Serum chloride has recently gained importance in the assessment of patients with heart failure and sepsis.1,2 In some studies, hypochloraemia has been associated with higher mortality rates.2 At the same time, the COVID-19 pandemic continues to be, to this day, a significant threat to health services worldwide. It is widely accepted that patients with cardiovascular comorbidity or chronic kidney disease are vulnerable to more severe forms of this disease.3
We carried out a retrospective cohort study. We analysed the serum chloride, C-reactive protein (CRP), procalcitonin, neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) of the 11 patients on our long-term haemodialysis programme who developed SARS-CoV-2 infection diagnosed by PCR/TMA during the second wave of the pandemic at our hospital (August-December 2020). We collected demographic data, length of hospital stay, diagnosis of pneumonia (yes/no) and the final outcome of the infection (cure or death). The median chloride level was taken into consideration as a cut-off point to divide the patients into two groups (1: ≤97 mEq/l; 2: >97 mEq/l).
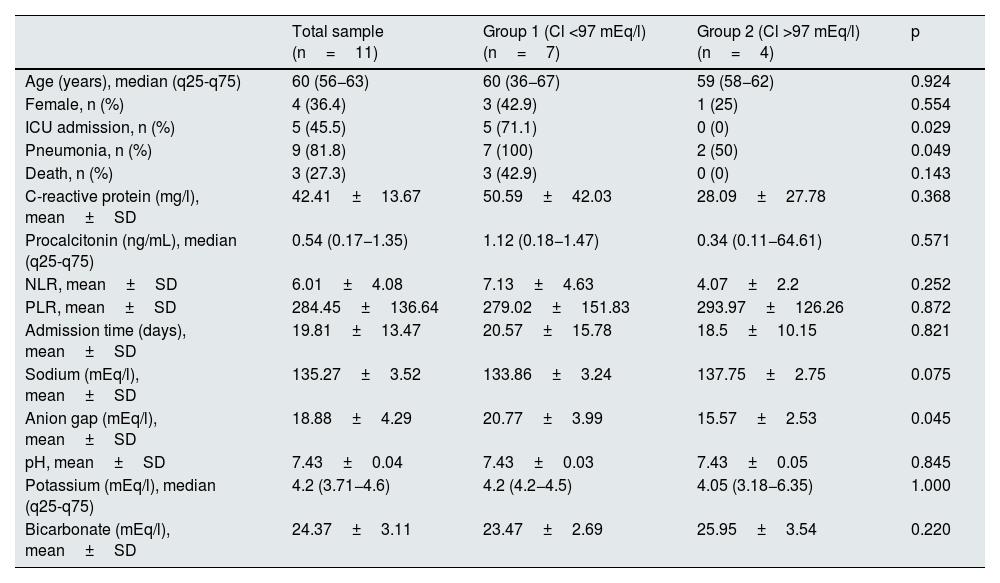
The median age was 60 years (q25-q75: 56−63); 36.36% (n=4) were female. All patients required hospital admission. The mean length of hospital stay was 19.81±13 days. Nine patients had COVID-19 pneumonia and three (27.3%) died. The median serum chloride level was 97 mEq/l (q25-q75: 94–99). The rest of the variables are shown in Table 1.
Baseline characteristics and blood test of the patients based on serum chloride levels at hospital admission.
| Total sample (n=11) | Group 1 (Cl <97 mEq/l) (n=7) | Group 2 (Cl >97 mEq/l) (n=4) | p | |
|---|---|---|---|---|
| Age (years), median (q25-q75) | 60 (56−63) | 60 (36−67) | 59 (58−62) | 0.924 |
| Female, n (%) | 4 (36.4) | 3 (42.9) | 1 (25) | 0.554 |
| ICU admission, n (%) | 5 (45.5) | 5 (71.1) | 0 (0) | 0.029 |
| Pneumonia, n (%) | 9 (81.8) | 7 (100) | 2 (50) | 0.049 |
| Death, n (%) | 3 (27.3) | 3 (42.9) | 0 (0) | 0.143 |
| C-reactive protein (mg/l), mean±SD | 42.41±13.67 | 50.59±42.03 | 28.09±27.78 | 0.368 |
| Procalcitonin (ng/mL), median (q25-q75) | 0.54 (0.17−1.35) | 1.12 (0.18−1.47) | 0.34 (0.11−64.61) | 0.571 |
| NLR, mean±SD | 6.01±4.08 | 7.13±4.63 | 4.07±2.2 | 0.252 |
| PLR, mean±SD | 284.45±136.64 | 279.02±151.83 | 293.97±126.26 | 0.872 |
| Admission time (days), mean±SD | 19.81±13.47 | 20.57±15.78 | 18.5±10.15 | 0.821 |
| Sodium (mEq/l), mean±SD | 135.27±3.52 | 133.86±3.24 | 137.75±2.75 | 0.075 |
| Anion gap (mEq/l), mean±SD | 18.88±4.29 | 20.77±3.99 | 15.57±2.53 | 0.045 |
| pH, mean±SD | 7.43±0.04 | 7.43±0.03 | 7.43±0.05 | 0.845 |
| Potassium (mEq/l), median (q25-q75) | 4.2 (3.71−4.6) | 4.2 (4.2−4.5) | 4.05 (3.18−6.35) | 1.000 |
| Bicarbonate (mEq/l), mean±SD | 24.37±3.11 | 23.47±2.69 | 25.95±3.54 | 0.220 |
ICU: intensive care unit; NLR: neutrophil-to-lymphocyte ratio; PLR: platelet-to-lymphocyte ratio; SD: standard deviation.
When these variables were compared based on chloride levels, significant differences were found only in the anion gap value (p=0.045). There were no significant differences in terms of inflammation parameters, pH, sodium, potassium and bicarbonate.
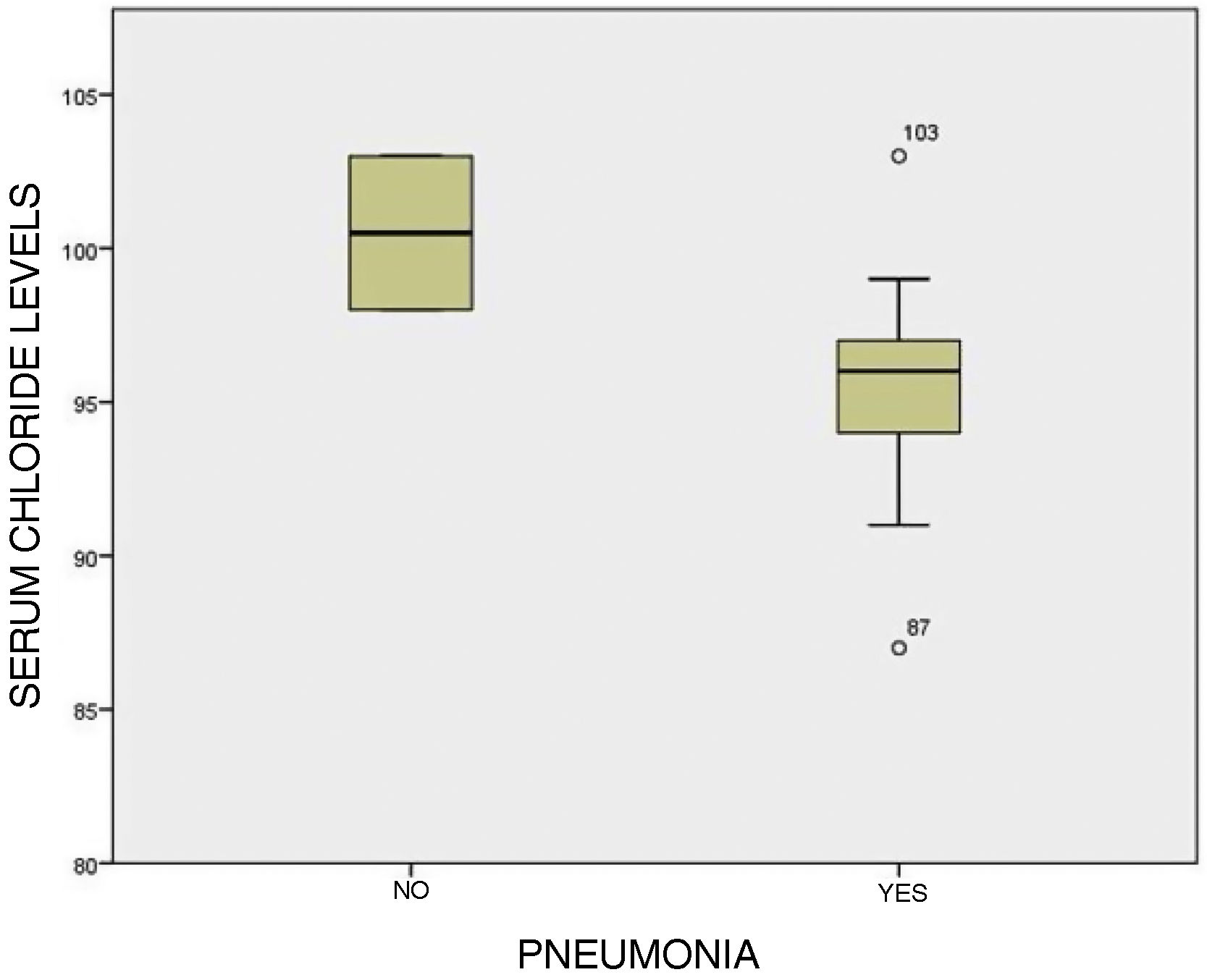
Group 1 (serum chloride ≤97 mEq/l) had a higher incidence of pneumonia (p=0.049) (Fig. 1) and a greater tendency to be admitted to the intensive care unit (p=0.029). Moreover, despite not reaching statistical significance, a higher mortality rate was evident in the group with lower chloride levels.
Patients on long-term haemodialysis have been particularly affected in this pandemic.3 To our knowledge, this is the first study that focuses entirely on patients on long-term haemodialysis and the possible utility of serum chloride levels at hospital admission for COVID-19. There are currently a number of studies showing a tendency in patients positive for SARS-CoV-2 to have lower serum chloride levels.4 Additionally, a recent cohort of patients hospitalised for COVID-19 shows that a 26% of patients had hypochloraemia, with this being more common in patients on haemodialysis.5 In addition other cohorts show that median serum chloride was significantly lower in patients with severe disease.6,7
Hypochloraemia is a prognostic marker of heart failure, even more powerful than sodium levels, due to its influence on neurohormonal activation and resistance to diuretics.1 However, this would not fully explain its role in the pathophysiology of COVID-19.
The possible influence of endothelial dysfunction within the pathophysiology of COVID-19 has been documented,8,9 and in some recent studies chloride has been linked to endothelial dysfunction through some ion channels.10 In our study, the median NLR, an emerging marker of inflammation, endothelial dysfunction and prognosis in COVID-19,3 was higher in patients with hypochloraemia. However, these results were not statistically significant due to the small size of the population studied.
It would be reasonable to think that the anion gap influences the results. However, in our analysis all the other variables involved in the anion gap formula (sodium, potassium and bicarbonate) did not show significant differences between groups, and this finding is therefore attributable to serum chloride itself.
In conclusion, in the absence of further studies, long-term haemodialysis patients with SARS-CoV-2 infection and lower serum chloride levels at hospital admission could have a greater tendency to develop pneumonia and require admission to the intensive care unit.