Dear Editor,
IgM nephropathy (IgMN) is a relatively newly described, and still contentious, clinicopathologic entity which presents mainly as idiopathic nephrotic syndrome (INS) in both children and adults. Although, it is widely acclaimed that this lesion was first described in 1978 by two groups led by Cohen et al.1 and Bhasin et al.,2 predominant IgM deposits in the glomeruli, in fact, were first described in renal biopsies in 1974 by Putte et al.3 in patients with persistent or recurrent hematuria. The frequency of IgMN reported in literature has varied from 2% to 18.5%.4-8 We have earlier reported a prevalence of IgMN of 18.5% in native renal biopsies in children presenting with INS in Pakistan.9 The disease is defined by its immunopathologic features: the light microscopic (LM) features being highly variable ranging from minimal change lesion to variable degrees of mesangial proliferation to focal segmental glomerulosclerosis (FSGS).4,5,9 A few studies have also noted small subcapsular crescents in cases of IgMN.4,5 However, up till now, no case of IgMN has been reported presenting with crescentic GN (CresGN). We herein report a case of an 11-year-old child presenting clinically with rapidly progressive glomerulonephritis (RPGN) and the biopsy features of CresGN.
CASE REPORT
An 11-year-old female presented with one month history of generalized body swelling, anorexia and moderate degree of hearing loss. On physical examination, her blood pressure was 150/110mmHg. No past medical history of note was elicited. Family history was unremarkable for renal disease. Abdominal ultrasound showed normal size kidneys. Urine examination revealed 1+ albumin, 15-20 white blood cells (WBCs)/HPF and 6-8 red blood cells (RBCs)/HPF. Her blood urea was 198mg/dL and serum creatinine, 4.5mg/dL. Relevant viral serology was negative. Slit-lamp examination for eye abnormalities was negative.
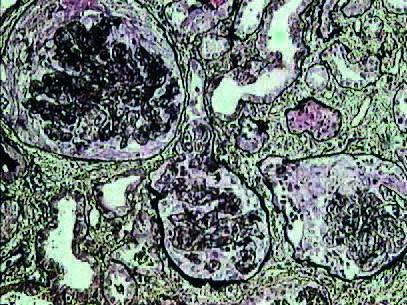
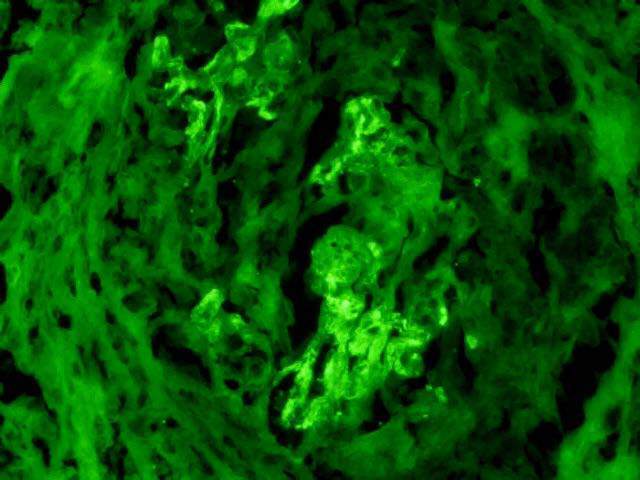
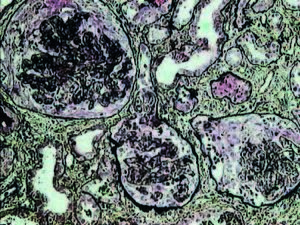
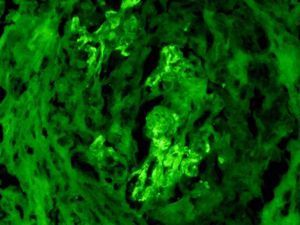
The percutaneous renal biopsy was done, which mostly comprised of medulla with little cortex containing six glomeruli. These showed diffuse severe degree of mesangial proliferation. In addition, three glomeruli showed extracapillary epithelial cell proliferation with the formation of cellular crescents (Figure 1). Mild arteriolosclerosis was seen. Mild degree of tubular atrophy and interstitial scarring was also noted. On immunoflourescence (IF), there was diffuse, bright (3+, on a scale of 0 to 3+) positivity of IgM in the mesangium and peripheral capillary loops, accompanied by C3 and C1q in similar location (Figure 2). IgG and IgA were negative. A diagnosis of IgMN was rendered and lupus serology and serum antineutrophil cytoplasmic antibodies (ANCAs) were advised, which returned negative.
She was given three pulses of methylprednisolone and was started on oral steroids in the standard dosage. Her serum creatinine stabilized at 2.3mg/dL and she was discharged with advice to follow-up in the OPD. Unfortunately, she was soon last to follow-up.
DISCUSSION
To our knowledge, this is the first case of IgMN in literature presenting with full-blown CresGN. The latter is a morphologic expression of severe glomerular injury resulting in rupture of glomerular basement membranes (GBMs) and leakage of fibrin and monocytes into the Bowman’s capsule. This causes reactive proliferation of the visceral and parietal epithelial cells along with influx of macrophages, resulting in crescent formation. CresGN is further classified into three etiologic categories on the basis of IF microscopy: anti-GBM disease, immune complex-mediated, and pauci-immune. Our case belongs to the second category on the basis of IF study.
The morphological changes observed on LM in our case were rather deviant from the vast majority of cases of IgMN, which show either minor changes or mild mesangial proliferation.4-10 Moderate to severe degree of mesangial proliferation is rare in the reported literature.8,9 Some authors have also noted small cellular crescents in a number of biopsy specimens in IgMN.4,5 In contrast, our case showed prominent cellular crescent formation in half of the glomeruli, thus, fulfilling the criteria for the diagnosis of CresGN. Full blown CresGN has not been previously reported in IgMN in the literature.
This case illustrates the point that the spectrum of morphological changes in IgMN is wider than hitherto described in the literature. In this regard, it resembles closely IgAN, another well characterized immune complex-mediated disease, not only clinically but also morphologically, which shows the entire range of morphologic changes from minor glomerular changes to CresGN to chronic sclerosing GN.
The etiology and pathogenesis of IgMN are still unresolved. Some authors have suggested immune complex-mediated, classical pathway of complement activation leading to mesangial injury and reaction, evinced by the co-localization of C1q and C4 along with IgM in the glomerular mesangium.4,5 Others have found C1q only infrequently.8 Source of the triggering antigen is also debated.5
In summary, the present case expands the spectrum of morphologic presentation of IgMN and proves that this disease can rarely present as rapidly progressive renal failure.
Conflict of interest
The authors declare that there is no conflict of interest associated with this manuscript.
Figure 1. Medium-power view showing cellular crescents in all the glomeruli (Silver stain, ×200).
Figure 2. High-power view showing diffuse mesangial positivity of 3+ intensity of IgM in the collapsed tufts of the glomerulus on immunoflourescence (IF) microscopy. The surrounding crescent is negative (anti-IgM on IF, ×400).