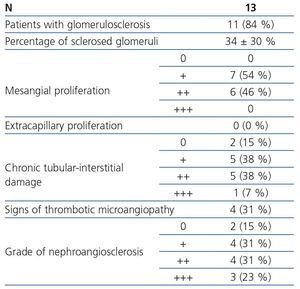
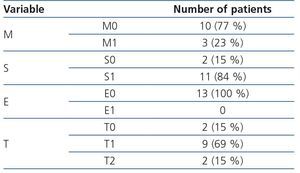
Table 2 summarises the main histological findings and Table 3 summarises their classification using the Oxford classification. In ten patients (77%) an early renal biopsy was performed in the first month after admission due to MHT. In the three remaining patients, the biopsy was performed after 14±8 (6-22) months. A mild mesangial proliferation was the most commonly observed histological finding. We found glomerulosclerosis (segmental or global) data in eleven patients (84%). The mean percentage of sclerosed glomeruli was 34±30%. We observed chronic interstitial damage in eleven patients, whose grade was mainly mild-moderate. By definition, all cases had predominant mesangial deposits of IgA in the immunofluorescence. In one patient, there were also deposits of IgM and in four there was C3. We found thrombotic microangiopathy data in four of the patients (31%). None had extracapillary proliferation. Only two patients did not have nephroangiosclerosis data in the renal biopsy. The grade of nephroangiosclerosis of the remaining patients is displayed in Table 2.
Treatment and long-term clinical course
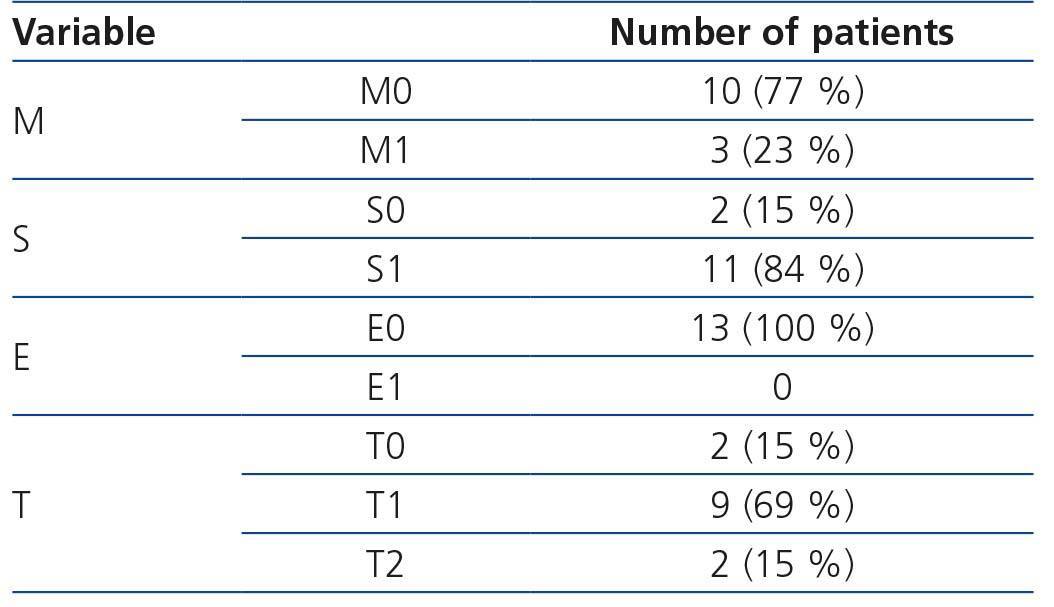
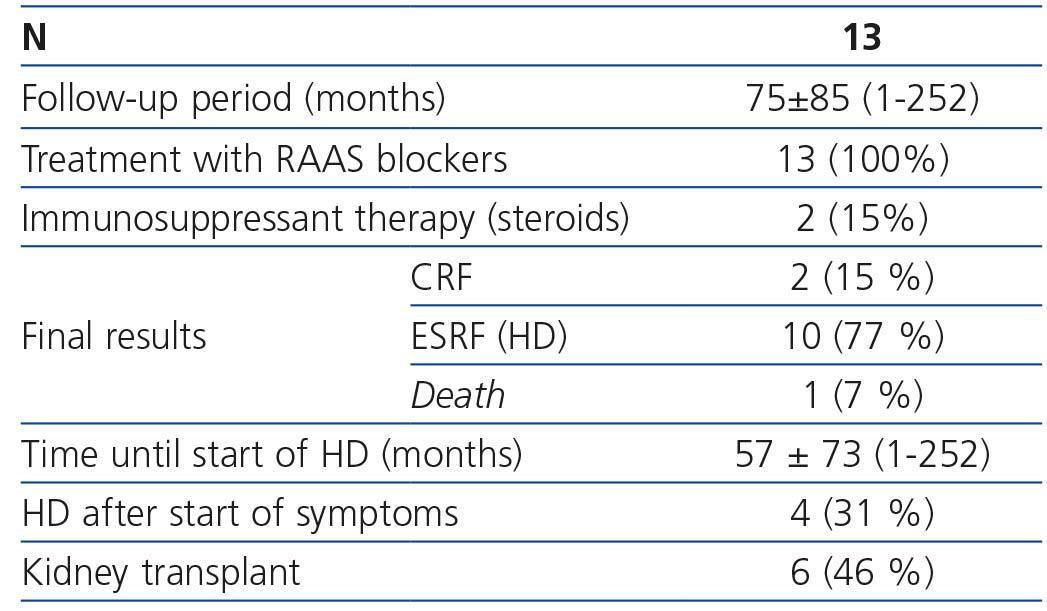
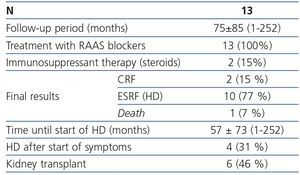
After the diagnosis of MHT, treatment was started with renin-angiotensin-aldosterone (RAAS) blockers in all cases. When necessary, other hypotensive drugs were included in the treatment. In all cases, an adequate blood pressure control was achieved and the visual impairment associated with hypertensive retinopathy gradually disappeared. The RAAS were maintained for the duration of the disease. Two patients received a course of oral steroids after the diagnosis of IgAN.
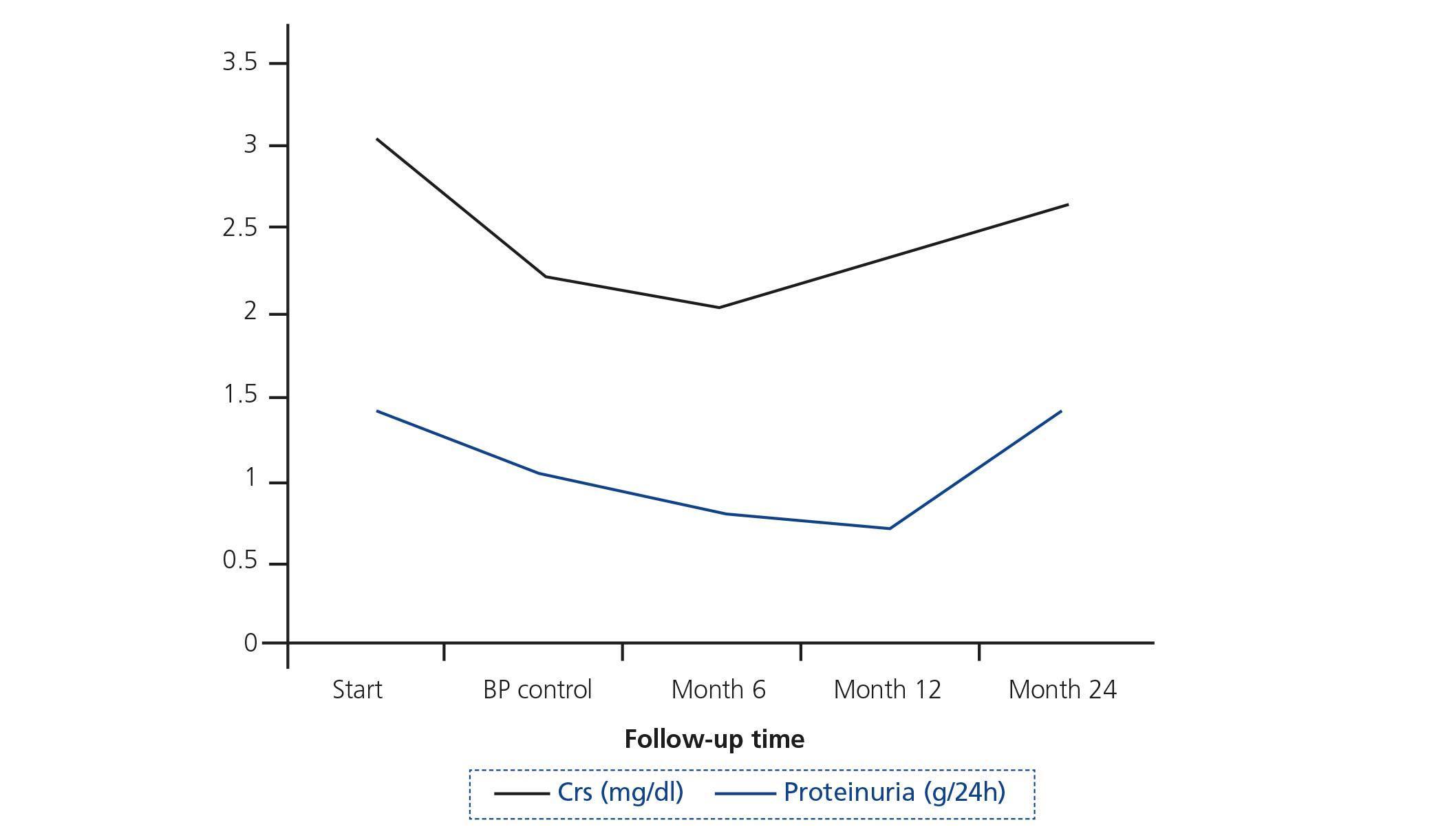
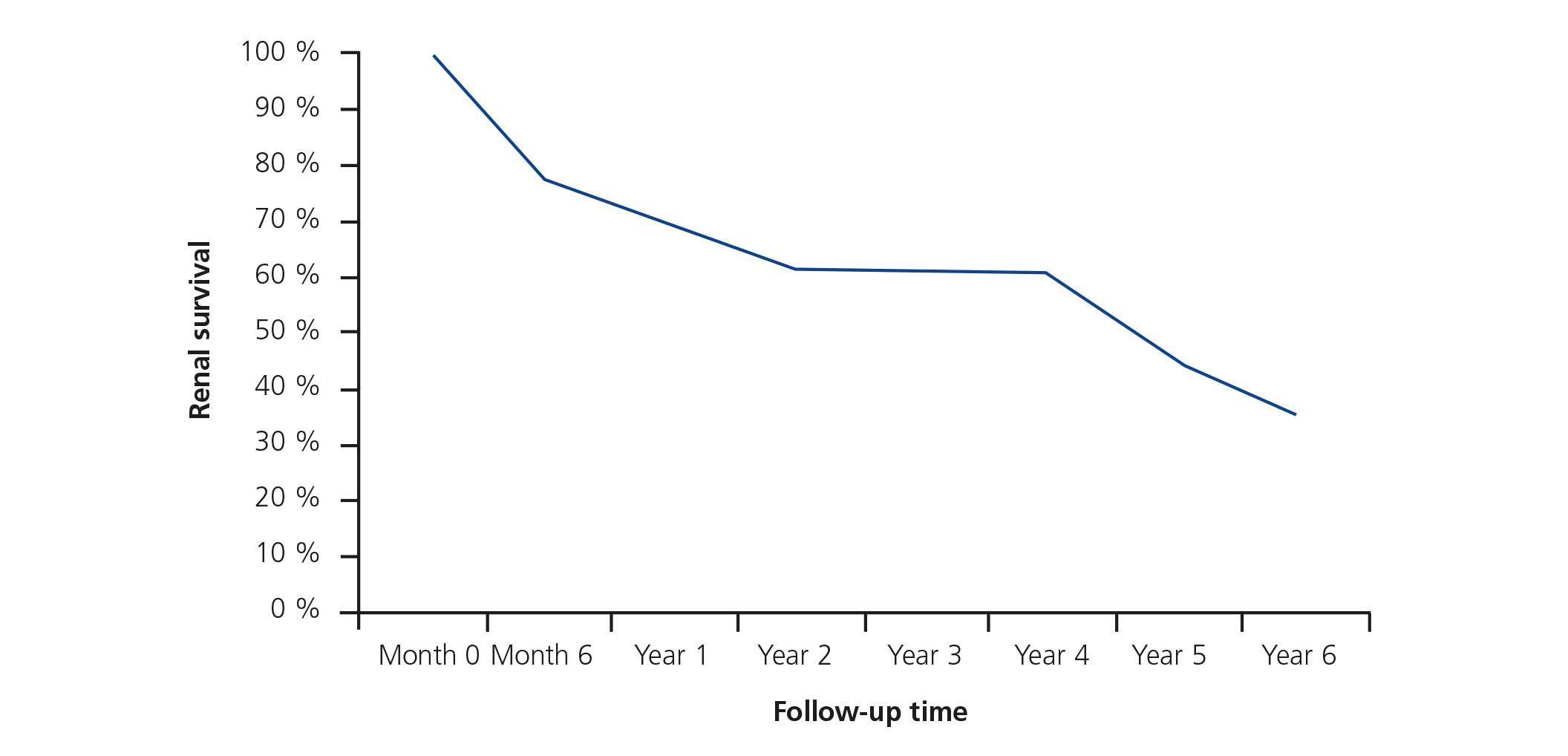
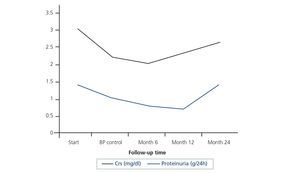
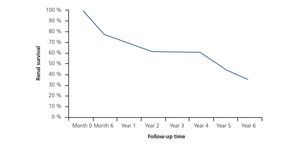
As displayed in Table 4, the mean follow-up time was 75±85 (1-252) months. After the adequate control of BP, the renal function of patients who were not dialysis-dependent somewhat improved. However, from the sixth month after blood pressure control, all patients showed again a progressive deterioration of renal function, which was maintained throughout the rest of follow-up (Figure 2). At the end of follow-up, one patient had died as a result of an ischaemic stroke, ten required haemodialysis (HD) (77%) and the other two remained in follow-up (15%). The mean time until the start of HD was 57±73 (1-252) months. Four patients began renal replacement therapy during the initial admission due to severe renal failure, which did not improve despite the measures established. The two patients who remained on follow-up had chronic renal failure (CRF) with SCr of 2.66 and 2.44mg/dl, an eGFR of 31.04 and 30.82ml/min/1.73 m2 and proteinuria of 1.09g/day and 0.18g/day, respectively. The probability of renal survival in the study population was 69% and 35% after 3 and 6 years of follow-up, respectively (Figure 3).
Kidney transplantation
Six of the patients who reached ESRF received a kidney transplant after 19±18 (5-54) months on HD. At the end of follow-up (137±88 months) 50% of patients had returned to HD due to loss of graft function. The three who did not return to dialysis had SCr of 1.50 (1.22-1.65) mg/dl, an eGFR of 57.29 (47.17-67.10) ml/min/1.73m2 and proteinuria of 0.70 (0.60-2.03) g/day. Biopsies were taken in five patients due to deterioration of renal function or proteinuria. In four of these patients we observed data consistent with IgAN recurrence combined with chronic allograft nephropathy (CAN) data. Despite the three patients who returned to HD having recurrence of the IgAN, the cause of graft loss in all patients was attributed to CAN.
One patient had an episode of thrombotic microangiopathy with HELLP criteria (microangiopathic haemolytic anaemia, thrombopenia and an increase in transaminases) during pregnancy. We detected new MHT in association with this condition with very high BP levels and grade III hypertensive retinopathy. The symptoms resolved when the pregnancy was ended by caesarean section and since that time the patient has had controlled BP and stable renal function.
DISCUSSION
MHT is, along with nephrotic syndrome and acute renal failure, one of the atypical manifestations of IgAN1. These manifestations, although less common, are important, since they may complicate the diagnosis of IgAN and their onset affects the clinical course and treatment of the disorder2.
Despite the literature on IgAN-MHT4-16, there is very little information on the long-term prognosis and the effectiveness of BP control or other types of treatment in these patients.
The prevalence of MHT in IgAN varies in accordance with the geographical region. In Europe, it is around 7%-15%7-9 and in Asia it is around 1.2%4. However, in Asian countries, IgAN is defined as one of the most common causes of secondary MHT10. In our series, MHT represented 7% of the cases of IgAN (13 out of 186). It is possible, moreover, that the prevalence may be greater, taking into account that in a significant amount of cases of MHT no renal biopsy is performed, either due to the severity of the MHT or the CRF or due to the assumption that they are cases of malignant essential HT. As such, the presence of haematuria, significant proteinuria and high serum IgA in a patient with MHT must make us suspect that it is an IgAN with this clinical manifestation. Likewise, the absence of the clinical profile characteristic of the essential HT (absence of family history, age <30-40 years, the absence of associated factors such as obesity or smoking) should also indicate secondary causes of MHT, including IgAN4,5,9.
In the past it was postulated that patients with IgAN who had outbreaks of MHT had advanced CRF or ESRF, and that this renal failure could explain the onset of MHT due to poor volume control and other factors associated with CRF8,9. However, studies carried out a posteriori, in which it was demonstrated by renal biopsy that more than half of the patients with MHT and IgAN had only moderate lesions at the histological level without much chronicity data, refute this hypothesis11. The histological findings of our series are consistent with those published in more recent studies, showing only a mild-moderate grade of glomerulosclerosis and interstitial fibrosis (Table 2). Another interesting piece of data is that only four of our patients had thrombotic microangiopathy data in the biopsy in contrast to that observed in the French series, in which all those with MHT had this histological finding7.
The pathogenesis of IgAN-MHT is completely unknown. One study showed a higher prevalence of antibodies against endothelial cells in patients with IgAN-MHT than in those with IgAN without MHT or cases of essential MHT11. However, no more studies have been published in this regard and we do not have information on the causes of these anti-endothelial cell antibodies in patients with IgAN-MHT. It has also been reported that certain mutations in the genes that regulate the release of chromogranin are more common in patients with MHT-IgAN than in the control groups6. An attractive hypothesis would be the involvement of a deregulation of the complement system, particularly of the alternative pathway, in the pathogenesis of these cases. The abnormal activation of the complement in practically all types of thrombotic microangiopathy17 and the importance that the abnormalities in this system seem to have in the pathogenesis of IgAN and on the severity of its clinical expression18-21 make this possibility plausible.
One piece of data that must be highlighted from our study is the poor renal prognosis of patients with IgAN-MHT. Despite there being an initial improvement after blood pressure control (Figure 2), of the thirteen patients included, 77% required in dialysis and up to 31% began renal clearance techniques immediately after the outbreak of MHT. The two patients who did not begin dialysis finished follow-up with advanced CRF (eGFR of 30.03±0.15ml/min/1.73m2). The Kaplan-Meier curves displayed renal survival of 69% and 35% after 3 and 6 years respectively. This poor clinical course of the disease had already been reported in previous publications. As such, in the experience of the two groups, the probability of reaching HD in two IgAN-MHT patient cohorts was 60% and 80% after 14 and 55 months respectively7,9. This renal survival was significantly lower than that observed in the control groups, patients with IgAN without MHT.
It is also important to stress that MHT associated with IgAN results in a significantly worse prognosis than that of patients with malignant essential HT, which is the most common MHT group. In a previous study in our group on the long-term prognosis of a cohort of 197 patients with malignant essential HT, 75% had an improvement or stabilisation of baseline renal function and renal survival was 85% and 72% after 5 and 10 years respectively22. 63% of patients had renal failure at admission and the initial mean creatinine was 2.49±2.9mg/dl (0.6-24.9). Despite these poor prognosis data, BP control with intensive antihypertensive treatment, which prioritised RAAS blockers, resulted in a favourable outcome in most patients22. By contrast, patients with IgAN-MHT in this study had a uniformly unfavourable outcome despite good control of BP and the use of RAAS in all cases. Two of them also received steroids, but no favourable effect was observed.
The mortality rate in individuals diagnosed with MHT was very high until the latter decades of the last century. After the introduction of RAAS blockers, this mortality decreased significantly22,23. In our case series it is highlighted that, despite poor renal survival and the fact that many patients were diagnosed with MHT in the nineteen-eighties, only one patient died during follow-up.
No treatment has shown to be effective in IgAN-MHT in preventing the progression of renal damage. Antihypertensive treatment is, logically, essential in patients with MHT and it seems reasonable that RAAS blockers should form a central part of the therapy, with the results extrapolated from other studies22,24. But there is no evidence that this control of BP will slow down the progression of renal damage as our cases illustrate and in contrast to what occurs in other types of MHT. Moreover, the potential involvement of an abnormal activation of the complement in cases of IgAN-MHT may trigger the use of eculizumab, a C5 inhibitor that has shown great efficacy in the atypical haemolytic-uraemic syndrome and in various other microangiopathies25, in the treatment of this disorder. To date only one case of the efficacy of eculizumab in the treatment of an aggressive IgAN with extracapillary proliferation has been reported26. Although the patient was hypertensive, there was no indication that he had MHT. Greater experience and further knowledge is required on the pathogenesis of the disorder in order for eculizumab to be recommended in the treatment of this condition.
Five of our patients had HCV infection, three of them with cirrhosis criteria. One of the patients was HIV-positive and another was HBV-positive and HIV-positive. The onset of IgAN was reported in both HIV-positive and HCV-positive patients, but the pathogenesis of its association was unclear27-30. The association between MHT and HIV is also known and is particularly common in patients with a glomerulopathy, particularly IgAN31. However, in the large MHT-IgAN series, this association with HCV, HBV and HIV has not been reported.
Our case series is the only one published in the literature in which there was follow-up of patients who received transplants after reaching HD. IgAN reappeared in 66% of the six patients who received transplants. There is recurrence of IgAN in patients with kidney transplants in approximately 33% of cases, with this prevalence varying between 9% and 61% depending on the series32. Despite all patients with transplants being on treatment with calcineurin inhibitors, drugs whose side effects include causing HT and occasionally thrombotic microangiopathy, only one patient had new symptoms of MHT within a HELLP thrombotic microangiopathy during pregnancy. The strict control of BP that is undertaken in transplant patients, thanks to the strict follow-up that they undergo in the clinic, may explain the non-recurrence of MHT.
In conclusion, MHT is a non-exceptional manifestation of IgAN (7% of cases in our experience), accompanied by acute deterioration of renal function in all cases and a very poor renal prognosis. By contrast, mortality was low, with only one death during follow-up. We must suspect the existence of an IgAN in a patient with MHT when the latter has haematuria (micro- or macroscopic), proteinuria or their clinical profile is different to the normal clinical profile in malignant essential HT. The pathogenesis of this complication is unknown and we do not possess specific treatments, apart from the essential intensive HT treatment. Studies that explain the pathogenic pathways are necessary in order that we may develop new therapeutic possibilities.
Acknowledgements
This study was partially funded with grants from the Fondo de Investigaciones Sanitarias (10/02668 and 10/02581), the Asociación para la Investigación y estudio de las Enfermedades Renales (AITER), REDinREN (RD012/0021), the FIS programme (Miguel Servet Programme: CP10/00479, PI13/00802 and PI14/00883) and the Sociedad Española de Nefrología to Juan Antonio Moreno. We also thank the research group “Complemento-Comunidad de Madrid” (S2010/BMD-2316) for its collaboration.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Characteristics at diagnosis
Table 2. Histological characteristics of the renal biopsy population
Table 3. Histological findings using the Oxford classification
Table 4. Treatment and clinical course
Figure 1. Year in which patients were diagnosed with IgA nephropathy and malignant hypertension
Figure 2. Evolution of renal function and proteinuria in patients who did not start dialysis immediately
Figure 3. Renal survival in our population