Organ donation is a voluntary, selfless and altruistic act. There have been advances in the development of procedures to improve clinical, surgical and logistical processes of transplants. Every country has also developed strategies to enhance the process of donation. In Colombia, the Red de Donación y Trasplantes de Órganos y Tejidos (Organ and Tissue Donation and Transplant Network), organisations related to donation processes have been operating since 2004.1
Despite these efforts, the refusal to donate organs is currently a major issue, which may reflect myths and beliefs held by society.
Surveys of public opinion show that only 75% favour donation. Of all potential donors (PD) worldwide, 85% took part in a family interview and only 47% gave their consent to donate.2
The refusal to donate organs is based on people's myths, beliefs and perceptions. These fears influence families’ decisions to refuse to give consent to donate their deceased relatives’ organs.3
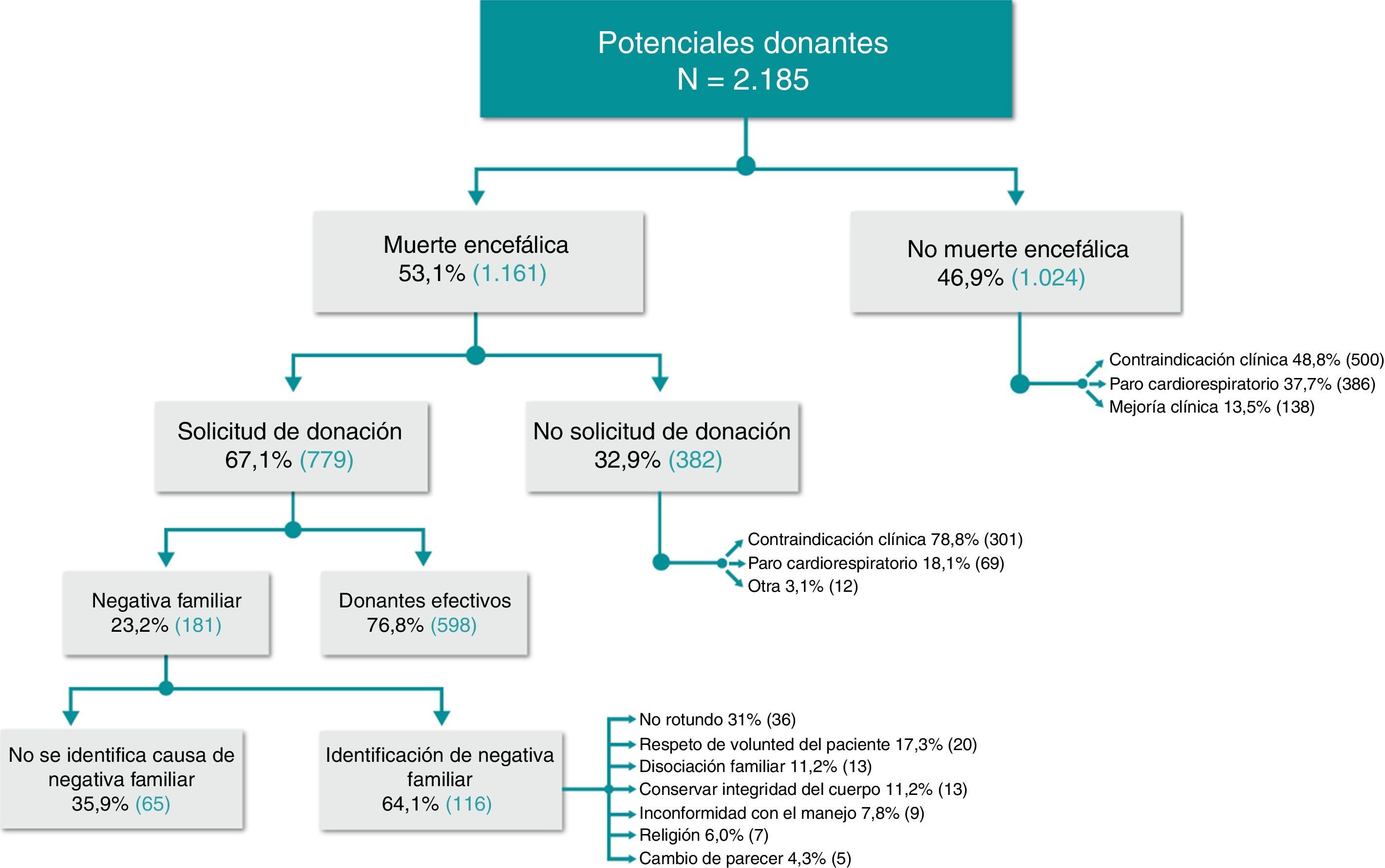
We carried out a retrospective observational study at the Clínica Fundación Valle del Lili (FVL) in Cali, Colombia, aiming to of identify the main causes for donor exclusion, the arguments against and the obstacles for organ donation. This information was obtained by reviewing the FVL Transplant Unit's record of effective and ineffective donors from January 2007 to April 2016. As many as 2185 PD were included; 1.024 patients were excluded because they did not progress to brain death (BD).
In patients diagnosed of BD (n=1161), 33% of cases were not asked for donation due to clinical contraindication (78.8%), cardiopulmonary arrest (18%) or other causes (3%).
An organ donation was requested in 67% of families of patients with a diagnosis of BD. A total of 23% of families refused and the reason for this refusal was recorded in 64% of cases (Fig. 1).
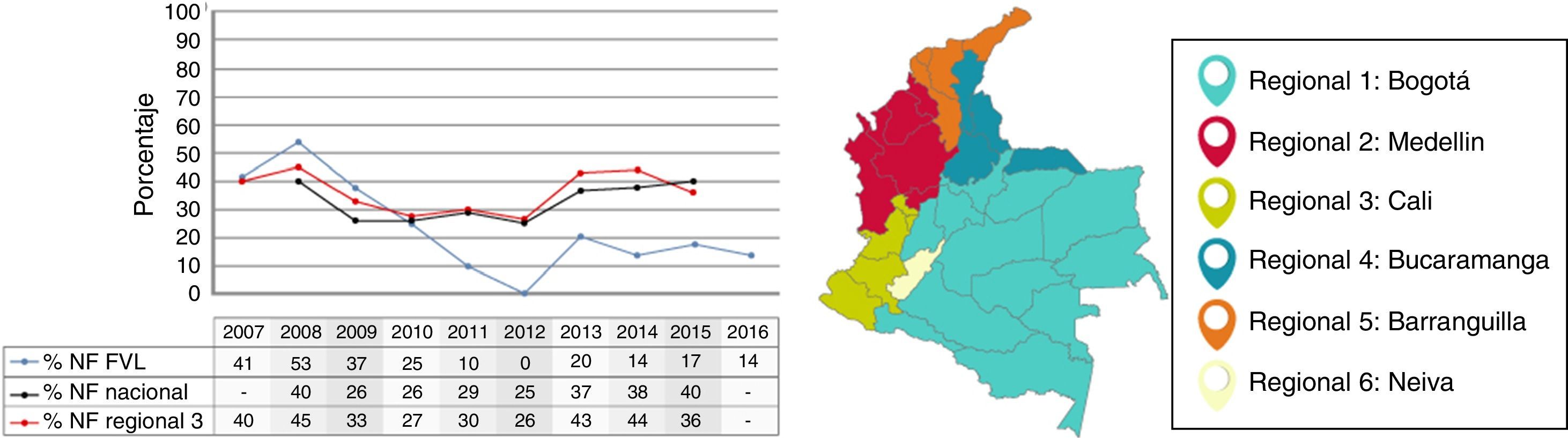
The percentage refusal of organ donation in the FVL during the study period is lower than the national figures (Fig. 2). This can be explained by the implementation of transplant coordination education programmes for healthcare professionals responsible for approaching families, as well as the introduction of training on Operational Coordination of Transplants, diploma obtained at the University of Icesi/FVL. These educational strategies have improved the medical treatment process of potential donors, the protocol for approaching families and its organisation.
Gómez et al. report 10 causes of family refusals obtained from a multicentre study in Spain between 1993 and 1994; the most common was the “assumed refusal of the deceased when he was alive” (40.7%), followed by “the family does not want” (24%).4 In our experience, a “flat refusal” by the family was recorded in 31% of cases, and in 17% the negative was related to “a respect of the patient's wishes” in contrast with the report from Spain.
Other reasons for family refusals such as “wishes of the relative while he/she was alive of not being a donor” and the family dissociation highlight the importance of communicating their wishes to relatives whilst still alive. There was also limited information on organ donation and a poor understanding about the diagnosis of BD, which was barrier for organ donation.5
According to the 2001 report by Cuende et al.,6 between 1998 and 2000, family refusals were responsible for between 23% and 25% of lost PD with BD, which is similar to our findings. However, in the report which covers the years 1998–2013, family refusal fell to 10.9% of the total interviews.7 Our rate of refusal is 23%, which suggests that strategies to be more assertive with PD families should be implemented.
Following the Spanish model of organ and tissue donation,8 the FVL has established itself as a “donor hospital” since 2014. This is an institutional campaign to promote the education of healthcare professionals and associated people from the academy, making them aware of the importance of implementing an organised and humanised process of donation.
In conclusion, based on our experience, it is important to continue with a protocolised process for approaching the families of potential organ and tissue donors both in transplant hospitals and in PD-generating hospitals. In addition, education of doctors, healthcare professionals and society is key to overcoming the myths, fears and perceptions related to the refusal to donate organs and tissue.
Please cite this article as: Molina MI, Toro PA, Manzi E, Dávalos D, Torres K, Aristizábal AM, et al. Principales causas de negativa familiar a la donación de órganos y tejidos: 10 años de experiencia en un centro latinoamericano. Nefrologia. 2018;38:225–227.