Dear Editor,
One of the practical applications of estimating glomerular filtration (GF) using formulas is the possibility of being able to adapt the prescription for patients with hidden chronic kidney disease,1 thereby avoiding potential iatrogenic complications, with potential to induce hyperpotassaemia.2
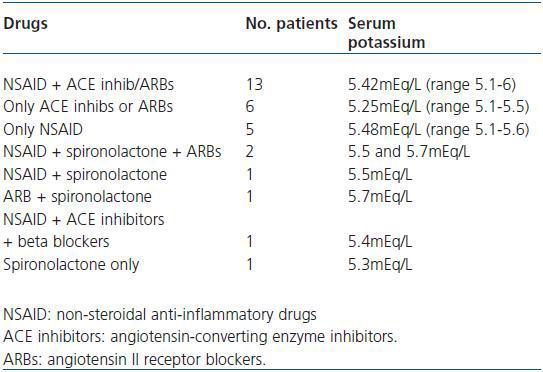
By means of a randomized sampling process, we selected a population made up of 4,014 patients over the age of 65 from the Spanish province of Huesca, who were seen in health centres with the OMI-AP IT system (Primary Care IT Organisation and Management, Stacks @), which allowed us to check the prescriptions. After excluding certain patients for different reasons, we established the GF using the abbreviated MDRD formula for 3,286 subjects. As a result, we detected 291 patients with hidden kidney failure (normal serum creatinine levels and an estimated GF < 60ml/min/1.73m2). We recorded the active ingredients prescribed by the general practitioners of 269 patients for acute or chronic conditions during a 12 month period (2007). Within this group, 211 patients (72.5%) were exposed to drugs, either alone or in combination, that could favour hyperpotassaemia. The mean serum potassium for the 211 patients was 4.553 ± 0.52meq/L (CI 95% 4.48-4.62) (median 4.6) (range 3.1-6). If we consider hyperpotassaemia3 levels above 5meq/l, the results indicate that thirty of the 211 patients presented this condition during the 12 month follow up. Table 1 shows the different drugs prescribed to these patients along with the serum potassium levels of each subgroup. The most common combination was NSAID with ACE inhibitors or ARA II. In monotherapy, NSAID were the drugs that were most commonly associated with hyperpotassaemia. Because of the design of the study, an individualised follow up of the patients was not carried out in order to determine whether there were any clinical consequences of the hyperpotassaemia. Nevertheless, the fact that this may have occurred in extreme cases should not be ruled out (seven patients had blood potassium levels of 5.7meq/l or higher).
Our study highlights the importance of correct dosage adjustment and prescription checks carried out by the professional to verify the use of certain drugs in patients with chronic kidney disease, which could remain undetected if only creatinine levels are estimated.4 Fortunately, GF estimation using MDRD has been available in our province for a few months now. In the same way that pharmacies in some hospitals in Spain issue a series of warnings when a potentially dangerous drug is prescribed to patients admitted with reduced GF, it would be good if a similar system were introduced in Primary Care. For example, currently the OMI-AP system issues a warning when doctors prescribe a drug which has been highlighted for causing an allergic reaction. Furthermore, if this system or any other IT system were able to combine the information about the patient¿s GF with the precise djustments in the handbook, it would be possible to avoid many of the consequences associated with incorrect prescriptions.
Table 1. Drug combinations that caused hyperpotassaemia in patients with ORF