Despite the benefits of physical exercise (PE) for patients with chronic kidney disease (CKD), the number of Nephrology services that have PE programs is limited.
ObjectivesTo describe the degree of knowledge of PE benefits in patients with CKD among professionals, as well as the level of implementation and characteristics of PE programs in Nephrology services in Spain.
MethodsA questionnaire on the degree of knowledge and prescription of PE in patients with CKD was designed and sent to members of the Spanish Nephrology and Nephrology Nursing Societies, as well as to physiotherapists and professionals in the Sciences of Physical Activity and Sport (PASS).
Results264 professionals participated. 98.8% agreed on the importance of prescribing PE, but only 20.5% carry out an assessment of functional capacity and 19.3% have a PE program for patients with CKD in their centre. The most frequent programs are performed for haemodialysis patients and strength and aerobic resistance exercises are combined. A physiotherapist or a PASS usually participates in its prescription. The main barriers were the absence of human and/or physical resources and the lack of training.
ConclusionsHealthcare workers know the benefits of PE in patients with CKD. However, the implementation of these programs in Spain is low, motivated by the lack of resources and training of professionals. We must establish strategies to guarantee an adequate functional capacity within the care of our patients.
A pesar de los beneficios del ejercicio físico (EF) para pacientes con enfermedad renal crónica (ERC), el número de servicios de Nefrología que han implementado programas de EF es limitado.
ObjetivosDescribir el grado de conocimiento del EF en pacientes con ERC entre los profesionales, así como el nivel de implementación y las características de los programas de EF en los servicios de Nefrología en España.
MétodosSe diseñó un cuestionario sobre el grado de conocimiento y de prescripción del EF en pacientes con ERC que se envió a los socios de la Sociedad Española de Nefrología y de la Sociedad Española de Enfermería Nefrológica, así como a fisioterapeutas y profesionales de las Ciencias de la Actividad Física y del Deporte (CAFyD).
ResultadosParticiparon 264 profesionales. El 98,8% coincidían en la importancia de prescribir EF, pero solo el 20,5% realizan una valoración de la capacidad funcional y solo el 19,3% disponen de un programa de EF para pacientes con ERC en su centro. Los programas más frecuentes están dirigidos a pacientes en hemodiálisis y combinan ejercicios de fuerza y de resistencia aeróbica. En la prescripción habitualmente interviene un fisioterapeuta o un PASS. Las principales barreras fueron la ausencia de recursos humanos y/o físicos y la falta de formación.
ConclusionesLos profesionales sanitarios conocen los beneficios del EF en el paciente renal. Sin embargo, la implementación de estos programas en España es baja, debido a la falta de recursos y a la falta de formación de los profesionales. Debemos establecer estrategias para garantizar una adecuada capacidad funcional dentro de los cuidados de nuestros pacientes.
Physical exercise (PE) significantly benefits patients with chronic kidney disease (CKD). It contributes to a better control of cardiovascular risk factors and improves aerobic and functional capacity. It also reduces fatigue, anxiety and depression.1–6 In addition, the prevalence of CKD is higher in patients with a sedentary lifestyle, which is an important cause of development of kidney disease.7 For all these reasons, one of the primary measures to prevent the appearance and progression of CKD is to include the practice of PE since the initial stages.8,9
However, 47%–60% of CKD patients have a sedentary lifestyle.8,10–12 Several studies have analysed the barriers to doing PE in CKD patients and concluded that generally they receive little information from their nephrologist about how PE impacts their health and the progression of their kidney disease, as well as a limited variety of exercises, hindering motivation and adherence.13,14 Other studies affirm that most nephrologists do not regularly advise their patients on the practice of PE, mainly due to lack of time and knowledge on how to prescribe it properly.12,15–20 All this suggests the need to evaluate effective and efficient counselling strategies and emphasises the role of the participation of exercise specialists in the care of patients with CKD.19,20
There is a growing number of nephrology services and dialysis centres that are implementing PE in kidney patients in Spain. However, still they are limited in number. For this reason, aiming to gain an understanding of the current situation of PE programmes in kidney patients in Spain, the Grupo Español Multidisciplinar de EF en el Enfermo Renal [Spanish PE Multidisciplinary Group in Renal Patients] (GEMEFER) of the Spanish Society of Nephrology proposed a survey as a starting point for the design of its action plan for the coming years.
Material and methodsSurvey participants and disseminationGEMEFER designed a questionnaire on the degree of knowledge about and prescription of PE in patients with CKD. Nephrologists, nurses, physiotherapists and graduates in Physical Activity and Sports Sciences (Ciencias de la Actividad Física y el Deporte, PASS) participated. The survey was distributed through the official communication channels of the Spanish Society of Nephrology, the Spanish Society of Nephrology Nursing (Sociedad Española de Enfermería Nefrológica), the Spanish Association of Physiotherapy (Asociación Española de Fisioterapia) and the Official College of Graduates in PASS (Colegio Oficial de Graduados en PASS). The professional's decision to complete the survey was interpreted as consent to participate. The response recruitment period was from 15 March 2021 to 15 May 2021.
Drafting of the survey and questionnaireThe survey was electronic, using the Google Forms platform, and allowed a single response per person. It consisted of 19 questions, prepared according to surveys conducted by other groups with a similar design.16,18,19,21 The following information was collected: a) demographic data; b) professional data; c) perception of the degree of knowledge of the impact of PE in renal patients and attitude towards the prescription of physical activity; d) situation regarding the assessment of functional capacity and the prescription of exercise in renal patients at the professional's centre; whether there were protocols for the assessment and prescription of physical activity, information was requested on the functional tests used, the type of exercise prescribed, to which patients it is directed and the professional making the prescription; e) barriers to implementing a PE programme, and f) suggestions for contributions from GEMEFER.
The survey included dichotomous questions (yes/no) and multiple-choice questions. The degree of agreement with the questions about subjective perception was measured using the 5-point Likert scale, with 1 being "never" or "not at all" and 5 being "always" or "extremely". A free text option was available to respond to the "other" option in the multiple choice questions, to list the functional tests used, to identify the barriers in implementing the programmes and to send suggestions to the group.
Data analysisA descriptive analysis of the responses received was performed. The questions with qualitative variables are described by their absolute and/or relative frequency and the quantitative variables by mean and standard deviation. The statistical analysis was performed with the SPSS software, version 20.0 (NY, USA).
ResultsRespondents' profileTwo hundred and sixty-four professionals participated, of which 73.1% were women; the mean age was 45.2 ± 10.9 years. The professional group with the greatest representation was nursing (43.9%); in a second position were nephrologists (36.7%), followed by PASS (13.6%) and physiotherapists (1.9%). The remainder is represented in a smaller percentage and corresponds to other categories. Sixty-one point four percent of those surveyed reported to be working in a university hospital, 17.8% in an external dialysis centre and 10.2% in a non-university hospital. Regarding the percentage of participation by autonomous communities, the Community of Madrid was the community that provided the greatest number of responses (28%), followed by Catalonia (13.6%), Andalusia (12.9%) and the Valencian Community (7.2%).
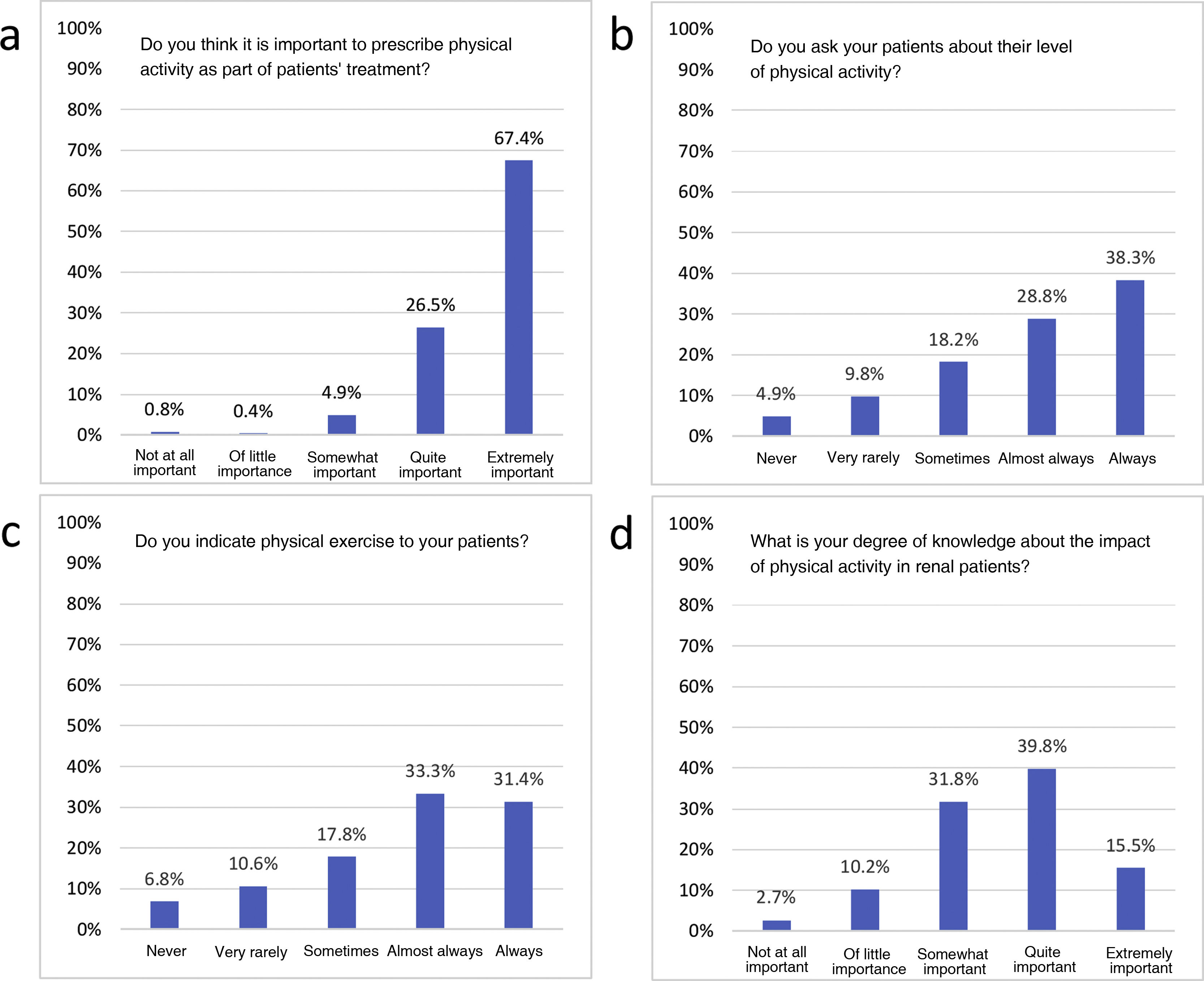
Degree of knowledge and prescription of physical exerciseNinety-eight point eight per cent of the participants agreed on the importance of the prescription of PE as part of the treatment of patients with CKD (Fig. 1a), 85.3% questioned patients about their level of physical activity (Fig. 1b), and 82.5% said they indicate exercise (Fig. 1c). Likewise, 55.3% of the participants stated that they knew "quite a lot" or "a lot" about the impact of PE on renal patients (Fig. 1d).
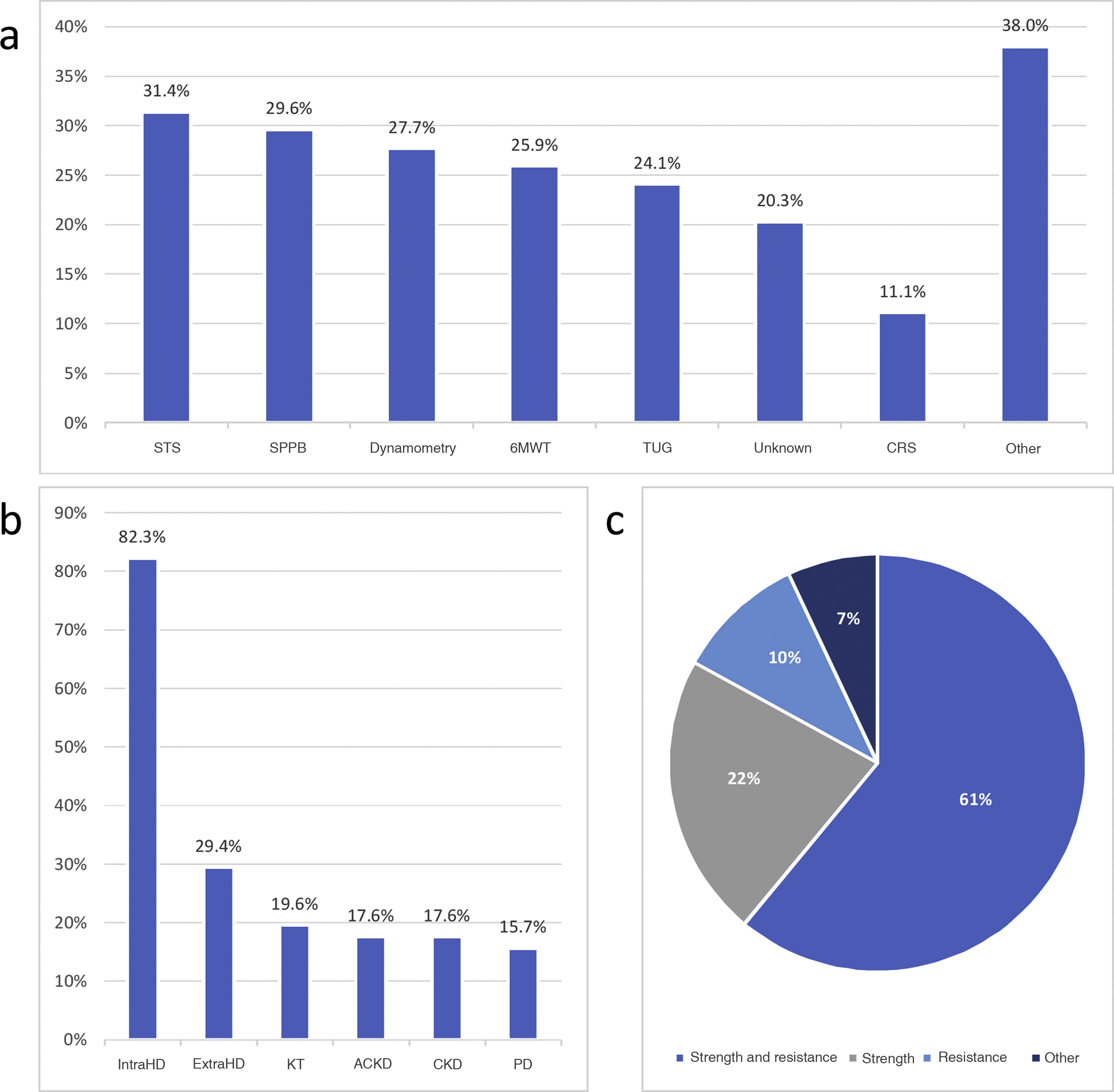
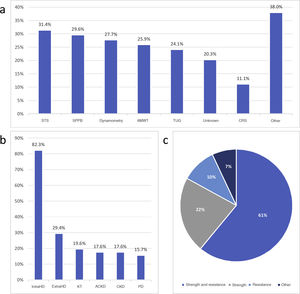
Assessment of functional capacity and implementation of physical exercise programmes in kidney patientsOnly 20.5% of those surveyed stated that they carried out a standardised assessment of functional capacity of patients in their workplace. The most frequently used tests were the Sit to Stand Test (in its ⋅10 times, ⋅5 times and 30 s variants) (31.4%), the Short Physical Performance Battery (29.6%), dynamometry (27.7%), the 6 min Walk Test (25.9%), the Timed Up and Go Test (24.1%) and the Chair Sit and Reach Test (11.1%). However, we found a wide variety of applied tests, although with an individual representation by centres. Twenty-point three percent of the participants were unaware of the tests used (Fig. 2a).
Assessment level of functional capacity and characteristics of physical exercise programmes in renal patients. (a) Functional tests used to assess functional capacity. (b) Group of patients to whom the exercise programme is directed. (c) Professional in charge of prescribing the exercise.
6MWT: 6 min Walk Test; ACKD: advanced chronic kidney disease; CKD: chronic kidney disease; CRS: Chair Sit and Reach Test; HD: haemodialysis; KT: kidney transplant; PD: peritoneal dialysis; SPPB: Short Physical Performance Battery; STS: Sit to Stand Test; TUG: Timed Up and Go Test.
Nineteen point three percent of those surveyed reported working in a centre that has a PE programme for patients with CKD. Most of these programmes were targeted towards haemodialysis patients, mainly intradialytic (82.3%) and, to a lesser extent, extradialytic (29.4%). Patients on peritoneal dialysis were those with the lowest representation within the PE programmes (15.7%) (Fig. 2b).
A physiotherapist or a PASS usually intervenes in the prescription of the training programme (72.6%). The nephrologist also participated in 27.4% of the centres, and nurses in 17.6%. The most frequently prescribed programmes combine resistance and aerobic resistance exercises (Fig. 2c).
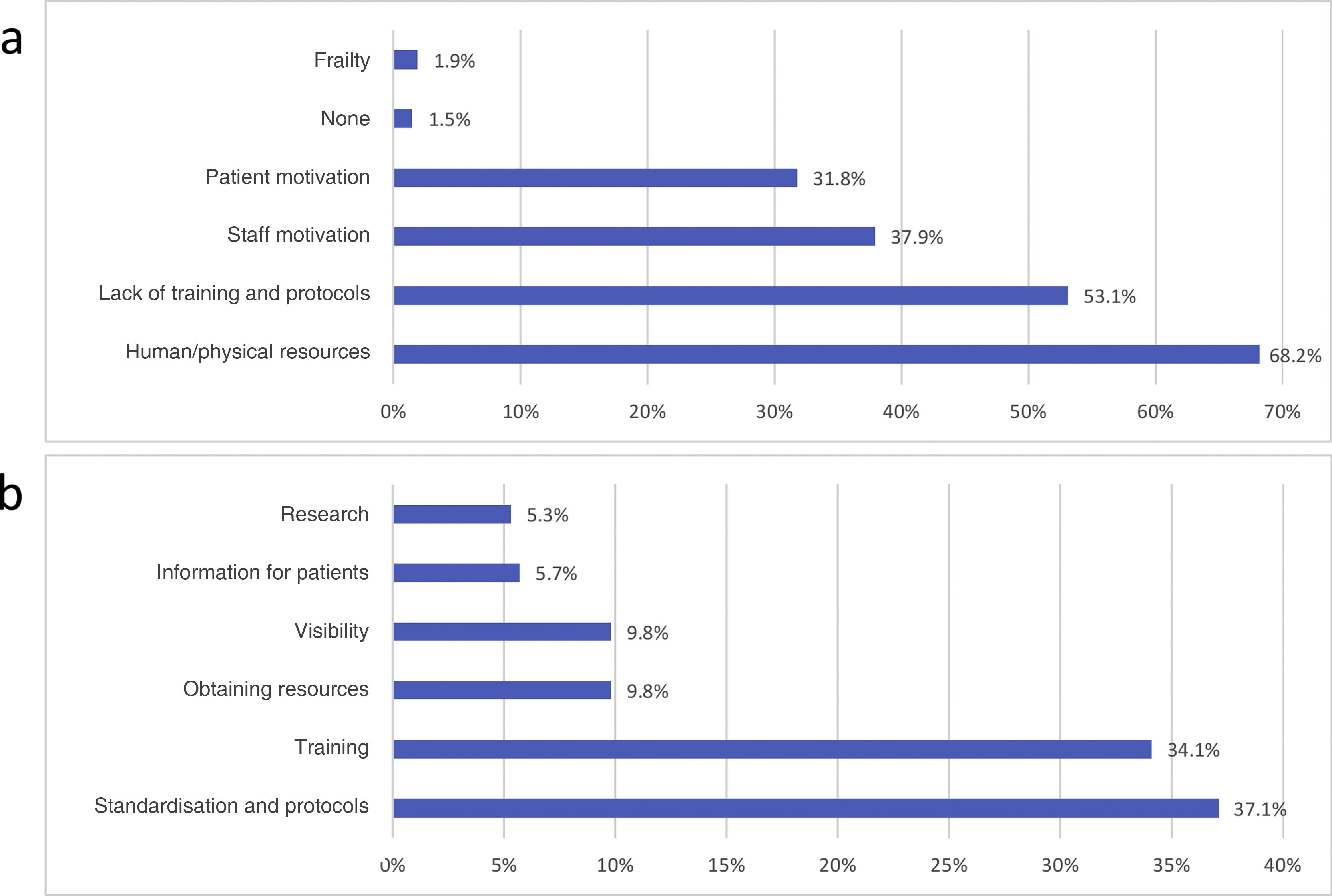
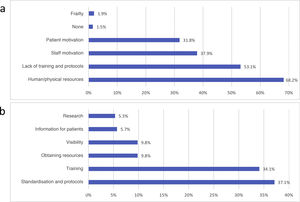
Barriers identified and suggestions for improvementThe main barriers identified for the implementation of PE programmes were the lack of human and/or physical resources (68.2%) and the lack of training and protocols (53.1%) (Fig. 3a).
Regarding suggestions to the group for contributions, it stand out training activities for professionals (34.1%) and the development and dissemination of standardised protocols (37.1%) (Fig. 3b).
DiscussionWe present the results of a survey on the current situation regarding PE programmes in renal patients in Spain, this being the first data available in this country. It is revealed that although the level of knowledge and interest of the nephrologists and the rest of the team's professionals regarding the benefits that exercise brings to CKD patients is high, the implementation of these programmes is still low and only a 20% reported that their centre has them available.
Our data is similar to that reported in other countries, reflecting the poor implementation of PE programmes in nephrology units.12,19 In recent years, the number of publications on the benefits of PE in CKD patients has increased exponentially. These data are reflected in our survey results, in which we found that the degree of knowledge of participants about the advantages of exercise in patients with CKD is high. However, there may be biases, since the professionals who participated are those most interested, this contrasts with the fact that one of the most significant barriers they mention is the lack of training and protocols. From this statement it follows that the deficiency is mainly regarding how to prescribe exercise correctly. These results are shared by professionals from other parts of the world, who consider that, although exercise is important and beneficial for CKD patients, they do not feel confident enough to advise them on such matter.10,12,15–19
This point seems to be the origin of the main barrier identified by those surveyed: the lack of resources, both human and physical. The elevated comorbidity of patients with CKD and the complexity of its management make it difficult for the nephrologist or nurse to prescribe PE. By the same token, to achieve maximum benefit and reduce risks, an individualised prescription and a specific exercise goal indicated by experienced personnel, such as physiotherapists and PASS, are necessary.13,21–23 However, there is a shortage of these professionals in hospitals, and they are usually ascribed to specific units. The units that they most frequently collaborate with are usually dialysis centres, and their contracts requires external financing.24 This point deserves special attention, since, as reflected in our survey, almost 75% of the PE programmes for patients with CKD in Spain are prescribed by physiotherapists and PASS. Therefore, in order to safely increase the prescription of PE in our patients, it is necessary the presence of these professionals in public system dialysis units and hospitals.
Lack of material and physical resources is another of the barriers identified. It would seem that a large number of elements are needed for the functional assessment of our patients and the implementation of a PE programme. Our results identified that the most widely used tests are simple, do not require additional material, and can be applied in the routine assessment of our patients. We hope that sharing this data will facilitate the implementation of these programmes in the rest of the units. Furthermore, the Spanish Society of Nephrology has recently published the "Guidelines for the practice of individualised physical exercise in haemodialysis", which describes the types of exercise recommended and the necessary materials, demonstrating that these are generally low-cost elements that are readily available.25
The GEMEFER Working Group came about as a response to these challenges, advocating the need for an integrated and multidisciplinary management of PE in renal patients. In addition to all the professionals, the group also includes CKD patients, who will ultimately benefit from their recommendations. Since the group was set up in 2018, work has been done to disseminate the benefits of PE for renal patients by inviting presentations at different workshops and conferences at the Spanish Society of Nephrology congresses. Although the current pandemic situation has limited the activity of the group, tele-contact between members has been maintained, with regular meetings held and the use made of new technologies to continue carrying out projects, such as the survey indicated here, training webinars and dissemination activities on social networks, all of them with excellent acceptance.
Our work has some limitations, mostly derived from the very open nature of the survey. Firstly, there may be a positive selection bias since it is likely that those professionals who were most sensitive to PE in renal patients were those who responded. However, the number of participants is higher than that reported in other studies with a similar design.15,16,18,19,21 Secondly, we do not have precise information to be sure of the proportion of participating centres with respect to the national total. Among the strengths of the study, it should be noted that it includes different professionals involved in the care of patients with CKD (nephrologists, nurses, physiotherapists and PASS graduates) and that all the communities in the Spanish national territory and the different healthcare settings (hospitals and external dialysis centres) are represented. This heterogeneity in the profile of the respondents is one of the strengths of our work since, as previously discussed, the prescription of PE in patients with CKD must be multidisciplinary.
In conclusion, the professionals involved in the care of patients with CKD in Spain who have responded to the survey are aware of the benefits of PE, and although services increasingly offer this type of intervention to their patients, the road to its widespread implementation in all nephrology units is long. At GEMEFER, we support a joint effort and collaboration between professionals in prescribing PE and renal patient care to achieve the best results. We invite anyone who shares these concerns to walk this path with us.
FundingThis study received no specific funding from public, private or non-profit organisations.
Conflicts of interestThe authors declare that they have no conflicts of interest.