To the Editor,
There is a growing interest in home haemodialysis (HHD) both in Spain’s neighbouring countries and in the United States. This interest has arisen out of the limitations of the conventional three-weekly therapy sessions, shown in studies such as HEME1, in order to increase the survival of stage 5 chronic kidney disease patients. There is an increasing number of publications that back home therapies in terms of quality of life2, blood pressure management, reduction of left ventricular hypertrophy, calcium-phosphorus control, anaemia, nutritional state and lower morbidity and mortality4,5, when compared to classic treatment plans; there are also studies supporting this treatment for its reduction of costs6.
For this reason, we think it opportune to present our experience in implementing a short daily HHD programme. Between March 2008 and November 2013, we included 10 patients (3 in 2008, 0 in 2009, 1 in 2010, 1 in 2011, 4 in 2012 and 1 in 2013); 50% were females, with an average age of 61 (range: 38-81), distance to the centre 42 km (range: 0-122 km) and remained in the technique for 32 ± 17 months. As regards the origin of the patients: five came from outpatient consultations, three were on peritoneal dialysis and two from a peripheral centre. In terms of the programme exits, there were two deaths and two transplants. No patient required a change of renal replacement therapy and there were no losses in the training period.
In terms of morbidity, we had two hospitalisations in 2008, one in 2009, two in 2010, none in 2011, one in 2012 and six in 2013 (we should point out that half of the hospitalisations were scheduled). The reasons for admission were: three cardiovascular, two infectious (associated with vascular access, in 2008 and 2010), one neoplasia, one digestive, two due to vascular access of non-infectious cause (insertion of tunnelled catheter and closure of fistula aneurysm) and three due to other causes (scheduled nephrectomy, herniorrhaphy and clinical deterioration).
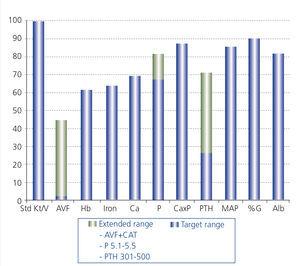
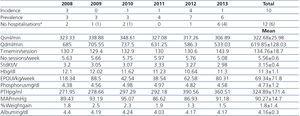
The prescribed haemodialysis plan and the results obtained are presented in Table 1 and Figure 1.
Regarding drugs, we used:
- Antihypertensives: 43% did not require any antihypertensive drug, 53% required one drug, and only 4%, two or more.
- Phosphate binders: the use of a binder was not required in 47% of the monthly checks; only one type of binder was needed in 35% of cases, predominantly calcium over non-calcium based binders; while a combination of various types of binders was required in the remaining cases. Although the average calcium carbonate dose used initially was high, 3829.8mg/day, there was subsequently a progressive substitution for calcium acetate, averaging 815.16mg/day. The other binders used were: aluminium hydroxide 77.66mg/day (one-off use and not used at present), 2478.83mg/day of sevelamer and 909.66mg/day of lanthanum carbonate.
- Calcimimetic or vitamin D analogues: their use was not required for controlling parathyroid hormone values in 15% of cases; only paricalcitol was used in 40% of cases, cinacalcet in 21%, and a combination in the remaining cases (24%). The average cinacalcet dose used was 28.9mg/day, and 3.84µg/week of paricalcitol.
- EPO: average dose was 69.34±71, 85UI/kg/week.
It must be highlighted that we did not observe any microbiological or chemical contamination in the checks carried out. In terms of technical complications, it must be noted that when dialysis treatment could not be carried out on the planned day, the patient took an un-planned break or went to hospital, on three occasions; we believe this fact to be anecdotic considering that more than 6000 sessions were undertaken in the study’s period.
The results obtained in clinical-analytical and morbidity and mortality terms surpass, or are at least comparable to, the standard quality of care objectives, with no incidences observed in relation to the patients’ safety. In addition, the technique has enabled a considerable improvement in patients’ quality of life. For these reasons, we consider that the patient has a right to the option of HHD, and therefore it is our duty to offer it. We believe that to do so, we must broaden patient selection criteria, not being led by preconceived ideas and strengthening the physical substrate in order to implement these programmes.
Figure 1. Percentage of the quality indicators obtained.
Table 1. Description of the results